Learning Objectives
This is an intermediate level course. After completing this course, mental health professionals will be able to:
- Define cultural efficacy.
- Identify components of cultural humility.
- Describe three dimensions of Falicov’s model, Multidimensional Ecological Comparative Approach (MECA).
- Discuss elements of a culturally informed clinical assessment, diagnosis and treatment plan.
- Explain intersectionality and its role in mental health treatment.
- Discuss role and use of cultural adaptations in evidence-based treatments.
The materials in this course are based on the most current information and research available to the authors at the time of writing. The field of multicultural psychotherapy is growing exponentially, and new information may emerge that supplements these course materials. This course material is designed to equip practitioners with a comprehensive understanding of multiple cultural identities, practice parameters, and the strengths of effective practice as well as an understanding of the potential harm inflicted on clients by less-than-competent practice. It is possible that reading about lack of awareness of multicultural factors could be triggering but those effects could be assuaged by enhanced knowledge of positive strategies for practice of effective clinical multicultural psychotherapy and by clinical consultation.
Outline
- Introduction
- Are We Culturally Efficacious?
- Guidelines For Multicultural Practice
- All Therapy and Practice Is Multicultural
- Defining “Cultural Competence”
- Training
- Graduate Training In Multicultural Practice
- Multicultural Competence
- Identities and Perspectives
- Race
- Immigration
- Socio-Economic Status and Social Class
- Language
- Religion and Spirituality
- Disability
- Intersectionality
- The Impact Of Covid
- Cultural Humility
- Cultural Formulation
- Intersectionality
- Identities
- Falicov’s MECA Theory
- The MECA Framework Includes
- Migration and Uprootings
- Ecological Context
- Family Organization
- Family Life Cycle
- Reflections
- Migration and Uprooting
- Ecological Context
- Family Organization and Family Life Cycle
- Psychotherapeutic Relationship: Strains and Ruptures
- Possible Avenues For Multicultural Interventions
- Additional Considerations - Lenses
- Cultural Countertransference
- Navigating Privilege and Oppression
- Addressing and Resolving Conflicts
- Self Awareness
- Cultural Biases: Confirmation; Implicit Bias
- Microaggressions
- Identities and Intersectionality
- Racial and Ethnic Diversity Trauma
- Dealing With Racism-Related Stress and Racial Trauma When Working With Clients Of Color
- Social Justice
- International
- Multicultural Theoretical Orientations
- Treatment Considerations
- Summary
- References
Introduction
In the ever-changing landscape of
society’s racial and cultural diversity, it is imperative that mental health
providers are equipped with the tools and knowledge to best serve diverse
groups. Having foundational knowledge of theories and concepts of
multiculturalism is critical in providing quality and effective psychotherapy.
Using a multicultural lens assists therapists in recognizing and valuing the
diversity of human experiences and the multiple ways that cultural factors can
influence an individual's thoughts, emotions, and behaviors and thus impact
psychotherapy.
The most frequent and
strongest predictor of client outcome is the therapeutic relationship. Thus,
establishment of the therapeutic alliance and identification and management of
countertransference or emotional reactivity are central factors. Apropos to the
relationship are the identities of each participant – client(s) and therapist(s) – assumptions
each makes about the other, openness to the individual cultural diversity
factors of each, self-perceptions, and perceptions and behaviors toward
clients. Therapist openness to client cultural beliefs, values, perspectives,
strengths, and resources, as well as empathic relating, are central to all
therapy. Therapist self-knowledge and awareness of personal identities, biases,
and worldviews enhance the therapeutic process. How a therapist approaches
multicultural factors, ethnicity, race, power, and privilege pave the
foundation and formation of the relationship. Interpersonal processes,
identifying and addressing strains, enhancing mutual understanding, and
initiating problem-solving all inform the therapy. There are many aspects that
can inform and strengthen the bond, enhance collaboration, and make for a respectful
process that facilitates treatment; similarly, some may hinder, feel unjust or
oppressive, or be lacking in empathy.
Therapists who
are trained in multiculturalism are better prepared to tailor treatment and address
the unique needs of clients from diverse cultural backgrounds. A better
understanding of cultural norms, values, and beliefs can influence clients' attitudes
toward mental health, help-seeking behaviors, and treatment preferences. Appropriate
multicultural training also creates opportunities to better recognize the
clinician’s own cultural biases that can impact their work.
In this program, key aspects of
multicultural psychotherapy are identified, contextualized in terms of
current research and analysis, and strategies are suggested to enhance
efficacious practice.
Are We Culturally
Efficacious?
Are
cultural identities a major factor in treatment? In a recent study it was shown
that although therapists may consider themselves culturally self-efficacious,
they generally do not even minimally address sociocultural factors or
background (Wilcox, Franks, Taylor, Monceaux, & Harris, 2020).
There was a
failure by a substantial proportion of participants. Therapists who perceived
themselves to be culturally efficacious did not even minimally address clients’
sociocultural context, demonstrating a significant disconnect between
self-perception and self- report and actual performance. Further, therapists
demonstrated denial of privilege and of oppression, simply suggesting that
sometimes dominance of some occurs. Further, tendencies toward
perspective-taking and possessing “just world” beliefs were associated with
multicultural competence. (Wilcox et al., 2020). So, a critical take-away is to not simply self-assess cultural efficacy generally but rather to consider
specific components and behaviors that comprise such efficacy.
It is also
important for the clinician to be self-aware of one’s cultural frame and
behaviors as one conducts clinical work. Our self-assessment is often not as
accurate as we believe it to be, and often differs markedly from observer
ratings. With this information, self-assess how often you use multicultural
case conceptualization. Specifically, to what extent are culture and context
significant components in your case conceptualization.
Given the important premise
that all clinical practice is multicultural, clinicians need to have
specific strategies to imbue their worldviews in their thinking,
conceptualizations, treatment planning, interactions, and relationships. Both
clinical practice and clinical supervision are cultural encounters (Falicov,
2014).
How does one strengthen one’s
multicultural practice acumen? Concern has been expressed about impact on
clinicians of the devaluation of field practicum and the disconnect between
academia and the field experience (Giddings, Cleveland, & Smith, 2007),
potentially leading to inadequate or harmful clinical practice. Substantial
evidence of the existence of harmful supervision during the training trajectory
has been revealed (Coleiro, Creaner, & Timulak, 2022) after Ellis et al.’s
(2015) shocking finding of high rates of inadequate and harmful clinical
supervision during the training trajectory. And if harmful clinical supervision
occurs, it will directly and adversely impact clinical practice. Note that in
harmful supervision, both clients and supervisees-in-training are harmed.
Guidelines for Multicultural Practice
It is critical for
practitioners to be prepared to approach multiculturalism intentionally and
systematically as a part of practice and to have requisite knowledge, skills,
and attitudes to initiate and maximize efficacy of the cultural encounter in
the frame of multicultural practice. A first step is to consider the concept of
worldviews.
Worldviews are sets of
attitudes, beliefs, assumptions, stories, expectations about the world and
social realities – and these inform our every thought and action. They impact
what we attend to, how we respond, and our attitudes and behavior toward
clients and our clinical work. As a clinician, it is critical to be self-aware
and open to input and consideration of how our own early life experiences and
identities form our expectations and behavior toward clients. From the very
onset of the therapeutic experience, our presentation (and if under
supervision, the supervisor’s as well) including attitudes and behavior, set
the frame for clinical work and relationship. Openness, supportive quality, and
empathy are essential ingredients. The depth and breadth of our worldviews set
the stage for our clinical practice.
When the American
Psychological Association presented revised multicultural guidelines (2017),
they refocused on efforts to address systems-level change rather than
traditional approaches to individual-level change. Thus, multiple populations’
historical experiences including power, privilege, and oppression were to be
addressed systemically, and attention to be focused on macro levels including
racism and multiple other isms (i.e., sexism, racism); also societal
structures: economic, educational, access to adequate culturally relevant
health care, as well as social and community contexts, all addressing both
health and healthcare disparities and access. This shift in focus to
systems-level approaches has been slow to reach the mental health communities.
Think about a client you are
currently working with or worked with previously. Before you met them for the
first time, consider how a combination of your brief information from the
client and your own life experience influenced your thoughts about how the
client would present for the first session. Reflect on how accurate your
expectations were. And think about what factors were operative in your thoughts
about how they would present. Examples could be previous clients, referral
question(s), phone screening information, and assumptions based on all of
those.
To further reflect on these
concepts, let’s review the following example.
Consider an adolescent who was referred for depression. The 14-year-old girl was not
eager to be in therapy, but her mother insisted. The therapist was unsure how
to deal with a reluctant client but began by encouraging her to identify what
was going well for her. The therapist wanted to identify three goals but the
youth was non-responsive and said therapy was “stupid.” Then the therapist gently
asked her about school and home. The client disclosed that she was at a new
school and kids at this school were really different from her. The therapist
encouraged her to talk about how they were different, and the client
said that she is Latina and most of them are not. The therapist explored that with
her, and discussion turned to her break-up with her boyfriend, worry about her
grades, annoyance with her brother, worry about her upcoming birthday, her
grandmother’s efforts to control it, and her feeling overwhelmed. She started
to say “quince …” and then stopped and asked the therapist if she even knew what
a quinceanera was. The therapist did, asked her a few questions about her many
preparations for it, and then encouraged the client to tell her specifically
what her worries were. Further discussion resulted in identifying several goals
for treatment, both immediate and longer-term ones, as they related to both the
celebration and her worries about school performance, isolation, and lack of
friends in her new school. The client asked the therapist how she knew so much about
“quince” and the therapist told her she had gone to school with several girls
growing up who had had one.
All Therapy and
Practice is Multicultural
Generally, in training
therapists studied “multicultural competence” in preparation for conducting
excellent therapy and assessment. Increasingly, concern turned to the inference
by some that “competence” was perceived as an endpoint one could achieve and
thereafter remain confident in one’s knowledge without ever learning anything
more. However, it is increasingly clear that there IS no endpoint and that the
components of “competence” – knowledge, skills, and attitudes – are ever-evolving,
and that there is no end to learning, experiencing, understanding, relating,
and integrating.
Next, researchers turned to
Multicultural Orientation (Owen, Tau, Leach, & Rodolfa, 2011), referring to
philosophy, values, and beliefs about the importance of multicultural factors
including racial and ethnic identities, and the clients’ cultural background in
the context of those of the therapist, and how one integrates all of those into
the conduct of assessment and intervention with the client(s). Importantly,
attention was focused on not simply knowledge, but on attitudes and skills.
These are essential, as therapy is anchored in relationship – which is comprised
of the working alliance, the “real” relationship, and
transference/countertransference or emotional reactivity, and is anchored in collaboration, which implicitly requires goals and tasks for therapy shared between the client
and therapist and requires therapist genuineness. When clients viewed their
therapist’s multicultural orientation positively, the therapist was perceived
to be more believable and credible, and client psychological wellbeing was
viewed to be more positively impacted. However, the results were not uniform
across various client ethnic and racial groups.
Defining Cultural Competence
While there is agreement
about the role and importance of considering culture in assessment, diagnosis,
and treatment, there remains a challenge in coming to consensus on defining
exactly what “cultural competence” is and how to achieve it in psychotherapy. A
2010 literature review that compared the various conceptualizations and
definitions of cultural competence across varied disciplines in healthcare
including psychology and social work found a lack of consensus regarding an operationalized
definition or concept of cultural competence. The review revealed that across
the varied models of cultural competence there was disparate emphasis on what
was considered to be the essential components of multicultural counseling.
Across the different models
of cultural competence, the authors did however identify four common themes
that can be used to develop a framework for providing effective clinical
services with clients of diverse cultures and backgrounds:
1)
awareness of one's own cultural beliefs and biases;
2) understanding of the client's cultural background;
3) knowledge of culturally appropriate interventions; and
4) development of cross-cultural skills.
Any therapist preparing to
work with diverse populations should prepare themselves to gain knowledge and
awareness across these four domains (Huey, et al., 2010).
Knowledge, skills and
attitudes are relevant and essential. Knowledge and understanding of one’s
personal biases, privilege, and assumptions; recognizing, respecting, and
honoring clients’ worldviews through inference and action; and being responsive
and aware of clients’ worldview and realities are all essential. Attitudes may
be implicit. Thus, engaging in reflective practice, ongoing training and
supervision, and being open to feedback and self-reflection with respect to
metacompetence (openness and thoughtfulness about what one knows and does not
know), self-critiquing, and being genuinely open to input and feedback – even
though it may be difficult to hear – are all essential components of effective
multicultural practice.
And remember there is NO
ENDPOINT to cultural competence: It is evolving and changing with experience
and with new knowledge, skills, and attitudes.
Training
Graduate Training in Multicultural Practice
Generally, attention to multicultural
competence and cultural humility in graduate training may have been limited and varied as a function
of when and where one received their training. Collins, Arthur, Brown, &
Kennedy (2015) studied student perspectives on graduate training in
multiculturalism and social justice. They identified competencies
facilitated and those in which barriers were encountered. Facilitated were:
- Developing
a culturally sensitive relationship that included accepting and respecting
cultural differences, inquiry about client’s culture, critical nature of
building a trusting environment, identifying and balancing power differentials;
- Awareness of others’ culture, balancing curiosity with respect;
- Building a trusting environment while respecting client worldview and working
collaboratively with them to achieve outcomes, as clients are the experts on
their culture and personal issues; and
- Awareness and need to balance power
differentials and not imposing personal worldviews and realities on clients
which precipitate relationship ruptures.
They described the process of
relationship-building scaffolded from their own understanding of their own
personal biases, privilege, and cultural assumptions and honoring clients’
worldviews. Barriers were student personal, interpersonal, or contextual
factors that blocked or interfered with facilitating factors. These included:
- Student lack of willingness or interest often predicated on previous negative
experiences;
- Resistance to acknowledgement of privilege or bias;
- Holding incompatible
values or views such as not being able to combat learned helplessness of
clients or disapproval of clients refusing some aspects of treatment; and
- Lack of
competence in general regarding cultural issues, powerlessness in the system, an
oppressive or discounting system or administration, or lack of resources.
Critical
questions include how to create a training environment of cultural humility? How
do each of us model reflection, acceptance, and openness to acknowledging our
own privilege, bias, and worldviews – and how do we demonstrate this in our
clinical practice?
Also, whose
perception counts? In a meta-analysis, client perceptions of multicultural
competence correlated with client outcomes, but therapist self-perceptions of multicultural
competence did not (Soto, Smith, Griner, Rodriguez & Bernal, 2018). They
described the use of cultural adaptations including holistic/spiritual
conceptualization of wellness and engaging in cultural rituals. Areas of
cultural adaptation included: language, use of and content of metaphors,
general content, goals, methods, and the context. Consider your own use of
cultural adaptation and how you enact it. Examples include respectful inquiry
about cultural meaning, spirituality in the context of the presenting issues or
solutions, harmony, and reflective practice including indicating if the
therapist does not understand a concept or practice. However, likely as a
result of their level of acculturation, children benefit less from cultural
adaptations (Huey & Polo, 2008).
It is suggested
that although therapists cannot be competent in every client identity or
attribute, they could be aware of, open to, and attempting to adapt treatment
to align with the salient intersecting identities, those valued most by the
client (e.g., religious, culture-specific) (Soto et al, 2018).
Another question
is how accurate is one’s own self-assessment? And how effective is one
multicultural course without integrated supervision and ongoing support?
Self-assess on your own training during the graduate trajectory and consider
the strengths and barriers presented above as well as the evolution of practice
and research in the past decade. Remember that your own active efforts to
self-assess enhance your self-knowledge and thus your competence.
Multicultural
Competence
Recognition must
exist that there are multiple factors in the provision of multiculturally
relevant therapy. This includes knowledge, skills, and attitudes. Provision of
therapy and assessment in a respectful, knowledgeable, and culturally competent
manner are essential. There is significant recognition that psychotherapy must
be culturally competent and occur through the lens of cultural humility. However,
clinicians may find themselves unclear or challenged to do so. Examination of
one’s attitudes, beliefs, skills, knowledge, and previous life experience is
imperative. Considering one’s assumptions about therapy, therapeutic
relationships, psychotherapy models, multicultural psychotherapy, values, and
biases are all essential.
Consider the
grounding principles of the APA’s Guidelines on Race and Ethnicity (APA, 2019):
articulating the critical and ubiquitous influence of ethnicity, race, and
related issues of power and privilege with the understanding that social
justice is inherent to racial and ethnocultural responsiveness. It is essential
for clinicians to be self-aware and proactive in discussion of race and racial
identity. This includes attending to power differentials related to race in
professional interactions and in relationships, minimizing detrimental effects
of unconscious, implicit bias. Race and ethnicity are sources of meaning and
context. Some possible steps provided in the guidelines are:
- modifying intake forms to address more complex meanings and
understandings of race, ethnicity, and intersectionality;
- regularly considering the racial and ethnic climate of the setting; and
- developing procedures to ensure that racial and ethnocultural influences
are directly addressed.
When race is
avoided, the avoidance interferes with relationships, promotes social distance,
and may be inferred to be (or is) implicit bias or implicit prejudice or
represents a set of negative attitudes. These may be manifest as social
distance, presumed prejudice, implicit attitudes, micro or macroaggressions
that are expressed or experienced, and internalized racism. Implicit bias is
automatic and unintentional, and results in assumptions, preferences,
aversions, or behavior that results in (unintended) assumptions and actions.
For example, when a therapist is more affiliative and responsive to someone
with a common name rather than a less usual name that may be associated with a
particular ethnicity, or making assumptions about a group or individual based
only on race. All of these prevent connection and harm the therapeutic
relationship. Race and ethnicity are also associated with experiences of
oppression, privilege, and power. Avoidance of the topics may lead to
assumptions of disrespect and generally undermine relationship and the
framework of social justice and fairness.
The first of these APA
guidelines (2019) is to “strive to recognize and engage the influence of race
and ethnicity in all aspects of professional activities as an ongoing process”
(Guidelines, APA, 2019, p. 9). With value attached and recognition of
importance, the clinical guideline sets the stage for discussion and mutual
understanding. Guidelines three and four entail striving for awareness of own’s
own positionality (and identities) with relation to ethnicity and race, and
addressing social inequities and injustices.
Proactive discussion includes
engaging in reflective practice including exploration of worldviews and social
positions, all of which are impactful on the presenting problem and the therapy
that ensues. Thus, it is imperative that clinicians continuously engage in
learning about these aspects of culture.
Identities and Perspectives
Race
Black persons are more likely
than Hispanics or Asians – and much more likely than White persons – to say
that their race is central to their identity. According to the Pew Research
Center, about three-quarters of Black adults say being black is extremely or
very (74%) important to how they think of themselves; 59% of Hispanics and 56%
of Asians say being Hispanic or Asian, respectively, is important, and about
three-in-ten in each group say it’s extremely important. In contrast, just 15%
of Whites say being white is very or extremely important to how they think of
themselves.
(pewresearch.org/social-trends/2019/04/09/race-in-america-2019/)
Racial and ethnic identity
thus are central to all aspects of self, although the extent is variable;
discrimination and racism negatively impact mental health processes and
outcomes. Race itself is complex, as it is a social construct that relates to
skin color, facial features, hair texture, and body shape (Harrell &
Sloan-Pena, 2006).
BIPOC (Black and Indigenous
People of Color) individuals are less likely to seek therapy, and when they do,
they are more likely to terminate therapy early (Owen et al., 2017). The
multicultural competence model proposed that therapists are expected to learn
culturally relevant knowledge, be open to challenge their own beliefs regarding
marginalized populations (awareness) and use culturally sensitive interventions
and skills.
Research has revealed that
when race or racism comes up in therapy, regardless of their own race
therapists often respond to BIPOC clients with denial, avoidance, or other
signs of cultural discomfort. Specifically, when Black clients bring up anti-Black
racism in session, particular responses occur. Bartholomew and colleagues
identified four such possible therapist responses:
(a) wanting
to move beyond strict acknowledgment to ensure acknowledgement of pain and
affirmation of experience;
(b) being present in the moment and drawing personal awareness into that moment;
(c) turning inward and engaging with one’s own emotional responses including
empathy with those experiences; and
(d) I am versus I should: proactive and reactive comfort including recognition
of pain and reacting to it authentically.
Therapist comfort is an
essential aspect that increases the likelihood such disclosure and discussion
occur. More specifically, therapists’ level of cultural comfort when discussing
anti-Black racism with Black clients may be based on their own racial
experience or emotions linked to personal racial beliefs, identities, and their own
life experience growing up (Bartholomew et al., 2021).
Use of the concept of the
ecological niche (Falicov, 2014) – consideration of multiple cultural locations
and their intersectionality – is useful in addressing client and therapist
identities. Harrell (2014) suggested considering familial and community racial
socialization including the salience of race, how much identification with the
racial group exists, meanings, beliefs, and judgments about race. Even if
client and therapist share the same racial group, intersectional multicultural
identities need to be factored in. Misunderstandings may occur if one minimizes
race or alternatively excludes other identities and factors, focusing only on race.
Harrell (2014) suggests ongoing reflective practice in order to understand the
multiple layers of sociopolitical, interpersonal, and intrapersonal meaning of
race for the individual and their family, regarding the referral question and
the context.
Immigration
Migration is often a
neglected multicultural consideration. At least 13.6 percent of the U.S.
population is comprised of immigrants (Migration Policy Institute, 2023).
However, generally, it is seldom discussed in clinical practice or in clinical
supervision. Falicov (2014) highlighted the complexity of experiences in
immigration, and the impacts that are often longstanding and profound. She
urges consideration of preimmigration, migration, and postmigration
considerations in the psychosocial assessment of clients. Further,
intersectionality with socioeconomic status, race, gender, gender identity,
age, generation, and developmental status at immigration; country of origin
(and its proximity, reason for migration including trauma); the process of
immigration, whether voluntary or forced; internal or refugee status, impacts,
and current immigration status should all be considered as well. Also important
is connection with family and friends in the country of origin through
telecommunication. Falicov urges a strength-based approach, considering losses
in the context of resilience, gains, and triumphs. She also emphasizes cultural
humility and intersectionality in a social justice frame.
Understanding family and
individual specific stressors, coping, and strengths is essential. Falicov
distinguishes between coaxed and unprepared migrations, those that were planned
and those that were very much in response to an event, often traumatic. Some of
the general issues to be discussed include a genogram of family in the U.S. and
in the home country, relationships, and emotional responses, losses, including
of employment, professional, or educational status, how family members are
learning the new language (which may rely on children who are learning the new
language at school and thus are potential translators for the family),
migration narratives, and whether children and family members are aware of any
or all aspects of the above.
Falicov uses the MECA (Multidimensional Ecosystemic Comparative Approach )
framework including ecological context (e.g., living conditions, school access,
limits on upward mobility, financial stressors, physical, psychological, and
cultural trauma), family life cycle (e.g. loyalty to family of origin, losses
of other generational influence, support), migration/acculturation status
(legal status, language acquisition and fluency), and family organization
(bonds with family members locally in in country of origin, family hierarchy
changes precipitated by migration including employment, roles, language
fluency). Further, Falicov describes interventions and therapist roles as a
function of stage of migration. Initially, the therapist deals with crises, and
helps to address and sometimes restore ecological order within the family. An
important aspect is engaging in self-reflection – by the therapist (and the
supervisor if there is one) to deconstruct and contextualize through the lens
of the personal experience of immigration of each.
Thus, it is essential for the
therapist to be self-aware of the impact of their own life experience (or
influences on their perspectives on immigration and acculturation) on their
clinical work with the family. Examples include a therapist who shares language
fluency with the family, although bearing in mind that language fluency does
not imply cultural competence or complete understanding of the client
experience. In addition to language, consideration of religion, spirituality,
family dynamics, ethnic identity, perception of and aspects of discrimination,
and understanding causal factors leading to illness, all viewed through a frame
of cultural humility, respectful caring, and strength-based approach.
In cases of forced migration,
an involuntary displacement and a crisis and upheaval of life expectations with
resulting barriers and stigmatization, cultural humility is essential (Adams
& Kivlighan, 2019). A high frequency of misdiagnosis and misunderstanding
occur when addressing the general physical and psychological consequences of
such migration that occurs generally with no warning or preparation.
Sensitivity to cultural and situational aspects of emotional expression,
exploration of harassment and prejudice, dynamics of resettlement and emotional
impact, and general empathic responding are essential.
Socio-economic Status
and Social Class
Socio-economic status and
social class include not simply income but educational attainment, financial
security, and subjective considerations, as well as one’s own and others’
perceptions of economic status, social status and social class. Social class is
more than income, education and occupation, and includes economic resources,
education, and occupation as well as prestige and power (summarized in Fouad
& Chavez-Korell, 2014). The APA guidelines for psychological practice for
people with low income and economic marginalization address economic
marginalization (APA, 2019).
In their resolution on
poverty and socio-economic status (SES), the American Psychological Association
(2023) identified the increasing gap between upper and lower SES, the
devastating personal and financial repercussions of the confluence of COVID and
an economic downturn, and the devastating impact of the intersection of low SES
and multiple minoritized identities, historical and systemic discrimination,
biased laws and resultant economic inequality. The resolution includes a
summary of the current research on the impact of poverty, intersections with
multiple identities, and impact on human rights. Economic marginalization
results in limited access to supports, resources, and opportunities in life,
which limit educational, physical and mental health, achievement, and general
quality of life.
Understanding not simply the
status or the economic numbers, perhaps represented by fees, but the need for
mental health providers to approach these with cultural humility, the therapist
needs to frame impacts on the presenting problems and on the possible treatment
options, to address specific needs.
Language
Over 350 languages are spoken in the U.S. according to the
2018 U.S. Census. A challenge to mental health is providing competent services
to those who seek them. 41 million people spoke Spanish at home. Even if the
therapist “speaks” Spanish, they may find they are less equipped to deal with mental
health issues or the language specific to those. Bilingual services are
severely underrepresented and much needed.
For example, it is
important to know that both therapists and clients report reverting to their
native language for emotionally intense disclosures or discussions, often
referred to as “code-switching” or “language switching” –especially if the
memories were encoded in the native language.
Valencia-Garcia and Montoya
(2018) state that although the need for bilingual therapists is acute, there is
still inadequate training – even though the U.S. census predicts 30% of the
population will be Latino by 2050. Common errors are assumptions that if a
supervisee or therapist has a Spanish surname, or says they speak “some”
Spanish, that they will be fluent and able to conduct therapy bilingually in
Spanish or any of the approximately 400 languages spoken in the U.S. Professional
fluency is distinct from conversational fluency. Further, a very small minority
of bilingual therapists have received bilingual supervision during their
training
A result is that ethnic and
racial minority students who are bilingual find themselves carrying the burden to
provide therapy in a language other than English with no training in therapy or
assessment in their native language or language they have studied, nor have
they been supervised either in the client language or by a bilingual
therapy – often due to the fact that the student is the only person on the staff
who speaks the language of the client. Or a translator is provided who is a
family member or office worker who has no training in translation and no
clinical training to understand relevant communications or to translate them
accurately, and may have significant emotional response or involvement in the
family situation. This is an area of significant concern and deemed essential
for ethical outcomes.
Having a shared language is
generally a great strength for therapeutic rapport, but bilingualism should not
be viewed as synonymous with cultural competence or knowledge and attitudes,
but it is clearly a great strength. Consultation is indicated and essential
when conducting evaluations (often high-stakes) or interventions to understand
culture and nuance. The value of bilingual therapy with Latino clients was
studied. Bilingual therapy was associated with:
(a)
Enhanced expression and understanding;
(b) An affirmative experience;
(c) Facilitating therapeutic processes;
(d) Utility of a therapist bilingual orientation, and;
(e) Strengthening the therapeutic relationship (Perez-Rojas et al., 2019).
Religion and Spirituality
Although often neglected or
frankly ignored by therapists, religion and spirituality shape personal
experience and are an essential aspect of worldview. They may also be a source
of strength, comfort, and hope. Or may be a source of distress, negative affect,
or anger (Vieten & Lukoff, 2022). However, these subjects are rarely
discussed or addressed in training or in clinical practice. Self-awareness and
-appraisal are critical for clinicians: considering one’s own faith commitment
and attitudes toward religion and spirituality. Gallup polls reveal that the
vast majority of the U.S. population report religion is “very or fairly”
important; in contrast, mental health professionals may view religion as much
less important (Shafranske, 2016).
Approaching religion and spirituality with an attitude of respect and openness
and competence is a professional competence, and neglecting to do so reflects a
deficit in cultural competence (Vieten & Lukoff, 2022). Vieten and Lukoff
(2022, p. 32) described and proposed 16 religious and spiritual competencies
for clinical practice. Attitudes and beliefs included demonstrating empathy,
respect, and appreciation for clients from diverse spiritual, religious or
secular backgrounds and affiliations; having awareness of how one’s own
spiritual and/or religious background and beliefs may influence their clinical
practice; and attitudes, perceptions, and assumptions about the nature of
psychological processes. Knowledge includes knowing that diverse forms of
spirituality and/or religion exist, and exploring spiritual and/or religious
beliefs, communities, and practices. Skills include helping clients explore and
access their own spiritual and/or religious strengths and resources.
Expanding upon cultural
humility through the lens of religion and spirituality, Davis and colleagues
add essential components of therapist civility, a neglected aspect, with
empathy, an affective stance. It includes openness; willingness to recognize
and explore different beliefs and perspectives; awareness of one’s own values,
beliefs, worldviews, strengths, and areas in development; an egalitarian
worldview; openness to diversity and differences, including in values and
self-reflective capability; awareness and proactive responding to inequality
and prejudice (Davis et al., 2021). An important aspect is how clients perceive
their therapists’ cultural humility toward religion and spirituality.
Although they identified their
findings as specific to correctional work, Gafford and colleagues describe risk
and strengths that are more generally applicable for therapists. Risks include
exhibiting moral superiority, discounting the client’s religious awakening or
beliefs, viewing faith as a discounting of responsibility, lacking cultural
comfort with client identities, and viewing religion as a defense or barrier to
treatment. Strengths include openness to client cultural discussions,
regulating negative feelings perhaps related to previous clients, exploring
cultural values, and openness to discussion of a religiosity-respectful process
(Gafford, Raines, Sinha, DeBlaere, Davis, Hook & Owen, 2019)
Disability
Disability is a lasting
physical or mental impairment that significantly interferes with an
individual’s ability to function in one or more central life activities, such
as self-care, ambulation, communication, social interaction, sexual expression,
or employment.
Disability is a broad concept
used to describe the interaction of physical, neurodivergent, psychological,
intellectual, and socioemotional differences with personal and environmental
factors including attitudes, cultural beliefs, legal and economic policies,
transportation, access, etc. A result may be disability stigma (Balva &
Tapia-Fuselier, 2020). Generally, training for therapists on disability ranges
from limited to nonexistent. And therapists are often not prepared to work with
clients with visible or hidden disabilities. Barriers for the disabled include
attitudinal, communication, physical, policy, social, and transportation
barriers.
"Ableism” is
discrimination toward and social prejudice against individuals with
disabilities. The American Psychological Association issued guidelines for
Assessment and Intervention with Persons with Disabilities (2022) that advocate
for changing ableist practices. That is, addressing and counteracting negative
stereotypes and assumptions and implicit bias which often result in
microaggressions. As lack of training and experience lead to prejudice, it is
essential for therapists to gain experience and to identify and address faulty
assumptions and bias. Recommended practices include therapist self-examination
of biases, beliefs, and emotional reactions to individuals with disabilities; and
considering implicit bias and intersectionality of race, nationality, and other
identities with disability. Since attitudes are deep-seated, self-awareness and
reflection are imperative. Strength-based approaches are indicated. Imperative
is knowledge of the Americans with Disabilities Act (ADA) (1990), the Americans
with Disabilities Amendments Act (2008); and the Individuals with Disabilities
Education Act (IDEA) (1997). Understanding the function and requirements of
reasonable accommodations is essential.
Developmental disabilities
refer to limitations in cognitive and functional abilities impacting learning,
problem solving, reasoning, planning, and in adaptive behavior such that the
individual does not acquire nor evidence skills that would be expected for
their developmental or chronological age group and would be necessary for
independent functioning as an adult. Neurodiversity refers to the shift to a
more positive, strengths-based approach to what were previously referred to as
autism, neurodevelopmental disorders, ADHD, and other behavioral differences (Fung,
2021).
Intersectionality
Increasingly it was
understood that most important is “intersectionality” or consideration of the
multiple identities of the client and therapist (and if under supervision,
those of the supervisor as well). This led to the current conceptualization and
critical component of multicultural practice, the concept of cultural humility,
openness to client diversity statuses, and recognition of the complexity of our
own status, and society’s and their intersection in relation to the client’s
identities, being respectful, open, and humble. The therapist needs to be open
to the worldviews and belief structures of the client(s) – often many within a
family constellation – and to be self-aware and monitor our own emotional
responses to difference. Further, exploration of “missed opportunities” to
discuss culturally relevant aspects of identity, behavior, and relationships in
life and in psychotherapy was introduced as there was substantial recognition
that such opportunities were frequent.
Recognition grew that client
reports of therapist behavior were more complex, multifaceted, and intersectional – these
concepts were not able to adequately address them.
Humility generally is
described as a fundamental human virtue. It is advocated in religious,
spiritual, and philosophical traditions, with adaptations and variations on
definition.
The Impact of COVID
Impact of COVID was
devastating generally and revealed dramatic health disparities for members of
racial and ethnic minority groups who had higher rates of COVID-19 positivity
and disease severity than White populations, less access to care, and had more
negative outcomes, including death. Causative factors included overrepresentation
of members of racial and ethnic minority groups in essential jobs which
increased vulnerability and exposure to COVID-19, lack of primary care access,
lack of health insurance and access to emergency care, as well as lack of
resources available in hospitals, differentially (Magesh et al., 2021). Social,
economic, and health inequities were perpetuated and exacerbated. COVID has led
to loss of beloved elders, loss of schooling or diminished schooling via
telecommunication as racial and ethnic minority students had less consistent
access, support, and connection (Falicov, Nino, & D’Urso, 2020). Mental
health needs rose as mental health resources were severely disrupted.
Recommended practices for clinicians included generally adopting an attitude of
cultural humility, focusing on identifying “emotional contagion,” identifying
impacts of systemic injustice that are likely being compounded by COVID-19, and
recognizing and addressing racial trauma in clients of color (Meyer & Young,
2021). For clinicians, moral injury occurred in that in multiple circumstances
they encountered experiences that were in conflict with their personal values,
making decisions where all options could lead to negative outcomes, sharing
pain and trauma with families, and fearing for their own safety.
Cultural Humility
Clearly, knowledge and skills
are not sufficient. The therapist must exhibit an attitude of the essential
importance of cultural humility – but simply espousing this is not sufficient;
one’s actions and attitudes must be syntonic and evident. This includes active
recognition of one’s own beliefs and biases, in value-attached and historical
context. Childhood experiences can be emblematic in our current behavior – and
may not even be noticed or recognized. Thus, a therapist may make assumptions
about a client based on their own life experience, or may have a negative
predilection toward an aspect of the client that they have not even recognized
or acknowledged. It only becomes recognized through reflection, noticing our
own behavior that is unusual or deviates from what one usually does. For
example, a client may share an identity with the therapist, for instance coming
from the same part of the country, and implicitly, without consciously
recognizing it, the therapist may be operating with assumptions based on their
OWN life experience – experiences during elementary school, values attached to
moving across the country, or multiple identity assumptions (socio-economic
status, ethnicity, race, religion, political affiliation, gender, gender
identity, sexual orientation, etc.).
“Cultural humility” is a
term introduced in 1998 by physicians Melanie Tervalon and Jann Murray-Garcia. It
entails humility and engaging in self-reflection and self-critiquing throughout
one’s client interactions and in formulations and clinical interventions. Anchored
in what we call “metacompetence,” or identifying and “knowing” what we do not
know, being humble, open, and resourceful, engaging the client in exploration
with respect and acknowledgement that the client knows their own experience
substantially more than we do. And, that we truly do not know what we do not
know. Cultural humility is both an attitude and a worldview. It has been defined
as “the ability to maintain an interpersonal stance that is other-oriented (or
open to the other) in relation to aspects of cultural identity that are most
important to the client” (Hook et al., 2013, p. 354).
Consider the following
dimensions of cultural humility: Accurate perception of one’s own cultural
values and other-oriented perspective incorporating respect and respectful
process, lack of superiority in attitudes or behavior, openness to feedback
(even negative) from others, awareness of judgments.
Words to describe clinical
interactions: Open, non-defensive, thoughtfulness and reflection before
determining response to culturally loaded queries or topics, respectful
curiosity, ability to question our assumptions and beliefs in a cultural frame,
markers of cultural humility.
Consider your own cultural
identities and which are associated with power; which with privilege vs.
prejudice, discrimination, oppression, in a frame of historical context. (Privilege
defined as status(es) that afford you a benefit or advantage over others [Falicov,
2014; Hook, Davis, Owen, & DeBlaere, 2017, Falender & Shafranske, 2021]).
Cultural humility entails the
specific ability to maintain an interpersonal stance that is respectful and
open to the other, to their experiences, worldviews, and to aspects of their
personal cultural identity. In displaying respect, therapists do not appear
“superior,” instead having a stance of openness and acceptance of the client
and their personal experience. The therapist collaborates with the client, hears
the client’s disclosures and perspectives, and considers the uniqueness of the
client’s presentation of intersectionality, their multiple identities and their
intersections (i.e., ethnicity, gender, sexual orientation, age, socioeconomic
status, race, religion), mindfully noting their own intersections and attending
to not inferring worldviews similar to the client’s. Key to the therapist
approach is an attitude of “not knowing” and being open to differing worldviews
and experiences that the client presents. We frame not knowing as
“metacompetence,” or being open to knowing and identifying what one does not
know. That is inclusive of being alert to areas of lesser competence, and being
open to disclosing lack of knowledge, skills, or perspective regarding a
particular area or areas.
Hook, Davis, Owen,
Worthington, and Utsey (2014) caution that rather than assuming
knowledge and understanding of diverse clients, therapists remain mindful that
we need to be aware of the limits of our knowledge of someone else’s life
experience. Cultural humility in the therapist is strongly associated with the
therapeutic alliance in that the therapist’s attitudes and values and openness
to “other” stance is strongly associated with the working relationship. In
fact, cultural humility was judged more important than therapist similarity,
knowledge, experience, and skills (Hook et al., 2014).
On a scale of cultural
humility developed by Hook and colleagues (2014, p. 357), positive items
connoting cultural humility included being respectful, open to exploring,
considerate, interested in learning more, open to seeing things from others’
perspectives, open minded; and asking questions when uncertain. Conversely,
negative exemplars included assuming one already knows a lot, making
assumptions about others, being a “know-it-all,” acting superior, and thinking
they know more than they actually do. And client perceptions of a therapist’s
degree of cultural humility were generally positively related to higher quality
of alliances with the therapist, but that was a finding that required further
study.
Cultural humility has been
described as composed of cultural humility, cultural opportunities, and
cultural comfort. The three pillars are: 1) cultural humility; 2) cultural
comfort; and 3) cultural missed opportunities. Cultural humility is defined as
the establishment of egalitarian, collaborative relationships with clients
while at the same time remaining self-aware and non-defensive regarding the
therapists’ own limitations to being other-oriented. Cultural comfort is the
level of genuine comfort one has in holding space for multicultural discussions
and conducting those in therapy. Cultural comfort has also been described as
the ways a therapist finds to be at ease, relaxed, and open when discussing
clients' cultural identities in treatment. A research finding is that client
perceptions of therapist’s cultural comfort were predictive of decreases in
psychological distress (Bartholomew, Perez-Rojas, Lockard, Joy, Robbins, Kang,
et al., 2021). Cultural missed opportunities refers to how often and how deeply
(and sincerely) a therapist explores (or misses) topics related to culture and
identity with a client (Owen, 2013; Owen et al., 2011) and lets opportunities
slip by.
Therapists who are rated high
on cultural humility and cultural comfort, and low on missed opportunities,
demonstrate better treatment outcomes generally.
The client may perceive the
therapist as having missed opportunities to discuss their cultural background,
wish the therapist had encouraged more discussion of culture and cultural
background, avoided topics related to the client’s cultural background, or
generally missed opportunities to have deeper discussions on those topics. Conversely,
the client may feel gratified that the therapist addressed, in depth, cultural
background (Owen, Tao, Drinane, Hook, Davis, & Kune, 2016).
Consider ways a therapist can
communicate cultural humility rather than communicating superiority or already
knowing. Consider again the words that can be used to describe clinical
interactions such as open, non-defensive, thoughtfulness, and reflection before determining responses to culturally loaded queries or topics, respectful
curiosity, ability to question our assumptions and beliefs in a cultural
frame – are all markers of cultural humility. Think about ways you communicate cultural humility.
Generally, when therapists
are culturally humble, they convey openness, respect, and interest. Both verbal
and nonverbal expressions are important.
Interestingly, depending on
context, identity salience changes. That is, one or several identities may be
salient in some situations and others in other situations. For example, one’s
religious identity would be salient when one was at a church or temple event,
the same individual’s racial identity salient when in a mental health
multicultural seminar. Less attention has been devoted to intersectionality,
which is a very important factor in understanding identities.
Davis and colleagues (2018)
proposed a multicultural orientation framework to address how cultural dynamics
influence the process of psychotherapy. That is, as theorists and researchers
have long suggested, psychotherapy relationships which include therapist
empathy and creating a working relationship with the client are inadequate
without consideration of the multicultural factors and dynamics of the client,
family, and significant others. So, focus is shifted to what is described as
orientation or how the therapist views, organizes, understands what the client says,
and how the client creates meaningfulness of the world and relationships within
it. They suggested that rather than focusing on “competencies,” which might be
perceived as inflexible, the therapist needs to be attuned to context,
behavioral change, and meaning. And the therapist does need to attend to identifying
and knowing what they do not know, which Falender & Shafranske (2021) refer
to as “metacompetence” – the ability to step back and increase awareness that one
does not know another’s experience, perceptions, or understanding … and the
therapist needs to be open to that recognition. In multicultural therapy (which
is ALL therapy), attunement to what one does not know is essential, as is openness
to that fact. The client is the expert on their own life and situation; the
therapist can assist them in multiple ways, but the client remains the expert
on their experience.
Key components of cultural
humility include respectful process, openness, and curiosity (Falicov, 2014) as
well as attending to intersectional identities of client, therapist, and if
there is one, the supervisor.
Another concept, intellectual
humility, is also essential in clinical practice. Intellectual humility is
best defined as people’s willingness to reconsider their views, to avoid
defensiveness when challenged, and to moderate their own need to appear
“right.” It is sensitive to counter-evidence, realistic in outlook, strives for
accuracy, shows little concern for self-importance, and is corrective of the
natural tendency to strongly prioritize one’s own needs. See: templeton.org/discoveries/intellectual-humility.
An additional critical
component within multicultural practice is social justice, addressing
the fair treatment and equitable status of all individuals and social groups
within a state or society. It also refers to advocacy focusing on forms of
oppression that limit access and opportunity in society as a function of
membership in socio-demographically diverse groups. It is aimed at attending to
change in societal values, policies, and practices to increase access to tools
of self-determination (derived from Goodman et al. 2004). Social justice has
been often sidelined or ignored by mental health professionals with the
exception of social workers for whom it is among their guiding principles (NASW,
2019) with articulation of equity and inclusion, spanning voters’ rights,
criminal and juvenile justice, environmental justice, immigration, and economic
justice. (See the section on Social Justice, below. )
Incorporating social justice
includes perspective-taking and consciousness-raising about differences and
inequities and addressing those; addressing power (in the therapeutic
relationship and societal impact on the client’s presenting problems);
perceptions of fairness and lack of such; and expressions of empathy, support,
and connection.
Gender, gender identity,
sexual orientation, race, ethnicity, and to some extent disability, are being
addressed and are increasingly recognized as significant identity factors in
mental health practice. However, consider multiple other identities that are
NOT being addressed or noticed in mental health, and the intersectionality of
identities. Some identities that are less addressed are religion, social class
or socioeconomic status, immigration status, education level, and language, to
name a few. Socioeconomic status relates to access to resources and power, and
positionality in the social class hierarchy. Multiple identities are
interrelated.
Cultural Formulation
Recognizing the cultural
nuances of different groups is important in order to enhance the effectiveness
of treatment outcomes. It increases the awareness and sensitivity in
understanding how different symptoms, disorders, and presenting issues may look
or manifest within and across different cultural groups. As part of a very
thorough clinical intake, the clinician must gather relevant psychosocial,
contextual and historical data that is then conceptualized within the social cultural
context of the client. Culturally informed intake and case formulation allows the
clinician to carefully consider clinically and culturally appropriate diagnoses
and treatment recommendations.
Pamela Hays’ ADDRESSING model (Hays 2001) offers a framework for clinicians to consider not
only the variables of culture to consider when gathering intake information,
and history from a client, but also strategies for self-reflection for the
clinician to consider the ways in which their own biases and cultural
identities emerge within clinical practice. ADDRESSING stands for:
- Age and
Generation;
- Developmental Disability;
- Disability (Acquired);
- Religion;
- Ethnicity and Race;
- Socioeconomic Status;
- Sexual Orientation;
- Indigenous Heritage;
- National Origin
and Language; and
- Gender.
Integrating the ADDRESSING framework into clinical
practice can lead to a cultural understanding of the client which offers the
clinician a robust case formulation that examines how social, cultural,
historical, and contextual variables are embedded within the development and
maintenance of clinical issues. An added benefit to application of Hays’ model
is that she encourages the clinician to consider not only their own cultural
factors as it relates to the multiple identities of their clients, but also
exploration of how these variables differently affect groups based on
membership in either the dominant or non-dominant group ( Hays 2022).
Below is a sample vignette which illustrates how
critical the integration of culture at time of intake is for clinicians. Please
read the vignette and then answer the questions that follow:
Jessie is a 35-year-old single male who presents for
an intake session seeking help for symptoms of anxiety and depression which are
interfering with his work performance. Jessie has difficulty sleeping at night
due to racing thoughts and has recently lost approximately 10 pounds in one
month. Jessie works as a software engineer and reports feeling overwhelmed and
stressed out by the job, which often requires long hours.
As you read the vignette, did you notice any automatic
assumptions regarding Jessie’s gender, race, ethnicity, or age? What are your
initial thoughts in terms of the assessment of Jessie’s symptoms and factors
contributing to the onset of symptoms? What might be some initial
recommendations or considerations for a treatment plan?
Now
consider that Jessie is a 35-year-old single woman and is one of few women in
her workplace. In what way does that change your conceptualization of the
workplace anxiety and any intake questions you may ask. What if Jessie is also
Jewish and there has been recent antisemitic violence in the area where her
company office is located. This vignette illustrates how therapists working
with clients from various cultural backgrounds need to understand and
appreciate the systemic, contextual and cultural differences that may impact
their clients' mental health and wellbeing.
When attending to diversity factors and in modifying
treatment to meet the needs of clients there can be assumptions about
appropriateness of evidence-based treatments
To address the role of
cultural variables on the diagnosis and treatment of mental disorders, the
Diagnostic and Statistical Manual of Mental Disorders - IV (DSM-IV) included an Outline of Cultural Formulation to give clinicians guidance on factors
to consider that yield better understanding and consideration of the impact of
psychosocial and cultural factors on symptom presentation.
As outlined in the DSM -IV,
the Outline of Cultural Formulation (OCF) consists of five components:
1.
Cultural Identity of the Individual
What are aspects of the client’s culture, race, ethnicity, nationality that
influence the presentation of symptoms as well as the client’s beliefs about
mental illness.
2.
Cultural Explanation of the Individual’s Illness
Exploration of how the client’s cultural background informs their explanation
of the cause and contributions to their psychological distress and mental
illness.
3.
Cultural Factors Affecting the Psychosocial Environment and Levels of
Functioning
Exploration of how client’s level of functioning, interpersonal dynamics,
family relationships, and social support systems are affected by cultural
variables.
4.
Cultural Elements of the Relationship Between the Individual and the Clinician
Encourages therapist to consider similarities and differences between therapist
and client to consider if and how those factors can affect the therapeutic
relationship.
5.
Overall Cultural Assessment for Diagnosis and Care
In this last component, the clinician integrates all the pieces of information
together to develop a culturally sensitive formulation which considers how
clients will respond to treatment.
While this OCF addressed a
previously neglected aspect of diagnosis and treatment planning, there was
still a need to provide direction and guidance to therapists on developing a
cultural formulation. Authors of the Diagnostic and Statistical Manual, 5th Ed.(
DSM 5) were very intentional in designing a Cultural Formulation Interview
(CFI) that expanded upon the OCF by detailing specific questions to elicit
information related to the client's cultural factors. The CFI defines culture
as the following (Aggarwal & Lewis-Fernandez, 2020):
Culture
refers to systems of knowledge, concepts, rules, and practices that are learned
and transmitted across generations. Culture includes language, religion and
spirituality, family structures, life-cycle stages, ceremonial rituals, and
customs, as well as moral and legal systems. Cultures are open, dynamic systems
that undergo continuous change over time; in the contemporary world, most
individuals and groups are exposed to multiple cultures, which they use to
fashion their own identities and make sense of experience.
The core CFI is a structured
interview comprising 16 questions that are organized around the five domains of
the OCF (Aggarwal et al. 2013).
The core CFI is organized into
four sections:
1) cultural definition of the problem;
2) cultural perceptions of cause, context, and support;
3) cultural factors affecting self-coping and past help-seeking; and
4) cultural factors affecting current help-seeking (Aggarwal & Lewis-Fernandez,
2015).
In addition to these four sections, there are also three supplemental domains
that can be appended to cultural formulation interviews to further assess the
socio-cultural factors relevant to an individual’s mental health functioning
(Jarvis et al, 2020):
1.
Cultural Strengths and Resilience
Within this domain the therapist identifies cultural traditions, rituals and
routines that serve as sources of support and can be integrated into treatment
planning to promote wellness and recovery.
2.
Cultural Challenges or Barriers to Care
This domain provides direction on asking questions about cultural factors or
beliefs about mental health that may interfere with accessing or receiving mental
health care.
3.
Cultural Identity of the Clinician
This supplemental domain has the clinician reflect on their own cultural
background and how it might impact the therapeutic relationship. Mental health
providers consider cultural biases as well as present ideas and techniques for
promoting cultural humility within the therapeutic setting.
There are also twelve
additional supplementary modules to the CFI which offer a more in-depth exploration of the five domains as well as considering
the specific needs of unique treatment populations such as children, older
adults, immigrants, and/or refugees.
A third component of the CFI
is an informant version of the CFI that allows the clinician to gather
collateral information and obtain the perspectives of family members and social
support systems of the CFI. As a clinical intake tool, the CFI assists the
clinician by providing a thorough, systematic, culturally informed tool which allows
the provider to understand the client’s perspective and worldview and achieves
the goal of inviting in the client’s perspective and worldview in consideration
of assessment, diagnosis, and treatment.
Let’s now apply Hays’
framework to the following vignette. As you read through the case, consider
what aspects of the client’s identity are most salient in presentation of
symptoms.
Phil is a 67-year-old heterosexual, self-identified Christian,
Caucasian, married male. He states that his doctor suggested he seek therapy
after complaints of headaches and stomach pains that had no known medical
cause. He recently retired and lives in an urban city with his wife. They have
two children and three grandchildren.
During the intake, Phil indicated that he worries all the time, and
about “everything under the sun.” For example, he reports equal worry about his
wife who is undergoing treatment for breast cancer and whether he returned his
book to the library. He recognizes that his wife is more important than a book
and is bothered that both cause him similar levels of worry. According to
Phil, he is unable to control his worrying. Accompanying this excessive and uncontrollable
worry are difficulty falling asleep, impatience with others, difficulty
remembering things, and significant back and muscle tension.
Phil states that he has had a lifelong problem with worry, recalling
that his mother called him a “worry wart” as a kid. He reports that he was a
good kid in school who made mostly all As and Bs. He graduated from college
with a business degree and has worked as an accountant most of his life. He
recently retired and has spent most of his time caring for his ill wife. His
worrying does wax and wane, and it worsened when his wife was recently
diagnosed with breast cancer.
Consider that you are
employed at a clinic that uses CBT for anxiety treatment protocol. Phil is
initially reluctant to engage in treatment as his experience of his anxiety is
physiological and he is unsure of how “talking” about his problems will provide
relief. In the initial sessions, you assign homework consistent with your
treatment model that Phil does not complete. He is very apologetic and always
assures you he will return with his homework done the following week.
Using Pamela Hays
ADDRESSing model what cultural factors are relevant for this case? What
adaptations if any might be needed to increase engagement and participation in
treatment? How might this differ if you were using a different treatment model?
Some of the variables
that are important to consider are Phil’s age, status as a recent retiree,
cultural norms, and ideas about being a husband, father, and grandfather and
how his age and recent retirement affect his role as a father and husband. In
what way might his anxiety increase as a result of change in his status in
these roles?
Intersectionality
Intersectionality is a term
developed in 1989 by the legal and race scholar Kimberle Crenshaw to explain
marginalization and oppression. She stated, “Black women are sometimes
excluded from feminist theory and antiracist policy discourse because both are
predicated on a discrete set of experiences that often does not accurately
reflect the interaction of race and gender… Because the intersectional
experience is greater than the sum of racism and sexism, any analysis that does
not take intersectionality into account cannot sufficiently address the
particular manner in which Black women are subordinated” (p. 140).
The concept of
intersectionality has been adopted by multiple professions including the American
Psychological Association (2017): social identities are interrelated,
interwoven, overlapping, and multi-layered. Consideration of privilege and
oppression based on social hierarchy addresses societal inequities. Identities
are not binary – for example, race – even within racial identity groups, skin color
can be associated with power or status. Or for immigration, assimilation may be
a significant variable that is associated with different levels of status
depending on the context.
Identities
- Gender
- Sexual orientation
- Gender identity
- Race
- Ethnicity
- Culture
- Language
- Language of origin
- Country and region of origin
- Immigration, immigration status,
citizenship
- Generation
- Acculturation
- Age
- Socioeconomic status
- Religion
- Spirituality
- Disability or Ableness
- Urban vs. rural/remote
- Body size
- Military experience
- Global, transnational
- Privilege / role of power
- Other factors including worldview
Consider your own identities,
intersections, and impacts with a particular client. Do they vary? Are certain
identities more prominent with a different client? How does that impact
assessment, diagnosis, case conceptualization, therapy? Then consider which of
your identities are associated with power and privilege? Which with oppression
and marginalization?
Then turn to consideration of
your client’s identities. Within a family constellation there may be significant
diversity in identities depending on the multiple aspects of identity
previously alluded to.
How different will therapy be
with a client who shares two or more identities with you versus one who shares
none? Are some of these implicit or explicitly discussed? Think of examples in
your current experience or during training.
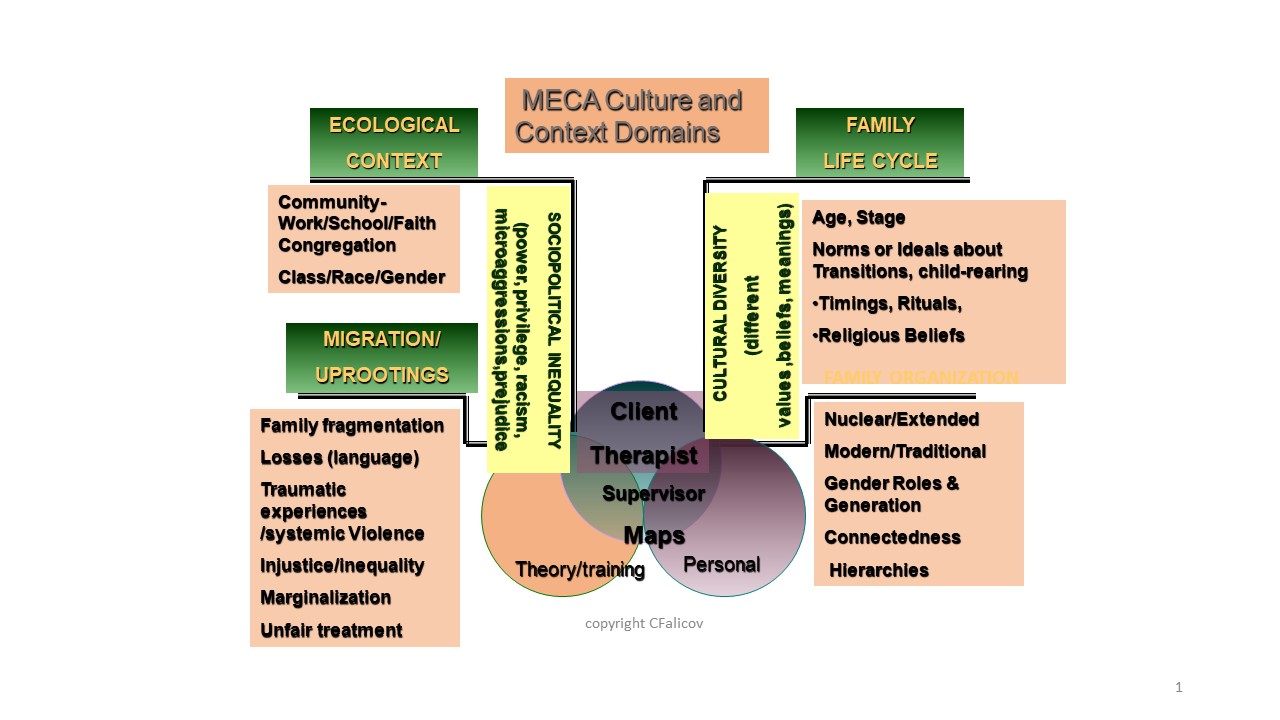
Falicov’s MECA Theory
A different framework
developed by Celia Falicov, is also useful in approaching intersectionality and
incorporating multiple aspects of diversity into practice. First, Celia
Falicov’s Multidimensional Ecosystemic
Comparative Approach (MECA) (Falicov, 2014; 2017) provides a framework
(Figure 1) that should not be your sole focus, but presents factors that are
essential to understand as part of an individual’s ecological niche, how they
fit in society. We are all multicultural beings and not subsumed under a
particular label or identity but by the intersections of those. These include
universals, particulars, or idiosyncratic histories, culture-specific aspects
(ethnic values, religious rituals), and each person’s ecological niche or
intersectional cultural identifiers. Note that the culture of each participant – client,
supervisee, and supervisor – are all included and essential in the cultural map
and formulation. Contextually, values, beliefs and meanings are not inferred
but are considered in the frame of culture of the clinician and the
relationship of those to the client/family.
Note that for Falicov,
culture refers to sets of shared worldviews, meanings attached, and adaptive,
functional behaviors, all derived from membership and participation in a variety
of contexts. These include languages spoken and understood, residing in rural
versus urban or suburban areas, race, ethnicity, socioeconomic status, age,
gender, sexual orientation, gender identity, religion, disability or ableness,
nationality, employment, education, occupation, political ideology, stage of
migration/acculturation, and experiencing and identifying with historical
moments (Falicov 2014). Exclusion from various contexts may also be essential
and critical parts of one’s cultural experience (Falicov 2014).
A first step is
self-assessment of the clinician’s own cultural contextual domains and
worldview. Consideration includes how the clinician’s own worldviews are
impacting questions asked and assumptions made, as well as guiding an empathic
process (Falicov, 2014). The process is conducted within an attitude of
respectful curiosity and not-knowing, rather than inferring or assuming
universals: understanding individual variations and the intersectional
complexity.
The MECA Framework Includes
Migration and Uprootings
When, how, and why did the
family migrate? And what was the process? Was it traumatic? Migration is viewed
in the context of loss and change, including some resultant gains. Families may
be fragmented geographically and psychologically as those who migrated become
acculturated or as connections are severed or lost completely. Systemic
violence could be the precipitant to or result of the uprooting. Injustice and
inequality may impact the family members uniformly or individually. Cultural
gaps between parents and children and within members of the family thus may be
exacerbated by the migration experience and the entry into the new culture and
role transformation or changes in traditional roles and subsequent differential
wages (i.e., a father who was a lawyer in their country of origin becoming a
low wage worker; the mother, previously unemployed working as a seamstress and
earning more money). Gender roles may evolve due to media exposure and cultural
immersion at school and result in changes to traditional expectations. Such
changes might entail highlighting cultural gender restrictions, tensions
between roles viewed on media and traditional ones. Also, a son or daughter who
becomes fluent quickly may become a translator for the family; the parent may
have lost specialized employment status from pre-immigration and be relegated
to a lower wage and level; the child(ren) may be left with a family member
including a sibling or other person for care; and family dissolution may result
from changes in status, self-worth, or other factors. Tensions may arise from
role issues, such as women being viewed as “less than” compared to men. Thus,
while respect is a high value, conflict may arise from frustration for the
undervaluation of the women. Questions include when, why, and how they migrated
or moved, current immigration status, connections with the country of origin,
including who was left behind, trauma in the country of origin and/or during
the immigration experience, injustices, marginalization, unfair treatment, loss
of status or security, current family dynamics and changes to those, to name a
few. Telecommunication may serve as a powerful connection to those remaining in
the home, country of origin, locale.
Ecological Context
This domain considers
diversity in where and how the family lives and fits in the sociopolitical
environment. This includes racial, ethnic, socioeconomic status/class,
religion, educational communities, living and working conditions, involvement
with schools and social agencies. Sensitivity to marginalization, consequences
of marginalization, discrimination experienced by family members due to race,
socio-economic status, documented or undocumented status, or multiple other
factors including exposure to racist or sexist stereotypes, all result in
powerlessness. Beliefs about physical and mental health, religion, spirituality
and magic are little explored in clinical practice, but are highly relevant to
clinical work, as are attitudes toward psychotherapy and complementary folk
medicine. Exploration of beliefs about personal responsibility, gender and
racial socialization, and sources of support through family, churches, or
affinity groups and how those relate to coming for psychological intervention,
are all important components as it is critical not to make assumptions based on
our own experience and beliefs.
Family Organization
This entails a consideration
of family structure and values relating to family structure and functions. Is
the organization nuclear or extended? What is the degree of connectedness? How hierarchical
in terms of respect, decision-making, and parent-child involvement? Some
families are collectivist family arrangements with high levels of parent-child
involvement, parental respect that endures through the entire life cycle,
across generations. Others are nuclear families that favor strength of the
parental unit, distinct from others. Nuclear family relationships may favor the
strength and power of nonblood relationships, husband and wife. When cultural
transformations, migration, or other changes occur, Falicov (2014) identified
how this impacts connectedness and separateness, generational hierarchies,
communication, conflict resolution, and secrets.
Family Life Cycle
In family life cycle, the
clinician assesses age and stage of development: chronological and
developmental position in terms of life and professional experience. The
clinician considers their own position chronologically, and their internalized
norms or ideals about child-rearing and life transitions (e.g., adolescence,
adulthood), construction of age-appropriate behavior – what one’s own personal
experience was like, what was normative for one’s setting and family, rituals
including religious, socio-cultural, or intrinsic to one’s family or milieu,
timing of transitions into adulthood or independence, and religious beliefs
generally and the impact of these on the presenting problems/issues of the
family. Next is conception of family: extended or nuclear family, gender roles,
flexibility, and generational considerations (e.g., if there is
multi-generational participation in child rearing; caretaking for elders),
gender role definition, hierarchies within the family that determine decision
making.
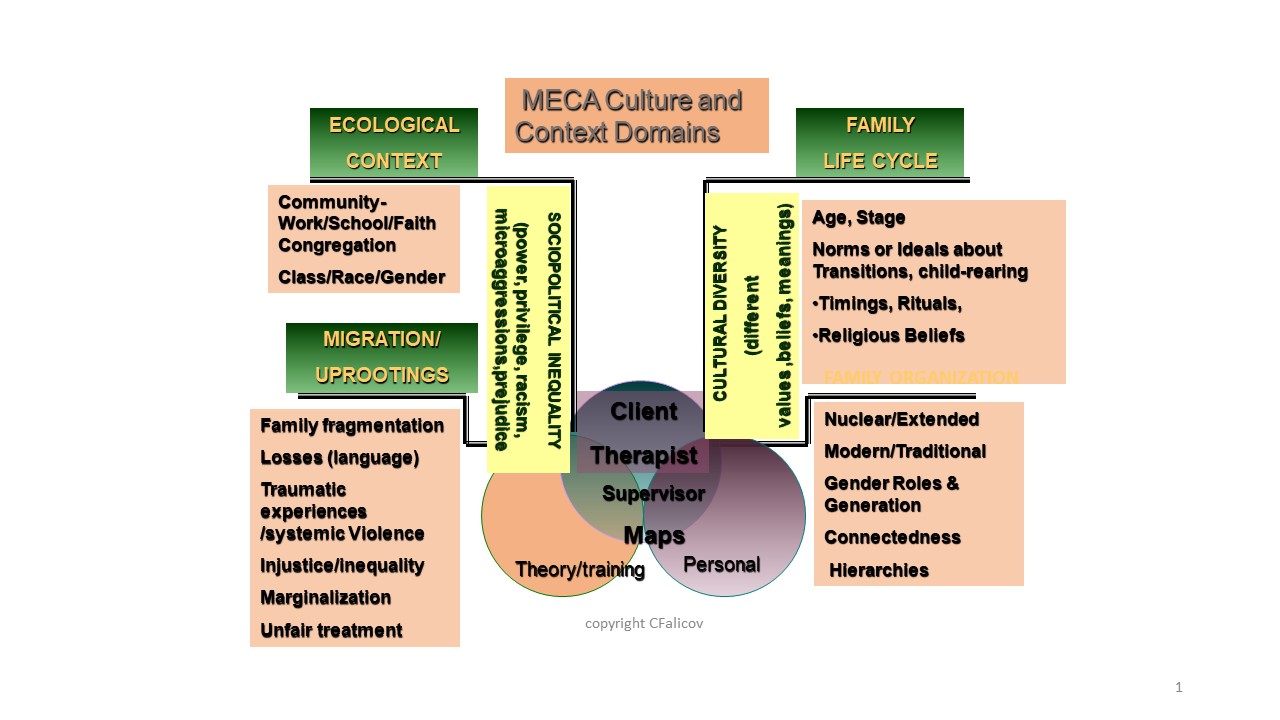
Figure 1. MECA (Multidimensional
Ecosystemic Comparative Approach) Culture and Context Domains
The intersection of these
components provides the clinician with a framework to address individual and
families and to understand the complexity of culture and intersections with
presenting problems in mental health. Consideration of the ecological niches
and worldviews of the clinician(s)/therapist(s), client(s) and families, and,
as relevant, supervisor(s), provides a backdrop to contextualize culture and
its multiple framing elements that are relevant to diagnosis and treatment.
To illustrate this model,
consider the multiple aspects of MECA and how the components of a case and the
therapist plan structure and intervention through a multicultural lens.
A new client, a 12-year-old
BIPOC male, who presented with significant school discipline problems and poor
performance of at least a year’s duration, is being raised by his great aunt
and uncle, who are in their late 70s, As they are the only remaining family
members after the death of his parents in a car crash when he was seven, they
agreed to raise him. His parents had been in and out of jail for years, used
illegal drugs, and he had only hazy memories of them. He had been in foster
care several times, having been removed from parental custody by the Department
of Children’s Services, but then reunited when his parents were deemed ready.
His great aunt is White, his great-uncle BIPOC. The client told the therapist
during their first session that his aunt had informed him a few weeks prior that
the day he turns 18 he will be on his own and no longer live with or be
supported by them. He reported he is often hungry as he is growing fast and the
lunch he brings to school doesn’t fill him up. The client was initially eager
for therapy but warned the therapist not to expect much from him. He described
his major (and only) strength is playing football but that is seasonal and, due
to his school performance, he may not be allowed to play in the coming season
if his grades continue to be below a “C” average. He had played at several
previous schools he attended and had been a “pretty strong” quarterback. What
is the effect and the range of emotional responses of the child and of the
therapist in response to the preliminary information? How would treatment
progress, being sensitive to the youth’s presenting problems of school-defiant
behavior and his relationship with the family?
The supervisee, a Latina, had
a very strong empathic response to the client after this disclosure, felt angry
with the great aunt and uncle, and found it difficult to even see the client
due to her own empathic reaction and concern for the child. Consider this scenario
in a MECA framework and with the assumptions about each domain described above.
Consider how you as the clinician would approach therapy. Consider what
emotional response this elicits in you, as the supervisor. Then consider how
you would proceed.
In the frame of cultural
humility, consider the following questions which were previously introduced in
this module:
- Would you use the following words to
describe the clinical interaction: open, non-defensive, thoughtful, or
reflective before determining responses to culturally loaded queries or topics?
Are you displaying respectful curiosity? Are you able to question your
assumptions and beliefs about this client within a cultural framework?
- Consider your own cultural
identities and which are associated with power; which with privilege vs.
prejudice, discrimination, oppression – in the frame of historical context.
- Privilege defined as status(es)
that afford you a benefit or advantage over others. (Falicov, 2014; Hook,
Davis, Owen, & DeBlaere, 2017, Falender & Shafranske, 2021)
Reflections
Migration and Uprooting
Consider the therapist’s own
identity. The therapist felt intense empathy for the youth, for the losses and
for the trauma compounded by going to live with people he barely knew and who
were not prepared to raise a child or teen. The therapist, a Latina in her late
30s recalled her own childhood, and thought about what the loss of her parents
would have meant and how she was blessed with a strong extended family. She
reflected on her close family network, strengthened by the fact they were
immigrants and found significant support from each other.
From the child’s perspective,
she viewed the uprooting as a continuation of the ongoing trauma of parental
neglect, foster care, death of his parents, relocating to a new geographical
area to live with a much older great aunt and uncle he had never met, changing
schools, and losing his one friend.
Ecological Context
Consider the therapist and
client differences with respect to power, privilege, identity, and culture and
how these potentially increase social and cultural distance and may lead to
misunderstandings or miscommunication that may result in ruptures, and may ultimately
have potential to contribute to, if not cause, severe alliance ruptures and
have definite potential to complicate any rupture repair process (Chang, Dunn,
Omidi, 2020), increase social and cultural distance, and render the
psychotherapeutic intervention less efficacious.
In this case example, the clinician accepted the client’s belief that they could not make the
football team due to ethnicity but learned that assumption was invalid as the client’s
counselor indicated it was because of grade point average. The clinician
formulated the great aunt and uncle to be unsupportive, potentially limiting
caloric input of the youth and being rejecting, with respect to the statement
about him “being on his own” at the age of 18. It was difficult for the
clinician, who felt significant empathy for the client, to separate these
formulations from her work, even though she reluctantly agreed they were not
founded on direct data, and data existed to the contrary (as he had a wide
range of healthy foods in his backpack and snacked on fruits and vegetables
during their sessions). In fact, her supervisor reminded her that in her
required meeting with the great aunt and uncle, she had observed them to be eager
for intervention, and struggling with the difficulty of raising a teen who had
lost so much, sustained unknown amounts of trauma and who felt very
disconnected from them, and with their own economic worries as they had planned
for a very different retirement. Even when the clinician saw the food on
multiple days, and saw evidence of their caring behavior, it was difficult for
her to be empathic toward them.
Family Organization and
Family Life Cycle
The couple had never raised a
child, was struggling financially and emotionally with the task, but was
dedicated to “seeing it through” even though they had hoped for a calm
retirement, had planned to sell their house and use the proceeds to live on,
buy a used RV and see the country until they had to live in a low-income
retirement community when they were much older, but now had a child to raise.
They had been married for more than 50 years and had a strong relationship, but
felt “cracks” emerging in their relationship with respect to efforts to deal
with the child. They were increasingly isolated as they no longer had work
contacts and now with raising a child, they had little time. His great aunt is
White; great-uncle, BIPOC. They were both from intact families and wanted to
provide the best they could for him but kept encountering his withdrawal and
disinterest in anything they suggested, so they were frustrated and felt
rejected and impotent. The great aunt said she had never parented, and her own
parents had been formal and not affectionate and her father was rarely present.
They both understood the limits of school-based treatment (to focus on the
child’s school performance) and had tried to seek out family therapy, but the
wait-lists were very long and their finances (both had worked in offices and
had limited retirement benefits) did not allow for the fees of an independent
provider even if they could have found one.
They were disappointed he was
not more connected with them, withdrew a lot, and understood this was at least
in part a result of his childhood experiences and trauma, but even when they
tried, he would not talk about any of that. He generally simply withdrew. They
were older, and not able to participate in sports with him and he would not
watch sports on TV with them. They knew he was a strong runner, but he refused
to run alone.
They were strict in their
rules, mirroring their own childhoods, but found it almost impossible to carry
through as he was highly avoidant and creative at escaping any consequences. They described the fact that even at school, he
was manipulating the system, getting thrown out of class frequently so that he
spent lots of time in the office where there was often food and the office
staff was kind to him, so it was more of a reward than a punishment. They
said the same kinds of things happened at home, revealing he was smart and very
able to get around most rules and consequences. They were used to a
hierarchical family structure, and the great uncle was the disciplinarian. The
great uncle bemoaned the fact that the child’s mother was deceased as he
thought she would have been much more effective parenting this youth. They
expressed concern that where they lived was not conducive to raising him. The
neighborhood was aged, no children nearby, and crime rates were high.
Consider how you would
approach therapy with the child, and what multicultural considerations enter
into your strategies. Consider the aspects of Falicov’s model in your planning.
Consider factors of the timeline, loss, mourning (and identifying whether the
child had an opportunity to mourn), entry into a new school in a new
neighborhood (with unknown diversity factors) and with new parental figures – all
adjustment issues.
Psychotherapeutic Relationship: Strains and Ruptures
In any psychotherapeutic
relationship, a critical component is the therapeutic relationship or the
working alliance which entails agreement on goals and tasks and is the
foundation of an emotional bond, and then attending to the ongoing process,
relationship, and monitoring for strains or ruptures that may arise. These
could be due to misunderstandings, different worldviews or belief structures,
or multiple other factors. In addition, maintenance of reflective practice requires
one to be self-aware of emotional state and changes to that, unusual emotional
responses, assumptions, and the impact of client disclosures or presentation
including multicultural identities, difference, assumptions of sameness or
difference.
Therapists should be
attentive to identification of transference and countertransference with the
client. That includes therapist emotional reactions such as boredom, anger,
irritation, sexual attraction or arousal, to name a few. These emotional
reactions are critical to be self-aware of and are extremely important in
psychotherapy. Sometimes the strength of such therapist response is shocking to
the therapist and it is most important that the therapist identify such
differences in clinical response to a client, their own emotional response or
reactivity, and how to manage those. Some may be representative of experiences
in the past or relationships with others outside the clinical realm. Gelso and
Hayes described countertransference as the therapist’s internal or external
reactions shaped by either (or both) the therapist’s past experiences or
present emotional conflicts and vulnerabilities (Gelso & Hayes, 2007).
Therapist self-awareness and self-insight are critical components, as is the
therapist monitoring their own personal responses, identifying anxiety that
arises, perhaps with respect to culture or cultural difference, identifying and
addressing/managing anxiety that may arise, and, as necessary, receiving
cultural or general consultation from a peer or supervisor to address these
aspects. Countertransference may manifest in deviations from more normative
therapeutic interactions. For example, the therapist may have an intense
emotional reaction to the client that is unexpected and highly unusual. That
might manifest as spontaneous sharing of personal stories, or acting in ways
that are inconsistent with the therapist’s normative clinical behavior.
Culture and multicultural
factors are always in the room, in the virtual connection, and generally in the
relationship, informing values and worldviews, but they may often not be
acknowledged or addressed. Multiple factors intersect and should be considered.
First is the impact of the personal cultural background of client and therapist
on potential countertransference. Second are shared and overlapping assumptions
and familiarity with the cultural identities, as shared identities may be
highly disparate given one’s other identities (socioeconomic status,
immigration history, educational level, employment). Third, what level of
importance or recognition of culture and identities has occurred in the
treatment from its onset? How have you, the therapist, initiated discussion and
recognition of the client's cultural context, connection to the presenting
issues, and cultural disclosures? And the worldviews resultant from those? Falicov’s
(2023) model is useful in these determinations.
Consider the risk for rupture
in the therapeutic relationship. It is known that therapist and client (as well
as the supervisor, should the therapist be under supervision) exhibit
differences in power, privilege, identity, and culture and that these increase
social and cultural distance and have the potential to contribute to alliance
strains or even ruptures. All of this complicates the repair process. Reflect
on cases you have carried and any risk factors and actual strains or ruptures
that have occurred. Examples include misunderstanding or making assumptions
based on something a client said that was not correctly interpreted.
Possible Avenues for
Multicultural Interventions
- The therapist needs to consider the Falicov framework to address
their own assumptions and predilections regarding the child in the case example
above. The therapist is not close in age to the client, yet is empathic about
his situation, losses, and multicultural stressors. A task is for the therapist
to increase self-awareness of the client’s own worldviews and identities, and
how these are impacting the schoolwork. How can the therapist approach the
therapy sessions in ways that will be more meaningful for the child? The strong
empathic engagement is generally a strength, but can it be a liability? How
could that be potentially limiting the flexibility of approaches and
strength-based practice? Consider what the therapist knows about the youth and
what could be done.
- For example, the
therapist learned that in football and other games, the client is very
competitive and likes to win. The therapist could focus on that competitive
strength and assist the client in seeing a clear path from current school
performance to a goal of making grades to be able to play football. If the
youth is hopeless, saying for example, that the team is all White and there is
no way he can get on it, the therapist could test the reality of that
perception and have the child (or the coach) provide input about the realities
of the ethnic makeup of the team and the strong possibility that the youth
could play if they bring their grades up – and that the youth could potentially
be a star due to previous performance (playing quarterback and being a strong
runner). Consider ways to encourage the youth to ask the P.E. teacher about
track-running during PE at school or figure out other ways to increase his physical
activity to enhance the chance of making the team).
- The therapist could play board
games for part of the session, reinforce winning, and help the client to
reflect on positive feelings generated by competition.
- If the youth feels
isolated at school due to a number of factors including being the “new” kid, his
cultural identities, socioeconomic factors, and school behavior, the therapist
could address these directly and problem-solve with the youth and the school
counselor on possible activities to begin to become more integrated into the
school culture, drawing upon the youth’s strengths.
- Get supervision if
possible to help to gain insight to balance
your own (as therapist) empathic engagement with the youth’s realities and
needs, educationally, socially, and multiculturally.
- Underlying issues of
trauma are critical and are likely factors leading to the youth’s avoidance of
relationships and activities. Dealing with rejection could be an important
trigger to identify. Helping with work on appropriate self-assertion, skills
for entering new social situations, self-compassion (Neff, n.d.) and
mindfulness could be important psychoeducational interventions.
Additional
Considerations – Lenses
- Cultural Humility: Accurate perception
of one’s own cultural values and other-oriented
perspective, incorporating respect and respectful process, lack of superiority
in attitudes and behaviors, being open to feedback (even negative) from others,
and being aware of judgments.
- How
to think about one’s own cultural values as a therapist and then to take an
other-oriented perspective, thinking through the lens of the client (and client
family); lacking superiority and being aware of judgments.
- Think about the judgments implicit
and explicit: some include being judgmental about the great aunt and uncle and
translating that into anger which would impact therapy with the youth and
interactions with the family; assumptions about the relationship of the aunt
and uncle with the youth without consideration of trauma, historical factors,
and empathy. How could the behavior of the therapist be proactive – how could it
be detrimental?
- How is privilege being
framed/addressed by the therapist? Advantage?
- Use
a lens of strengths to begin to conceptualize effective intervention – drawing upon
the strengths of the youth, of the family constellation (dedication,
commitment, caring, desire to help and support). Think through a strength-based
lens.
- A general premise is: The client is
the expert on their own experiences and therapists pay special attention to
approaching cultural identities with curiosity and openness.
Considering clinical cases
through a social constructivist, social action oriented frame entails
encouraging perspective-taking, including steps of noting exceptions to
observations, moving toward externalizing the problem from the individual,
considering processes of deconstruction including thinking about how the issue
originated, the belief systems of the youth and the family, reflecting and
taking different roles (having the youth reflect on what they would do as a
parental figure, collaboratively developing hypotheses). Also, to note
exceptions (tell me about the times you were not depressed (or
demoralized) this week … think about the chains of behavior that occur when you
are depressed (you cause a problem in class, you get sent to the office, you
eat food, but you miss class and then fail your next text so then you are
further from your goal of being able to play football next year). Measure
affective response – depressed mood, “disinterest,” “unmotivated,” “connected,”
“happy,” “involved,” or others collaboratively developed.
Give feedback to the
client – about the football team membership failure and discuss what IS within
their power to change.
Think about how the sequence
of events turned out – what were the good consequences that happened; what were
the problematic ones? How could those be shifted? What IS within your control. How
could the counselor advocate for the client?
Cultural Countertransference
Cultural countertransference
is a phenomenon originating from implicit or conscious beliefs, assumptions,
biases, and unresolved conflicts of the therapist or elicited by the client or
setting-specific issues, or by general stimuli. It could be triggered by
cultural events or perceptions of those including spoken language; race,
ethnic, and sexual identities; cultural mores; generational differences; and/or
by childhood personal cultural experiences. The resultant countertransference
could manifest through actions, attitudes, emotional responses, or implicit
assumptions (Hayes, Gelso, Goldberg, & Kivlighan, 2018). It could result in
a client not being forthcoming or comfortable with the therapist or the whole
Western idea of therapy, strain, rupture, and even withdrawal from services.
However, such phenomena are generally not addressed even though successful countertransference
management is positively related to better therapy outcomes. When
countertransference management occurs in clinical sessions, it includes
consideration of the emotional response of self and the client, enhanced
self-awareness in the moment, connection, empathic understanding, anxiety
management, and self-integration (Perez-Rojas et al., 2017).
Disregard for cultural
countertransference might include the therapist discouraging discussion of or
discounting the role of any cultural influence or component on the presenting
problem, the therapeutic relationship, or the general milieu of the client.
Other evidence could be client or therapist detachment in the session,
discounting validity of perceptions of the other, or withdrawal from treatment.
Or a client who does not seem comfortable enough to self-disclose and thus does
not appear to you to be a “good” therapy client.
How to proceed? Perhaps by discussing
the therapist’s expectation for self-disclosure and how it may not be
culturally syntonic or seem safe. And by understanding what the client’s
expectations are from you and what they hope to gain by coming – or if required
to come by some individual or entity, exploring the feelings and context
surrounding that. Ethical aspects include clarity about limits of confidentiality
and general informed consent so the client gains understanding about the
context and expectations. Therapists should be mindful of their own cultural
expectations – in an instance when a family wanted the grandmother to come to
treatment with them, the therapist refused, saying that she is not part of the
nuclear family, not understanding the role of respect for elders, multiple
generations, power, and self-determination within family constellations as
critical considerations. Therapists’ beliefs about whether cultural events had
happened was mediated by multiple aspects including therapist overwhelm or
disorganized countertransference reactions and more colorblindness. In those
instances, therapists were less likely to believe microaggressions had occurred
to clients (Dictato & Torres-Harding, 2022).
Consider cultural
microaggressions that could occur without therapist awareness. For example,
assumptions the therapist could make based on diversity dimensions. An example is
assuming lack of (English) language facility due to client appearance or
reticence to speak.
Use of Falicov’s model
provides a prototype encouraging the therapist to self-assess and consider the
client (and as relevant, the supervisor) through multiple cultural lenses.
Consider a situation with a
client when either your emotional response or your behavior deviated from the
norm or elicited a response different from what you expected. Think about the
aspects of the situation that were operative. Consider cultural factors. How
did you respond, and proceed? Did you identify countertransferential aspects of
the event? How did the client respond?
Navigating Privilege and Oppression
In many therapeutic
relationships, issues of privilege and oppression exist but are generally not
addressed.
However, clinicians need to
be mindful of the disproportionate risk of adverse health outcomes that exist
for multiple minority populations (e.g., Helminen et al., 2022). These may
manifest as depression, anxiety, substance use, suicide, school dropout, and
general psychological distress and may not be disclosed or easily addressed. Self-compassion
is conceptualized as a way in which personal self-appraisal and response to
one’s own emotional experiences could be an important key to enhancing
self-kindness and mindfulness, and coping with the stress evoked by minority
stressors that may go unaddressed generally as well as in clinical encounters.
Miville et al. (2009, p. 236)
described strategies to navigate privilege, oppression, and gender and they are summarized below:
Addressing and
Resolving Conflicts
1. Resolve conflicts
Gender and multiple identities result in multiple messages about constructing
gender roles, some of which may have been internalized from childhood. Some may
relate to current tensions in language. Stereotypes of empathic, nurturing
females, strong and assertive males, and conflict between individualistic
values, egalitarian roles, and clear sex role definitions may arise.
So in clinical practice, be thoughtful about language with
clients, reflect on one’s own identities and about gender language that is
syntonic with the client. Be reflective about stereotypes that may exist that
are reflective of one’s cultural history growing up, regional differences, and
current language – and be attentive to the client’s own self-designations,
familial issues, conflicts, syntonic language, and their particular phrasing
regarding those issues.
2. Navigate privilege and
oppression
Consider the larger sociopolitical context and the dominant/subordinate
relationships; move toward mutual respect and mutuality within families and
toward others.
3. Understand one’s
impact on others
Internalizing (negative) gender or racist stereotypes may involve enacting
roles that are oppressive and potentially lead to harm; help clients and
yourself critically examine beliefs and consider the consequences of behaviors
and their impact on others to address beliefs and self-images.
4. Transform
self-perceptions
Identify struggles between cultural prescriptions and stereotypes and how those
apply to one’s personal life, expression, and relationships and are manifest in
therapy.
5. Consider
intersectional identities
Consider the full gamut of cultural identities and their intersectionality (APA
2017) (including sexual orientation, religion, socioeconomic status, and
multiple identities).
6. Navigate emotions
Increase awareness of the impact of negative stereotypes and contextual
cultural expectations and norms; learn to navigate one’s own emotions in the
context of societal expectations.
7. Construct (and
reconstruct) roles in family, community, and society
Communicate and uphold responsibility, balancing roles.
Now read this case vignette
and respond to the questions that follow.
Minh,
a 15-year-old Vietnamese-American client, was referred for school failure after
she had been an “A” student but had a difficult break-up with her boyfriend and
felt alienated, devastated, and hopeless. Her grades had fallen precipitously
and her school counselor referred her for therapy to help her recoup before she
lost her chance to get a scholarship to college. Minh’s grandfather was a U.S.
military officer, her grandmother, Vietnamese. They migrated with Minh’s mother
to the U.S. in the 1990s but Minh disclosed that no one talked about her
cultural heritage, and she became even more depressed when she was assigned to
write an essay about personal family history. Minh’s therapist, a Latina, recently
licensed, had attempted to address culture but beyond the one disclosure about
the essay on family history, Minh put her head down and refused to discuss it except
to say it was very depressing and no one talked about anything.
Consider what therapeutic
strategies you might initiate to work with Minh. How would you encourage the
therapist to approach Minh with cultural humility? Consider cultural
opportunities and strength-based approaches including her excellent grade
history, her curiosity and eagerness to find out more, and the information she
already has. Think about your own personal response to Minh’s situation.
Self Awareness
A primary issue in the
multicultural context is self-awareness. Most of the multicultural frameworks
(rooted in the work of Sue, Arredondo, and McDavis, 1992) consider
self-awareness to be an essential first step in the process of becoming more
“culturally competent.” There are multiple deterrents to enhanced
self-awareness including the fact that White therapists may not consider
themselves to have a culture, or if they do, they question whether it is
relevant. There is also disregard of White privilege, and as long as it is
disregarded, the multiple power differentials in the therapy equation are
disregarded. Self-awareness has not traditionally been a part of training
programs. As if therapy were value-free – a premise long discounted – training
programs have not attended to what values, assumptions, and belief structures
each of us brings to our practice of therapy.
A second key deterrent is
resistance to content, i.e., believing there are no differences among ethnic
groups, or feeling a lack of safety in discussing diversity, culture, or trauma.
A third deterrent is
neglecting the concept of ecological niches or diversity as an important part
of the equation. What are ecological niches? Think of all the descriptors that
go into your identity .For example, gender, religion, profession, sexual
orientation, gender identity, culture, ethnicity, socio-economic status, race,
and so forth. It has been speculated that each individual could develop an
“equation” to describe which of one’s niche characteristics are most impactful,
and how they interact. This whole area of discussion requires openness to
discussion and self-awareness of culture and diversity status.
Self-awareness by the
therapist of their personal discomfort discussing any of these topics is critical
and may require consultation or supervision or one could risk strains,
ruptures, and loss of clients in therapy as a result (Adams & Kivlighan,
2019). Further, client comfort or discomfort in disclosing pain, hardship, or loss,
could prevent cultural issues from being discussed.
A strength-based approach is
useful in therapist inquiry about relational stressors including community or
familial supports; openness to indigenous or other rituals, including those for
healing; and attending to individual and family strengths and resilience.
Overlooking any of these could represent missed opportunities for cultural
openings that could facilitate understanding, compassion, and insight.
Understanding the issues of
the multiple generations who migrated leads to assisting with cultural
transitions and balancing generational hierarchies, all too often neglected in
therapists’ conceptualizations. Falicov (2014) describes the complexities of
respecting the hierarchy and strengthening it, as well as the various
viewpoints of different family members. Balancing acculturation with adaptation
and addressing cultural dilemmas requires therapist skill and flexibility. There
are also significant issues of therapist language and cultural competence to
conduct such work.
Clinicians learn critical self-awareness of how power, privilege, culture,
and identity inform both our internal experience and our affective and
behavioral responding in the moment. and our perceptions of others. Therapists
should use wise affect, respond to negative emotions that have potential to
lead to disconnection, and through positive emotions, enhance caring and
connection. This requires
the ability to empathize with the client’s
experience and be sensitive to the ways the interaction and relationship will
be shaped by dynamics of oppression. Through interpersonal engagement,
empathize with the client’s experience and be sensitive to the ways the relationship
is shaped by dynamics and history. Our behavior, dress, nonverbal
communication, and language all communicate messages that are powerful.
Therapists’ understanding of their own racial identity
and biases are positively associated with clients’ perception of the
therapist’s skills and improves the quality of the therapeutic alliance (Chang
et al, 2021).
Cultural Biases: Confirmation; Implicit Bias
Cultural biases may develop from childhood or from experience and
may be positive or negative, favoring certain individuals, groups, or
identities, or else disfavoring, avoiding, or stigmatizing them. Individuals
are aware of some biases, and unaware of others. Racism and sexism are examples
of these biases.
Among biases which are known to exist are:
- Distance and anxiety
toward difference;
- Implicit cultural
messages;
- Negative past
experiences that inform present behavior;
- Personal cultural
struggles;
- Changes to cultural
identities over time; and
- Cultural biases in the
form of patronizing, overidentification, idealization, failure to challenge
particular behaviors
(Hook et al., 2017)
Therapists are not always rational, dispassionate actors and
evaluators and may use heuristics, rules, or shortcuts that are culturally
bound in making judgments and that result in cognitive bias in decision-making.
Heuristics, or mental shortcuts, may include implicit biases, described as
habits of mind, that have significant potential to affect viewpoints and
evaluations of situations, and those may result in undetected prejudices and
erroneous judgments that may lead to more positive or more negative
evaluations and actions, but in fact may be based on irrelevant factors.
In the instance of confirmation bias, the tendency is to
seek information that conforms to our beliefs. Thus, the clinician interprets,
prioritizes, and recalls information that confirms or supports one’s prior
beliefs or values based on personal life experience. Conversely, this leads to
discounting information that does not conform, so that one selectively attends
to or even seeks out information that confirms an impression, opinion,
or conclusion rather than looking for and attending to that information which
does not.
An example would be a therapist who starts working with a
client, learns that they attended the same high school (although separated by
many years), and works from the assumption that the client had a similar
schooling experience to their own. Even when the client gives the therapist information that is not consistent with the therapist’s
assumption, the therapist persists in that
assumption, confident in their own experience and attending only to aspects
that coincide with it and not being aware of that thinking error.
Tversky and Kahneman (1973) defined the “availability heuristic” as
how vividly and saliently particular social and cultural events and experiences
strongly influence decision-making and even perceptions. The availability
heuristic is a cognitive bias that influences decisions so as to be based on
false perceptions from recent memory. Thus, the most vivid experiences stand
out and influence our perceptions. For example, events drawn from one’s
personal experience are more readily available, so if someone was queried about
frequency of deaths – accidents versus medical conditions such as heart disease – they
might respond “accidental,” having witnessed so many online or on video and
heard about them in news reports. In attribution error, there is the tendency to
place greater emphasis on an individual’s personal characteristics and less
emphasis on social and situational forces when judging behavior. All of these
biases impact our cultural perceptions and relationships.
Cultural biases may emanate
from childhood or life experience. They can be positive or negative. These
include explicit biases, in which individuals are aware of their specific
biases, and they may be negative or positive. They may be reflected in distance
or anxiety toward difference. Implicit cultural messages may be verbal or
behavioral (startling, moving away from). These may have arisen from negative
past experiences, personal cultural struggles, or changes to cultural
identities over time. Cultural biases may take the form of patronizing, overidentification,
idealization, or failure to challenge behaviors.
A cultural bias could also be
the assumption that a client who comes alone to therapy does not want the
therapeutic process to involve family members or others in the therapy, either
in the formulation of the problem or in the sessions, and wants a totally
individualistic approach. Or it could be the therapist discounting the reason
the client says they are coming to therapy, for example when the client says
they just “feel like a failure” to their family, but the therapist frames it
individualistically as depression.
For clinicians, a reflective process and self-awareness are
essential so that recent vivid experience is distinguished from a careful
dispassionate analytic approach that demonstrates distance from emotions and
experience. Biases are introduced by disproportionately attending to certain
rules, failure to adhere to professional boundaries perhaps manifest as
intrusive advocacy, forcing the client to do something the therapist or
supervisor feels is correct, or allowing personal values to trump professional
ones (Knapp, Handelsman, Gottlieb, & Vandecreek, 2013).
Clinicians may rely on
shortcuts or heuristics, that is to say rules or shortcuts in thinking that
have worked successfully over time but may cloak undetected prejudices that
lead to more positive evaluations based on irrelevant factors such as common
experiences or identities or personal attractiveness, as distinguished from
competence or performance (Kahneman & Tversky, 1973). An example of an
anchoring heuristic is that a potential client hears from a friend that her
therapy costs $40 an hour so when the potential client hears that the therapist
she is considering costs $100, she has “anchored” her idea of fees to $40, not
considering the quality or training of the therapist or reports of efficacy. Another
example, the familiarity heuristic, relates to the tendency to have more
favorable opinions of places or people one has experienced previously, as
opposed to new, unfamiliar ones.
Kahneman and Tversky (1973)
found that by requiring interviewers to consider a series of specific
attributes of job applicants separately, evaluating individual characteristics
independently rather than making a holistic judgment about the person, resulted
in more accurate and reliable judgments with less variability.
Microaggressions
Sue and colleagues described
racial microaggressions as “the everyday slights, insults, put-downs,
invalidations, and offensive behaviors that people of color experience in daily
interactions with generally well-intentioned White Americans who may be unaware
that they have engaged in racially demeaning ways toward target groups (Sue et
al., 2007), (Sue et al., 2019, p. 129). Microaggressions have been identified
and discussed targeting multiple minority populations including women,
LGBTQIA2S+ (lesbian, gay, bisexual, transgender and/or gender expansive, queer
and/or questioning, intersex, asexual, and two-spirit), ethnic minorities
including Asian-Americans and Latino-Americans, individuals who have immigrated
from any country, religious group members, to name a few. Microaggressions have
also been identified as frequent occurrences in clinical settings, in therapy
sessions, both individual and group, and in clinical supervision. Although as
Sue and colleagues describe, many downplay the significance and impact of
microaggressions, in fact they inflict substantial harm both on the intended
recipient, and also on the setting in which they occur, creating a toxic work
environment. They are actually “macroacts of bias and discrimination” (Sue et
al., 2019, p. 130). Microaggressions are traumatizing.
Sue (2010) gave examples of
microaggressions that include a faculty member of color being mistaken for a
service worker, an example of a theme of being a second-class citizen, or when
race is brought up in classroom discussion, asking a student of color “Why are
you always so angry?”
Therapists may inadvertently
use microaggressions in their work with clients. These include statements that
seem oblivious to racial or other identity tensions, making jokes or comments
that are offensive to women or to diverse groups, or generally being dismissive
of identity factors in interactions and psychotherapy with clients who are
Black, Indigenous, or women of color (DeBlaere et al., 2022) among many others.
These comments were more frequently heard from White therapists, and their impact
may be moderated by attitudes of cultural humility.
Kivlighan et al. (2021)
reported that 72% of their 71 ethnic and racial minority clients in 38 therapy
groups reported at least one racial microaggression during their group
therapy – and they reported those were associated with low cultural comfort among
those clients.
When microaggressions occur,
they tend to be normalized or overlooked, but they create an environment of
disrespect and invalidation.
Sue and colleagues (2019)
described the harm done when these microaggressions – which are actually
“macroaggressions” – occur and suggested none are “micro”. Those who hear them
are either targets, allies, or bystanders. Targets are the object to whom
prejudice, and discrimination are directed. Allies are members of dominant social
groups and have the power to move toward eradication of prejudice. Bystanders
may be well-intentioned but may anticipate negative reactions to their responding
and so step back.
To directly address the
aggressions, Sue and colleagues (2019) suggest micro interventions which
include:
(a)
make the invisible visible, challenging the stereotype, asking for
clarification, and circulating literature or soliciting feedback from others;
(b)
disarm the microaggression by expressing disagreement, interrupting, or
redirecting;
(c)
educate the perpetrator by appealing to the individual’s values and principles,
instituting long-term mandated training; and
(d)
seek external reinforcement or support.
However, such findings are
indicative of the urgent need for more training, reflection, and cultural
humility in all clinical interactions. Self-assess your use of
microaggressions – through the lens of the client. Jokes or throw-away comments
may be microaggressions.
Consider possible responses
when you hear a microaggression from a colleague. Which micro-intervention
might you use? What would stop you from using one? How could you increase the
probability of using a micro-intervention?
Cultural humility is one
intervention to mediate negative effects of microaggressions within the therapeutic
relationship (DeBleare et al 2023).
Identities and
Intersectionality
The frameworks of both
Falicov and Hays offer strategies to examine the places of power and privilege
held by the therapist. In her book Connecting Across Cultures: A helper’s
toolkit (2012), Dr. Hays provides a series of questions which have the
therapist engage in introspection and curiously investigate their own
identities and privileges. From these questions, the individual designs what
Hays coins as a “culture sketch.” Adapted from her ADDRESSING multicultural
framework, the culture sketch brings forth the complexity of social-cultural
variables and helps bring awareness to places where a mental health provider
may hold privilege in cross-cultural interactions with clients (Hays 2012).
As stated previously, the construct
of “intersectionality” is derived from the work of Kimberle Crenshaw (McCall,
2015) and represents the constellation that race, ethnicity, gender, gender
identity, sexual orientation, socio-economic status, religion, spirituality,
disability/ableness, and other identity dimensions and statuses are social
constructions that collectively encompass human identities. Intersectionality
refers to proactively integrating the multiple identities and their resultant
privilege and oppression to amplify understanding of context, mental health,
and effective intervention.
Internalized stigma or “isms”
can result in prejudice, stigma, and negative mental health outcomes. Unfortunately,
multiple identities and their intersections have been generally neglected in
training, literature, and practice.
Among those neglected are gender
variant nonbinary and transgender identities. Recognize that a binary
expectation generally exists from the time a client contacts a mental health
provider or setting. Generally, intake forms include “male/female” choices; in
some settings there is “other.” Consider your own forms and ways of greeting
potential clients. Consider whether you identify and disclose your own
pronouns.
Binary refers to
classification of gender into two distinct and opposite forms of masculine and
feminine, whether determined by social system, cultural belief, or other
factors in combination. One’s gender identity and sexual orientation are
unrelated. Transgender and gender variant affirmative counseling and
psychological practice needs to be current, culturally relevant, responsive to
the client and the multiple social identities, addressing social inequities,
enhancing resilience and coping, advocating to reduce systemic barriers to
mental and physical health, and building upon client strengths (Singh &
Dickey, 2017). Cisgender refers to those whose gender identity corresponds with
the sex registered for them at birth.
Generally, a binary worldview
predominates. That is, individuals are perceived as either male or female. For
example, asking if one was “born a boy or girl” reflects the therapist’s binary
orientation. Further, a total or “laser” focus on gender identities ignores
other intersectional identities such as race, ethnicity, religion,
spirituality, socio-economic status, migration and immigration status,
disability or ableness, examples of intersectionality, considering multiple
identities and their interactions.
Sex is assigned at birth and
is binary, generally relating to anatomy. Gender refers to social constructs:
roles, behaviors, activity choices, etc., that society considers appropriate.
Sexual orientation refers to a pattern of emotional, romantic, and/or sexual
attraction of men to women or women to men (heterosexual), of women to women or
men to men (homosexual), or by men or women to both sexes (bisexual). It also
refers to an individual’s evolving sense of personal and social identity that
is based on attraction, related behaviors, and, potentially, membership in a
community of others who share those attractions and behaviors. Nonbinary refers
to people whose gender does not fall within binary categories of man and woman. Thus the term “nonbinary” refers to individuals who do not define themselves
as either “male” or “female.” It can be expressed as an absence of gender,
presence of multiple genders, or as gender expansive, not fitting neatly into
any category.
Pronouns for nonbinary
individuals may include they/them/theirs, or alternate between she/her/hers and
he/him/his.
Sexual orientation and gender
identity are not the same. Children generally identify their gender between the
ages of three and five. Gender identity refers to a person’s internal
sense of identified gender; gender expression refers to how an individual communicates
gender identity to others through their behavior, dress, presentation, voice,
or bodily characteristics. “Trans” may be used as shorthand for “transgender,”
referring to individuals whose gender identity or gender expression does not
correspond to the sex they were assigned at birth. Gender nonconforming also means not conforming to the
gender identified at birth. Some clients may use an “in-between” or other terms
not within the gender binary, for example, “genderqueer.”
Sexual orientation refers
to one’s consistent physical, romantic, and/or emotional attraction to another
person, whereas gender identity refers to one’s internal and individual
experience and expression of gender. Gender expression is how a
person publicly expresses or presents their gender: behavior, appearance such
as dress, hair, make-up, body language and voice. A person’s chosen name and
pronouns are also ways to express gender.
Clients and therapists alike
may not disclose gender identity or other identities due to concern about
stigmatization or pigeon-holing – assuming aspects of identity that are not
accurate or due to multiple situational, political, or other factors. Further,
“cisgender” or denoting a person whose gender identity corresponds with the sex
registered for them at birth, generally is associated with privilege in many
settings and interactions. In the case of children or individuals who request
the use of pronouns that differ from those assigned at birth, or who already use
pronouns that differ from those assigned at birth, who often encounter
stigmatization and social oppression, and who may identify as trans or gender-diverse,
the therapist needs to self-assess their own training and general orientation
toward binary and nonbinary designations.
Disclosure of one’s personal
pronouns is an important practice. Failure to use the client’s pronouns is
perceived as a signal of not being respectful or inclusive in gender identity. Consider
your own setting(s) and use of personal pronouns. Consider situations when
pronouns have been misused or disregarded and the impact of that on the
individuals. Also consider whether gender identity is simply ignored and the
message that is communicated by that. “Misgendering” refers to using language
or pronouns that are not accurate for gender.
Frequent
heterosexist and gender microaggressions or macroaggressions occur. LGBT
trainees report infrequent discussion of cultural diversity and downplaying or
disregarding the importance of sexual orientation and other intersectional
cultural identities/considerations (Hagler, 2020). No microaggressions are
acceptable in a clinical or training environment as they connote disrespect,
bias, and a lack of safety.
The
intersections of LGBT and religion are increasingly challenging and complex, as
sexual minority individuals may experience conflict among family members, across generations, their
religion, and their sexual orientation. This may result in a combination of
withdrawing from formal religion, escalating family conflict, and distress.
Resources are available
The American Psychological Association (APA, 2021) – APA Guidelines for
Psychological Practice with Sexual Minority Persons
A Guide for Understanding
Supporting, and Affirming LGBTQI2-S Children, Youth, and Families
Guidelines for Affirmative
Social Work Education, (Craig et al., 2016)
AAMFT Gender Identity
Racial and Ethnic Diversity Trauma
Directly
related to the therapeutic relationship and to worldviews associated with
clinical assessment and treatment, is knowledge and competence with respect to
racial group membership, exposure to racial trauma, including prejudice and
discrimination (Pieterse, 2018). Membership in a particular racial or ethnic
group has led to job loss or rejection, loss of opportunities, and painfully
incorrect assumptions. Much of the trauma literature has omitted mention of
these forms of trauma. Some issues to address – and to self-assess on – are how you
identify and approach racial trauma. Consider the example of the BIPOC and/or
religious diverse supervisee who comes to you to tell you her client used
pejorative racial/ethnic language in session. It was not directly aimed at them
but was very hurtful. Or the client discloses that they felt disrespected by
office staff. Or they describe their own personal history of trauma that was
evoked by the client or staff. Pieterse (2018) suggested some possible
approaches:
- Acknowledge/validate
the experience;
- Do not
challenge the client (or staff employee) but accept it as a valid perception; empathically
acknowledge, normalize;
- Assess
the impact on the client, empathic validation, assist in enhancing coping
strategies;
- Contextualize
in terms of what you know about the client’s history, trauma;
- Work
with/address cognitive distortions; address the harmful effect of self-blame;
- Process
strong emotions; approach nonjudgmentally, supportively;
- Respond
to loss of health, possessions, trust, sense of self; and
- Consider
strategies for coping and resistance.
If in fact,
the situation is related to clinic staff, it is critical for the therapist to
address this within the proper setting.
Mental health
professionals are strongly encouraged to engage in processes such as acknowledging
and addressing traumatic stress resulting from racism; being informed and
knowledgeable about the nature of racism; and engaging in ongoing self-evaluation
as part of creating an anti-racist clinical practice. ( Pieterse 2023)
With continuous
self-examination and exploration of implicit bias, therapists can best position
themselves to be effective in cross-cultural interactions with clients
In 2021, the
American Psychological Association (APA) established
a standard definition of racism and issued a resolution apologizing for their role in “Promoting,
Perpetuating, and Failing to Challenge Racism, Racial Discrimination, and Human
Hierarchy in U.S” (APA 2021)
As you read through the
resolution, what thoughts and reactions do you notice? What are clinical
practices that you can adopt into your work that reflect some of the
commitments mentioned in this statement?
Dealing with
Racism-related Stress and Racial Trauma when Working with Clients of Color
Pieterse and colleagues
(2023) provided invaluable guidance for working with racism-related stress and
racial trauma when working with clients of color. Experiences of racism are
identified as having the potential to result in traumatic stress reactions, a
fact generally overlooked by mental health professions but one that has been
borne out by multiple research and experiential studies. Experience of racism
is a traumatic event that may be “chronic, cumulative, and intergenerational”
(p. 2) and may be passed to future generations in multiple ways including
through storytelling. The authors note that not all race-related events may be
traumatic, but those that are negative, sudden in occurrence, and
uncontrollable have significant potential to be. For the therapist, awareness
and self-awareness are critical first steps toward acknowledging that racism is
traumatic and is associated with significant mental health outcomes including
anger, anxiety, and depression. Further, racism and racial oppression are
violence, but these are easily overlooked as a causative factor in mental
health diagnosis and conceptualization. Thus, it is essential to ask and
understand what has happened to the client in their experience of racism and
oppression. Racial oppression may be overlooked, but minimizing or ignoring it
is a form of retraumatization. Pieterse and colleagues urge clinicians to move
from conceptualizing what is wrong with the client to considering what events
have occurred/what has happened to the client.
In describing a facilitative
process, Pieterse and colleagues proposed that clinicians must be courageous in
addressing race and racial impact. The clinician must be attuned and ready to
address racial misunderstandings and potential microaggressions that may occur
in the client-therapist interaction or those that are reported to the therapist
by the client. They urge immediacy, addressing in the moment dynamics and
interactions. Attention to the therapeutic alliance is essential, attending to
its formation, goals, tasks, and power and privilege. The authors identify the
high rates of racial microaggressions and other misunderstandings that occur
and their potential for rupture without dedicated repair.
Essential components are
cultural humility, empathy, and empathic validation, marked by efforts to
empathize and contextualize experience and to engage in therapeutic empathy,
trying to see through the client’s lens of experience.
Specific techniques for
facilitative processes include enhancing adaptive coping to racial events
utilizing mindfulness focused on stress reduction, empowerment, supporting and
validating the impacts and potential shame associated with racial trauma. They
also suggest the approaches of processing of racial trauma through empathic
attunement and seeing the traumatic events through the lens of the client.
Strategies to assist the
client in moving forward include empowerment, generally reframing from victim
to survivor, enhancing a sense of agency or the power to be proactive. Also a
strategy generally is to elevate anti-racism, and for professionals to decenter
Eurocentric and Western approaches, including and valuing writings and
practices of racial and cultural communities that were marginalized through
colonization.
Social Justice
Social justice refers to
increasing well-being among marginalized communities, decreasing social
inequities, and promoting and enhancing human values of equality and justice by
facilitating removal of barriers to opportunity and well-being.
Self-awareness is a complex
competency, including a requisite self-understanding of personal identities, values, beliefs, biases, personal privilege,
motivation to learn about culture and cultural worldviews, identification
and understanding of oppression, marginalization, prejudice, and health
disparities; employing skills of cultural humility, self-awareness, and the
knowledge, skills and attitudes requisite to serve myriad diverse client
populations.
Social justice is a core
value of the profession of social work, including advocacy to decrease human
suffering and to promote human values of equality and justice, and is a significant aspect of psychology counseling
programs. Social justice is defined as the “process of acknowledging systemic
societal inequities and oppression while acting responsibly to eliminate the systemic oppression in the forms of racism, sexism, heterosexism, classism, and other biases in clinical practice both on individual and
distributive levels” (Odegard & Vereen, 2010, p.
130). An understanding of social justice encompasses privilege and oppression, marginalization,
educational disparities, unintentional educational practices, cultural
worldviews, unequal opportunity, and inequities in all realms.
Individually,
persons have multiple identities, intersections of privileged and marginalized.
Thus, there is intersectionality between multiculturalism and social justice.
In
a study of how individuals developed a social justice orientation, counseling
psychology students and professionals identified critical incidents that
influenced them: the influence of significant persons (mentors, parents, family,
and peers) with mentors who introduced them to integrating social
justice into research and academic studies, and families and classmates who
fought for social justice and modeled the behavior for them. Exposure to
injustice, oppression, loss of privilege – personally or by witnessing critical
events – were associated with supporting development of social justice in their
orientation by increasing/deepening their awareness of injustice and
solidifying their commitment to a social justice agenda (Caldwell & Vera, 2010).
For
clinicians, an understanding of the requisite attitudes, values, frame, and
context of social justice is a competency. It requires self-knowledge of one’s
own identities and privilege; self-awareness of one’s impact on others,
including clients; attention to the clients’ worldviews, for example referring
to Falicov’s model and
understanding the role of therapist as advocate, assisting the individual or
family with interpersonal,
institutional, community, public policy advocacy efforts, referrals, and support. For example, interpersonal
might include food or housing referrals or childcare resources. Others might
involve advocacy to impact local, state, or national policy for homelessness,
hunger, poverty, or the mentally ill.
Microaggressions are another
manifestation of verbal and behavioral cues that recreate and serve to
reinforce discriminatory and oppressive social patterns (Owen et al., 2014) and
inflict pain. Microaggressions include derogatory remarks denigrating culture,
and assumptions of financial or other limitations due to identity. Examples are
assuming a client cannot afford to buy a book or object relevant to therapy, or
surprise when a diverse client possesses a doctoral degree. High numbers of
microaggressions occur in group therapy (Kivlighan, Swancy, Smith, &
Brennaman, 2021). Microaggressions include avoidance of or minimizing relevance
of cultural issues or use of cultural stereotypes, even if unintentional (Owen
et al., 2016). Microaggressions cause strain or ruptures, and the therapist may
lack awareness of the source. Chang and colleagues (2021) discuss the
phenomenon of White clients challenging BIPOC therapist credentials as a
reflection of cultural stereotypes that such therapists are less qualified or
are affirmative action hires.
Cultural mis-attunement may
occur when clients share meaningful, cultural, emotionally laden experiences only
to have the therapist minimize or ignore the disclosures or turn inward and
talk about their own emotional experience, deflecting from the client. Or when
a BIPOC client is described as “angry” and the therapist addresses that anger
purely as a behavioral phenomenon and deals with strategies to manage anger
rather than addressing the underlying cultural milieu in which the anger is a
survival strategy against a lifetime of oppression.
Emotional expression is
another cultural variant. Self-awareness of the cultural nuances of
relationship and communication in providing therapy is essential. Self-awareness
includes awareness of our own identities and use of Falicov’s graphic to
consider our attitudes, privilege, perceived power, and culture and how these
impact our attitudes and behaviors toward our clients – and toward perceived
difference and sameness. Self-awareness extends to identifying personal
emotional response to clients and attending to that, obtaining consultation as
indicated, identifying feelings of discomfort, or other responses that arise.
Trina
and Joseph are a heterosexual married couple who have been together for
approximately six years. They recently started experiencing difficulties in
their relationship due to what they describe as “poor communication.” During
the intake session, Joseph expresses his concerns about their frequent
arguments that often escalate into heated conflicts. Trina agrees and states
that she wishes they could talk calmly without getting into screaming matches.
She begins to detail a recent fight they had in which Joseph yelled at her.
Joseph immediately gets upset and says firmly “I was not yelling.” As Joseph
begins to speak you notice tension in your own body increasing. Trina and
Joseph also notice the change and Trina comments “See, you’re even upsetting
the therapist.”
In this example it would be
important to attend to not only the discrepancy in the couple’s characterization
of the fight, but also the reaction that you noticed in your own body during
the session. It would be important to inquire about what, if any, family norms
or experiences in the couple’s childhood history inform their individual
communication and conflict resolution style. Increased understanding of what
messages they received about expression of emotion could help inform what
clinical approach you use and what potential interventions to introduce to the
couple. Finally, attending to your reaction and exploring whether you were
reacting to Joseph’s specific comment, the rise of tension between the couple,
or a recent fight you had with your partner would be the first step in
addressing the possible cross-cultural interactions showing up within the therapy.
Essential components to
address ruptures include: Identification of client response and withdrawal and the
ability to address these in an empathic manner; accurate self-awareness of the impacts
of power, privilege, and culture on perceptions and relationships with clients;
self-awareness of negative emotions and empathy to manifest toward clients and
difference; ability to empathically engage without becoming defensive or
withdrawing emotionally from difference and oppression; and moving forward to
repair and be present with the client in the moment to process the event(s),
impacts, and the relationship moving forward.
International
Worldviews impact every
aspect of our perceptions and relationships with clients and others. Consider
two dimensions that define our view of culture. First is unilateral
globalization, based on belief in the superiority of one’s own culture, values,
and ideals, and imposing that standard on all individuals and cultures – one
culture dominates and subjugates others.
In contrast, enlightened globalization is based on
understanding, dialogue, respect, integrating knowledge to foster cultural
development, with recognition that each culture has a different set of values,
beliefs, skills, and resources (Kim & Park, 2007).
Colonialism is a result of
unilateral globalization. Colonialism is a confluence of profound negative
social and emotional consequences that result when one ethnic or cultural group
subjugates another. Colonization refers to processes whereby a country or group
transports and implants settlers in another country with the aim of domination.
Results include loss of original inhabitants’ tribal lands, their traditional
ways of economic support, destruction and degradation and then loss of social
patterns, traditions, power, roles, self-respect, loss of language, cultural
practices, autonomy, self-determination, and cultural mores.
And there is simultaneously, an
elevation of the mores and power of the dominant Western European groups
(Hernandez et al., 2010; Hernandez-Wolfe, 2011) and their cultural mores which
are in sharp distinction from those of the country being overtaken and
dominated. The domination is divisive, resulting in subjugation,
dehumanization, and a loss of culture.
Attention is being devoted to
mental health systems through the lens of colonization. Significant losses
described which are highly relevant for clinical practice are those of
well-being and spirituality. Further, recognition of our own privilege helps to
foster humility (Hernandez-Wolfe, 2011) and compassion in our work.
Multicultural
Theoretical Orientations
As other disciplines such as
political science and law bring attention to greater understanding of how
systemic racism, discrimination, and marginalization affects individuals,
families, and social institutions, the mental health field has also
incorporated these concepts into multicultural frameworks that offer clinicians
alternative strategies to understanding of effective clinical treatments
tailored to meet the needs of diverse populations. Feminist theories and
Relational Cultural Theory (RCT) are two examples of such multicultural
theories.
Feminist
theory assumes a perspective which aims to understand how gender influences the
client’s experiences and shapes their beliefs and behaviors. These Feminist
theories and their application in psychological practice grew from the Women’s
Movement in the 1960s because of concerns that traditional psychotherapies did
not adequately acknowledge or address gender and social-political issues that
differentially affected all persons, but women in particular. During this time
there was a surge of collective theories, concepts, and ideas that began to
note the absence of consideration of gender in the conceptualization and understanding
of social systems and human behavior. Consider the impact of the intersection
of gender and culture on the development and well-being of individuals and how
it continues to evolve. Feminist theories are broadly applied to a variety of
clinical issues including trauma and sexual abuse, with a central focus on
understanding how social and cultural norms influence the presentation of
clinical issues such as eating disorders and trauma, particularly in response
to gendered violence and personal identity.
As a theoretical framework, feminist theory emphasizes
the intersection of gender and culture in the development of the individual
(regardless of gender identity). There is also consideration of how social and
political constructs such as discrimination, oppression, and sexism impact our
clients and it offers strategies for addressing that in treatment. While there
is no unified definition of feminist theory, there are underlying principles
that guide the use of it in clinical practice.
The four clinical components (Israeli & Santor,
2000) of feminist theory include:
Additional
guiding principles of feminist theory highlight its attention to social
justice, empowerment, equality and inclusion:
- The personal is political; and
- Commitment to social change
There are four approaches to
feminist theory (liberal feminism, cultural feminism, radical feminism, and
social feminism) that can be applied to case conceptualizations (Draganovic
2012).
Black Feminist Counseling Theory
Black feminist theorists explore the specific and
unique challenges faced by Black women which should be integrated into
psychological theory and practice. Three specific strategies informed by Black
feminist theories include the use of critical affirmations, raising black
consciousness, and intentional self-definition (Oliphant et. Al, 2022)
Mujerista Counseling Theory
Womanist theory focuses
on BIPOC communities while Mujerista theories focus on experiences of
Latinx women. Mujerista is a term that emerged within Latinx communities to
describe a feminist perspective that is centered around the experiences,
struggles, and liberation of Latina and Hispanic women. As a feminist theory,
it emphasizes intersectionality, cultural identity, and social justice in
understanding how systems of oppression uniquely affect Latina and Hispanic
women. Both in theory and practice, Mujerista recognizes the
interconnectedness of different forms of discrimination and advocates for
political and social change.
Relational Cultural Theory
(RCT)
As a multicultural theory,
RCT complements the multicultural/social justice movement by (a) identifying
how contextual and sociocultural challenges impede individuals’ ability to
create, sustain, and participate in growth-fostering relationships in therapy
and in life and (b) illuminating the complexities of human development by
offering an expansive examination of the development of relational competencies
over the life span. (Comstock et al, 2008).
Embedded within RCT are seven
core tenets (Comstock et al, 2008) that anchor clinical case formulation in an
understanding of human development. RCT centers the role of relationships as a
measure and function of psychological wellness. This premise operates from a
collectivist perspective that is more culturally congruent than some other
theoretical perspectives. Review the seven tenets and consider with what client
populations this conceptual framework could be useful:
1. People grow through and toward
relationships throughout their lifespan.
2. Movement toward mutuality rather
than separation characterizes mature functioning.
3. The ability to participate in
increasingly complex and diversified relational networks characterizes
psychological growth.
4. Mutual empathy and mutual
empowerment are at the core of growth-fostering relationships.
5. Authenticity is necessary for real
engagement in growth-fostering relationships.
6. When people contribute to the
development of growth-fostering relationships, they grow as a result of their
participation in such relationships.
7. The goal of development is the realization of
increased relational competence over the life span.
Treatment Considerations
While there is consensus
that attending to socio-cultural and individual factors will enhance treatment
outcome, there continues to be ongoing discussion in research literature
regarding cultural adaptations of diverse clients. Researchers and treatment developers
have long been criticized for neglecting cultural variables in both treatment
development, design, and evaluation.
A 2008 review of effective
treatments for ethnic minority youth (Huey & Polo) highlighted the
importance of therapist knowledge and skills in cross-cultural effectiveness as
enhancing treatment outcomes for ethnically diverse youth. This meta-analysis
primarily focused on reviewing the impact of the cultural adaptation of EBTs (evidence-based
therapies) for ethnic and racial minorities in enhancing treatment outcomes.
Their work highlights the importance of considering cultural factors such as
values, beliefs, and traditions when designing and implementing EBTs. The
researchers indicate that failing to consider socio-cultural variables,
including acculturation status, can result in inaccurate diagnosis, less
effective treatment, and a lack of engagement from individuals from diverse
cultural backgrounds.( Huey et. al. 2014)
A ten-year follow-up to the
review of psychosocial treatments for ethnic minority youth revealed that there
remains few evidence-based treatments, specifically for Asian and Native
American youth (Huey et. al. 2019).
One such treatment model is
Brief and Strategic Family Therapy (BSFT) developed by Jose Szapocznik. Szapocznik’s pioneer model is one that built upon
systems therapy in the 1970s and 1980s primarily with Cuban American families.
This model was created for specific attention to cultural norms, values, and
clinical issues for Hispanic youth and families, specifically Cuban American
families. One unique aspect of this model is
that he added a bicultural effectiveness
training which made the acculturation elements of the population intended for
the intervention more explicit than in other treatment models. Acculturation
dynamics were central to the model.
There is general recognition
that Cognitive Behavioral Therapy (CBT) treatment approaches were developed in
Western countries and reflect that strong cultural bias. As Falicov (2014) and
others describe, multicultural factors are central to identity in all cultures.
Cultural ruptures occur frequently in psychotherapy. They can result from
affective mis-attunement including failure of empathy or misunderstanding
occurring through a cultural lens, misunderstandings which may or may not be
recognized, relational disconnects relating to cultural mores or
misunderstandings, or relational disconnects or misalignments resulting in
strains or ruptures (Chang, Omidi, & Dunn, 2021). Chang and colleagues
state that understanding of clients is difficult and elusive, and often
therapists misunderstand while believing that they can understand the processes
of socialization. However, those misunderstandings occur through differential
socialization and assumptions based on personal processes and through lenses of
privilege versus internalized oppression. These internalized scripts become
automatic and are enacted without conscious awareness. They foster strains and
ruptures and generally disconnect any potentially internalized oppression. Therapists
then impose cultural, racial, or sexual stereotypes on clients without
conscious awareness they are doing so. These may be represented in assumptions,
language, or attitudes.
Clinicians are encouraged to
identify strategies that will allow them to consider unique needs of diverse
groups while also implementing treatment modalities in a manner that maintains
fidelity to the clinical model. Several authors provide guidance on culturally
informed strategies to effectively integrate culture into evidence-based
treatments. Pamela Hays (2009) outlined the following 10 steps that can be used
when integrating a multicultural framework into CBT:
- Assess the person’s and family’s
needs with an emphasis on culturally respectful behavior.
- Identify culturally related
strengths and supports.
- Clarify what part of the problem is
primarily environmental (i.e., external to the client) and what part is
cognitive (internal), with attention to cultural influences.
- For environmentally based
problems, focus on helping the client to make changes that minimize stressors,
increase personal strengths and supports, and build skills for interacting more
effectively with the social and physical environment.
- Validate clients’ self-reported
experiences of oppression.
- Emphasize collaboration over
confrontation, with attention to client-therapist differences.
- With cognitive restructuring,
question the helpfulness (rather than the validity) of the thought or belief.
- Do not challenge core cultural
beliefs.
- Use the client’s list of
culturally related strengths and supports to develop a list of helpful
cognitions to replace the unhelpful ones.
- Develop weekly homework
assignments with an emphasis on cultural congruence and client direction.
In contrast, Falicov would
want to know more about the ecological context and stressors, family
constellation, relationships, and relationship to culture. In practice, essential
are demonstrating curiosity and respect, culture-specific adaptation, and
transformation of theories such as attachment and individuation. Regarding
social justice, attention is given to power differences and contextual
stressors tied to gender, sexual orientation, gender identity, race, social
class, and minority status. And in practice, empowerment, cultural resistance,
social action, and legitimization of local knowledge are critical.
So for Falicov, focus is on
intersectionality, context, relationships, and approaching clinical work with
respect, curiosity, reflection, and openness. (Falicov, 2014, p. 28)
A recent article (Huey et al,
2023) expanded upon Hays’ work to explore what, if any, adaptations are needed
to ensure integrity and effectiveness of Cognitive Behavioral Therapy with
diverse populations. This work continues to support the efficacy of CBT for
culturally diverse groups while emphasizing the need for clinical training in
both cultural competence and evidence-based strategies for cultural adaptations
(Huey et al., 2023). It is important to consider not only adaptations made to
treatment outcomes but also the role of therapists receiving training in
cultural competence in order to improve treatment efficacy with diverse clients
(Huey, 2014).
While the literature on
culturally sensitive EBTs remains lacking (Huey et al., 2023), there is
emerging support for personalized psychotherapy tailored for the individual.
The personal relevance of the psychotherapy (PROP) model proposed by Hall et al.
(2021) is one strategic method to integrate and account for the dimensions of
culture outlined in this course. Within the PROP model, clinicians are
encouraged to consider individual, group, and universal factors that are
relevant not only in the development and diagnosis of psychopathology, but also
in selecting and implementing treatment intervention. As an illustration, read
through the following vignette and respond to the following questions.
Kai is a
20-year-old gay Asian cisgendered male who seeks services at his university
counseling center. At intake, he reports that he feels depressed and is
experiencing a significant amount of stress about school, commenting that he’ll
“probably flunk out.” He has a 2.0 GPA and has experienced a significant
decline in his grades over the past year. He spends much of his day in his dorm
room playing video games and has a hard time identifying what, if anything, is
enjoyable in a typical day. He rarely attends class and has avoided reaching
out to his professors to try to salvage his grades this semester. Kai states
that since elementary school he has always been “shy” and had trouble making
friends. He does report having a very small and cohesive group of friends from
elementary through high school that he met mostly at church. He indicates that
his level of anxiety significantly amplified at the start of the COVID-19
pandemic. When meeting new people, he has a hard time concentrating on the
interaction because he is busy worrying about what they will think of him,
often assuming that they will find him “dumb,” “boring,” or a “loser.” When he
loses his concentration, he stutters, is at a loss for words, and starts to
sweat, which only serves to make him feel more uneasy. After social
interactions, he replays the conversation over and over again, focusing on the
“stupid” things he said. Similarly, he has a long-standing history of being
uncomfortable with authority figures and has had a hard time raising his hand
in class and approaching teachers. Since resuming classes in person, he has
increased his isolation from peers, turning down invitations from his roommate
to go eat or hang out, ignoring his cell phone when it rings, and habitually
skipping class. As summer approaches and he prepares to return home to his
family, he is seeking help to let his parents know that graduation will likely
be delayed.
In considering possible diagnoses, what are the
individual behaviors and symptoms displayed by Kai that inform and clarify
diagnoses? He shows some signs of anxiety and depression. Some of those
symptoms possibly were exacerbated by the COVID-19 pandemic and others may by
culturally congruent.
In what way does Kai’s early history, age, gender
identity, sexual orientation, and his current status as a college student add
to your understanding of the salience of these behaviors in his overall health
and well-being? As a college student, he is in a developmental stage of life in
which socializing with peers, identity formation, and experimentation with
different identities are normative. The amount of social isolation that he
describes is not only possibly emblematic of a psychiatric disorder, it is
developmentally incongruent for his age.
What do you identify as priority targets of treatment
according to how Kai is presenting and his reason for seeking services? What
additional information about Kai, his family and his social support system is
important to know before determining possible intervention? Some of Kai’s
symptoms are culturally congruent so it would be important to first consider
potential impact of targeting behaviors that someone from a different cultural
perspective would assess as problematic yet may not be a source of distress for
Kai and his family of origin. A therapist errs if their targets of treatment
are inconsistent with his cultural norms and expectations of his community.
While we know that generally CBT is an effective
treatment for anxiety and depression, would specific traits that Kai displays such
as distorted thoughts and ruminations help determine if CBT is indicated or
contraindicated for him? Before initiating services, a clinician would also
need to consider aspects of his current setting and family life that could
impact treatment and need to be modified or adapted. Other universal factors to
consider would be what group cultural values or norm should be integrated into
treatment.
In Falicov’s model, the
therapist focuses on relationship, on current stressors and strengths,
approaching Kai with curiosity and respect, increasing understanding of his
family of origin, the onset of his school difficulties, the relationship of
those to his family constellation and peer group so as to understand the onset,
precursors, and current impact of the actions he feels he must take, how his parents
have responded previously, identifying patterns of avoidance and their efficacy
short and long-term, general parent-client dissonance, COVID-19, and their
impact on his presenting problem. The therapist would identify and address
family roles, boundaries, avoidance as coping, and imbalances that have arisen
through Kai’s college trajectory that may have been rooted in family
relationships and patterns that have become increasingly less adaptive with
maturation. The therapist would explore the role of the church, how impactful
that had been, and what resources he has available to use religion,
spirituality and the church currently, as well as other positive coping to
enhance the client’s personal agency and control which could positively
influence his life.
Identifying and applying an
evidence-informed approach can provide a roadmap of how to deliver culturally
congruent and effective treatment for diverse populations.
Meredith
is a 52-year-old divorced Black female. She lives alone and works in sales. She
has a 24-year-old daughter that she has a strained relationship with and rarely
sees. She comes to therapy seeking assistance for workplace harassment. She has
been employed with her company for 18 months and was recently placed on a
Performance Improvement Plan due to decline in her sales. She works remotely
and only goes out into the field to make customer visits. She believes the
write-up was racially motivated. She denies a previous history of mental health
issues. She reports an increase in depression and anxiety since the
disciplinary action from Human Resources. She is having trouble concentrating
at work and has canceled several meetings with her supervisor. She states that
she is usually a happy person, but the work situation has changed her mood. She
indicates that she is isolating from her friends and not spending time outside
of her home. As part of your clinical intake, you provide her with PHQ 9 and
GAD 7 to complete, however she neglects to finish them each week.
As you prepare to consider a
diagnosis, consider what cultural factors impact symptomatology and possible
diagnoses.
In generating intake questions to
help develop a culturally informed case conceptualization use DSM 5 Cultural Formulation
Interview to develop a list of questions and considerations for this client:
What is found when considering social,
cultural, and contextual variables in symptom presentation?
What are cross-cultural factors
that you must take into consideration for you in your work with this specific
client?
How do you as a therapist approach
this client from a place of cultural humility in a manner that establishes
trust?
In
your third session, Meredith reveals that she was terminated from her previous
job for frequent absences and poor work performance. She reports that her
absences were secondary to a vehicle motor accident which involved her and
another motorist. She reports having similar symptoms and difficulties at work
now that she had after her accident.
A
month after she was placed on a workplace performance improvement plan, she
applied for short term disability but was declined. Since then, she is asking
you for assistance with filing an appeal as well as a complaint to her current company
about racial discrimination.
How do you respond to this
client’s report of racism?
What strategies do you use to
address racism in psychotherapy with the client?
How does the therapist
balance legal, ethical, multicultural, and clinical aspects of treatment? What
personal factors of the therapist will impact treatment? Do you consider the
role of cultural consultation from a peer or previous supervisor in order to enhance
treatment?
Summary
Attending to the varied
aspects of diversity and multiculturalism is a critical aspect of psychotherapy
that improves and enhances the experience of our clients and their treatment
outcomes. Integrating diversity into our assessment, conceptualization,
diagnosis, and treatment, we improve our quality of care and create welcoming
environments for all populations. As we grow in our skills and competencies it
is essential that we remain committed to the principles of multiculturalism,
recognize diversity as a strength, and develop effective training and clinical
services that convey value and respect for everyone.
References
Adams, M. C., &
Kivlighan III, D. M. (2019). When home is gone: An application of
the multicultural orientation framework to enhance clinical practice with refugees
of forced migration. Professional Psychology: Research and Practice, 50(3), 176- 183. https://doi.org/
Aggarwal, N., Nicasio, A.,
DeSilva, R., Boiler, M., & Lewis-Fernandez, R. (2013). Barriers
to Implementing the DSM-5 Cultural Formulation Interview: A qualitative study.
Culture, Medicine, and Psychiatry, 37(3):505-33. doi:
10.1007/s11013-013-9325-z.
Aggarwal, N., and Lewis-Fernandez,
R. (2015) An Introduction to the Cultural Formulation
Interview, Focus, 13:426–431; doi: 10.1176/appi.focus.20150016
American Psychological
Association (2017). Multicultural Guidelines: An Ecological
Approach to Context, Identity, and Intersectionality. Retrieved from:
http://www.apa.org/about/policy/multicultural-guidelines.pdf
American Psychological
Association, APA Task Force on Race and Ethnicity Guidelines
in Psychology. (2019). Race and Ethnicity Guidelines in Psychology:
Promoting Responsiveness and Equity. Retrieved from
http://www.apa.org/about/policy/race-and-ethnicity-in-psychology.pdf
Balva,
D., & Tapia-Fuselier, J. (2020). Working with clients with disabilities: Implications for psychotherapists., 55(1), 19-22.
Bartholomew, T. T., Perez-Rojas,
A. E., Lockard, A. J., Joy, E. E., Robbins, K. A., Kang,
E., & Maldonado-Aguiniga, S. (2021). Therapists’ cultural comfort and
clients’ distress: An initial exploration. Psychotherapy, 58(2),
275–281. https://doi.org/10.1037/pst0000331
Bernal, G., Jimenez-Chafey,
M.I., Domenech Rodriguez, M.M. (2009). Cultural
Adaptation of Treatments: A Resource for Considering Culture in Evidence-Based
Practice. Professional Psychology, Research and Practice. 40(4), 361-368.
https://doi:10.1037/a0016401
Brabeck, M.,
& Brown, L. (1997). Feminist theory and psychological practice. In J. Worell & N. G. Johnson (Eds.), Shaping the future of
feminist psychology: Education, research, and practice (pp. 15–35).
American Psychological Association. https://doi.org/10.1037/10245-001
Bryant-Davis,
T, Diaz-Comas, L (2016). Introduction: Womanist and Mujerista Psychologies. Davis-Bryan, T, Diaz-Comas, L
(Ed.). Womanist and Mujerista Psychologies: Voices of Fire, Acts of Courage.
Washington, D.C. American Psychological Association.
Caldwell, J. C., & Vera,
E. M. (2010). Critical incidents in counseling psychology professionals'
and trainees' social justice orientation development. Training and
Education in Professional Psychology, 4(3), 163–176. https://doi.org/10.1037/a0019093
Cardona, N. D., Cohen, J. M.,
& Feinstein, B. A. (2023). Targeting
self-compassion among sexual and gender minority people experiencing
psychological distress: A comment on Helminen et al. (2022). Clinical
Psychology: Science and Practice, 30(1), 40–42. https://doi.org/10.1037/cps0000116
Chang DF, Dunn JJ, Omidi M. (2021).
A critical‐cultural‐relational approach to rupture
resolution: A case illustration with a cross‐racial dyad. J. Clin.
Psychol. 77:369–383. https://doi.org/10.1002/jclp.23080
Coleiro, A. C., Creaner, M.,
& Timulak, L. (2022): The good, the bad, and the less than
ideal in clinical supervision: a qualitative meta-analysis of supervisee
experiences, Counselling Psychology Quarterly, doi:
10.1080/09515070.2021.2023098
Cousins, C. (2010) 'Treat Me
Don't Beat Me' … . Exploring Supervisory Games
and Their Effect on Poor Performance Management, Practice, 22:5,
281-292, DOI: 10.1080/09503153.2010.514044
Craig, S. L., Alessi, E. J.,
Fisher-Borne, M., Dentato, M. P., Austin, A., Paceley, M.,
Wagaman, A., Arguello, T., Lewis, T., Balestrery, J. E., & Van Der Horn, R.
(2016). Guidelines for affirmative social work education: Enhancing the
climate for LGBQQ students, staff, and faculty in social work education.
Alexandria, VA: Council on Social Work Education.
Comstock, Hammer, T. R.,
Strentzsch, J., Cannon, K., Parsons, J., & II, G. S. (2008).
Relational-Cultural Theory: A Framework for Bridging Relational, Multicultural,
and Social
Justice Competencies. Journal of Counseling and Development, 86(3), 279–287.
https://doi.org/10.1002/j.1556-6678.2008.tb00510.x
Crenshaw, K. (1989). Demarginalizing
the intersection of race and sex: A Black feminist
critique of antidiscrimination doctrine, feminist theory and antiracist
politics. University of Chicago Legal Forum: Vol. 1989 (1), Article 8. chicagounbound.uchicago.edu/uclf/vol1989/iss1/8
Davis, D. E., DeBlaere, C.,
Owen, J., Hook, J. N., Rivera, D. P., Choe, E., Van Tongeren,
D. R., Worthington, E. L., Jr., & Placeres, V. (2018). The multicultural
orientation framework: A narrative review. Psychotherapy, 55(1),
89–100. https://doi.org/10.1037/pst0000160
DeBlaere, C., Zelaya, D. G.,
Dean, J.-A. B., Chadwick, C. N., Davis, D. E., Hook, J.
N., & Owen, J. (2022, December 8). Multiple microaggressions and therapy
outcomes: The indirect effects of cultural humility and working alliance
with Black, Indigenous, Women of Color clients. Professional Psychology:
Research and Practice. Advance online
publication. https://dx.doi.org/10.1037/pro0000497
Delgado-Romero, E. A., De Los
Santos, J., Raman, V. S., Merrifield, J. N., Vazquez,
M. S., Monroig, M. M., Bautista, E. C., & Duran, M. Y. (2018). Caught in
the middle: Spanish-speaking bilingual mental health counselors as language
brokers. Journal of Mental Health Counseling, 40(4),
341–352. https://doi.org/10.17744/mehc.40.4.06
Depauw H, Van Hiel A, De
Clercq B, Bracke P, Van De Putte B. (2022. )Addressing
cultural topics during psychotherapy: Evidence-based do’s and don’ts from an
ethnic minority perspective. Psychotherapy Research. 2022;1-15.
doi:10.1080/10503307.2022.2156307
Draganovic, Selvira. (2012).
Approaches to Feminist Therapy: A Case Study Illustration.
Epiphany. 4. 10.21533/epiphany.v4i1.34.
Dictado, J., &
Torres-Harding, S. R. (2022). Predictors of therapy trainees’ pathologizing
and invalidating microaggressions with sexual and racial minority therapy
clients. Training and Education in Professional Psychology.
https://doi-org.lib.pepperdine.edu/10.1037/tep0000424
Falicov, C. J. (2014a).
Psychotherapy and supervision as cultural encounters: The MECA
framework. In C. Falender, E. Shafranske, & C. Falicov (Eds.), Multiculturalism
and diversity in clinical supervision: A competency-based approach (pp.
29-58). Washington, DC: American Psychological Association.
Falicov C, Nino A, D'Urso S. (2020). Expanding
Possibilities: Flexibility and Solidarity with Under-resourced Immigrant
Families During the COVID-19 Pandemic. Family Process. 59(3):865-882. doi:
10.1111/famp.12578.
Fouad, N. A., &
Chavez-Korell, S. (2014). Considering social class and socioeconomic status in
the context of multiple identities: An integrative clinical supervision
approach. In C. A. Falender, E. P. Shafranske, & C. J. Falicov (Eds.), and diversity in clinical supervision: A
competency-based approach(pp. 145–161). American
Psychological Association. https://doi.org/10.1037/14370-006
Gafford, J., Raines, T. C., Sinha, S., DeBlaere, C.,
Davis, D. E., Hook, J. N., & Owen, J. (2019). Cultural humility as a
spiritually focused intervention in correctional settings: The role of
therapists’ multicultural orientation. Journal of Psychology and
Theology, 47(3), 187–201. https://doi.org/10.1177/0091647119847540
Giddings, M. M., Cleveland, P. H., &
Smith, C. H. (2007) Responding to Inadequate Supervision, The Clinical
Supervisor, 25:1-2, 105-126, DOI:10.1300/J001v25n01_08
Goodman, L. A., Liang, B., Helms, J. E.,
Latta, R. E., Sparks, E., & Weintraub, S. R. (2004). Training counseling
psychologists as social justice agents: Feminist and multicultural principles in
action. The Counseling Psychologist, 32, 793-837.
doi:10.1177/0011000004268802
Guzder, researchgate.net/publication/280742465_supplementary_Module_9_school_aged_children_and_adolescents_DSM_5_APA_publication
Hagler,
M. A. (2020). LGBQ-affirming and -nonaffirming supervision: Perspectives from a queer
trainee. Journal of Psychotherapy
Integration, 30(1),
76–83. https://doi.org/10.1037/int0000165
Hall, G. C. N.,
Berkman, E. T., Zane, N. W., Leong, F. T. L., Hwang, W.-C., Nezu, A. M., Nezu, C. M., Hong, J. J., Chu, J. P., & Huang, E. R.
(2021). Reducing mental health disparities by increasing the personal relevance
of interventions. American Psychologist, 76(1), 91–103.
https://doi.org/10.1037/amp00006160
Hayes J.A., Gelso C.J.,
Goldberg S., Kivlighan D.M. (2018). Countertransference management
and effective psychotherapy: Meta-analytic findings. Psychotherapy, 55(4):496-507.
doi: 10.1037/pst0000189. PMID: 30335461.
Hays, P. A.
(2001). Addressing cultural complexities in practice: A framework for clinicians and counselors. American Psychological Association. https://doi.org/10.1037/10411-000
Hays, P.A.
(2009) Integrating Evidence-Based Practice, Cognitive-Behavior Therapy, and Multicultural Therapy: Ten Steps for Culturally
Competent Practice. Professional Psychology, Research and Practice, 40 (4),
354-360.https:// doi:10.1037/a0016250
Hays, P. A.
(2012). Connecting Across Cultures: The Helper's Toolkit. India: SAGE Publications.
Hays, P. S.
(2022). Addressing cultural complexities in counseling and clinical practice: An intersectional approach (4th ed.)
American Psychological Association.
Helminen, E.
C., Ducar, D. M., Scheer, J. R., Parke, K. L., Morton, M. L., & Felver, J. C. (2023). Self-compassion, minority stress, and mental health in
sexual and gender minority populations: A meta-analysis and systematic
review. Clinical Psychology: Science
and Practice, 30(1), 26–39. https://doi.org/10.1037/cps0000104
Hernandez, P., & McDowell, T.
(2010). Intersectionality, power, and relational safety in context: Key
concepts in clinical supervision. Training and Education in Professional
Psychology, 4, 29–35. http://dx.doi .org/10.1037/a0017064
Hernandez-Wolfe, P., &
McDowell, T. (2013) Social Privilege and Accountability: Lessons from Family Therapy Educators, Journal of Feminist Family Therapy, 25:1, 1-16, doi: 10.1080/08952833.2013.755079
Hook, J., Davis, D., Owen, J.,
Worthington, E., & Utsey, S. (2013). Cultural humility: Measuring openness
to culturally diverse clients. Journal of Counseling Psychology, 60(3),
353-366. doi:10.1037/a0032595
Hook, J. N., Davis, D., Owen, J., &
DeBlaere, C. (2017). Cultural humility: Engaging diverse identities in
therapy. American Psychological Association. https://doi.org/10.1037/0000037-000
Huey, S. J., Jr.,
& Polo, A. J. (2008). Evidence-based psychosocial treatments for ethnic minority youth. Journal of Clinical Child and Adolescent
Psychology, 37(1), 262-301. doi: 10.1080/15374410701820174.
Huey, S. J.,
Henggeler, S. W., Rowland, M. D., Halliday-Boykins, C. A.,
Cunningham, P. B., Pickrel, S. G., & Edwards, J. (2012).
Cultural adaptation of evidence-based interventions: An example from
psychotherapy with African American/Black youth. Journal of Black Psychology,
38(3), 286-310. doi: 10.1177/0095798411407347.
Huey, S.J.,
Tilley, J.L., Jones, E.O., & Smith, C.A. (2014). The Contribution of Cultural Competence to Evidence-Based Care for Ethnically Diverse
Populations. Annual Review of Clinical Psychology. 10(1), 305-338.
https://doi:10.1146/annurev-clinpsy-032813-153729
Israeli, A. &
Santor, D. A. (2000). Reviewing effective components of feminist therapy. Counselling Psychology Quarterly, 13(3), 233–247. https://doi.org/10.1080/095150700300091820
Jarvis, G.,
Kirmayer, L., Gomez-Carrillo, A., Aggarwal, N. & Lewis-Fernandez, R.(2020) Update on the Cultural Formulation Interview. Focus. American Psychiatry Publication). 18(1):40-46. doi: 10.1176/appi.focus.20190037.
Kahneman, D., & Tversky,
A. (1973). On the psychology of prediction. Psychological
Review, 80, 237–251.
Kim, U., & Park, Y. (2007).
Development of indigenous psychologies: Understanding
people in a global context. In M. J. Stevens & U. P. Gielen (Eds.), Toward
a global psychology: Theory, research, intervention, and pedagogy (pp.
147-172). Mahway, NJ: Lawrence Erlbaum.
Kivlighan DM, Swancy AG,
Smith E, Brennaman C. (2021). Examining racial microaggressions
in group therapy and the buffering role of members' perceptions of their
group's multicultural orientation. Journal of Counseling Psychology, 68(5),
621-628. doi: 10.1037/cou0000531
Knapp,
S., Handelsman, M. M., Gottlieb, M. C., & VandeCreek, L. D. (2013). The dark side of professional ethics. Professional Psychology: Research and Practice, 44(6), 371–377. https://doi.org/10.1037/a0035110
Magesh S, John D, Li WT, et
al. Disparities in COVID-19 Outcomes by Race, Ethnicity,
and Socioeconomic Status: A Systematic Review and Meta-analysis. JAMA Netw
Open. 2021;4(11):e2134147. doi:10.1001/jamanetworkopen.2021.34147
McCall, L. (2005). The
complexity of intersectionality. Signs, 30, 1771–1800. doi:10.1086/426800
Meyer, M. L., & Young, E.
(2021). Best practice recommendations for psychologists
working with marginalized populations impacted by COVID-19. Professional
Psychology: Research and Practice, 52(4), 309–317.
https://doi.org/10.1037/pro0000409
Miville, M. L. (Ed.) (2013). Multicultural
gender roles: Applications for mentalhealth
and education. New Jersey, Wiley.
Miville, M. L., Romero, L.,
& Corpus, M. J. (2009). Incorporating affirming, feminist,
and relational perspectives: The case of Juan. In M. E. Gallardo &
B.
W. McNeill (Eds.), Intersections of multiple identities: A casebook of
evidence-based practices with diverse populations (pp. 175–201).
Routledge/Taylor & Francis Group. National Association of
Social Workers. (2019). NASW Social Justice priorities. socialworkers.org/Portals/0/PDF/Advocacy/Public/Social-Justice/Social-Justice-Priorities-2018-2019.pdf
Neff, K. (n.d.). Self-compassion. self-compassion.org
Odegard, M. A., & Vereen,
L. G. (2010). A grounded theory of counselor educators
integrating social justice into their
pedagogy. Counselor Education and Supervision, 50, 130–149. doi:10.1002/j.1556-6978.2010.tb00114.x
Oliphant, V.,
Broyles, D., Clement, D. & Wingate, L. (2022). Mental Health Strategies
Informed by Black Feminist Thought. Open
Cultural Studies, 6(1),
137-146. https://doi.org/10.1515/culture-2022-0151
Owen, J.,
Tao, K. W., Drinane, J. M., Hook, J., Davis, D. E., & Kune, N. F. (2016). Client perceptions of therapists’ multicultural orientation:
Cultural (missed) opportunities and cultural humility. Professional
Psychology: Research and Practice, 47(1), 30–37.
https://doi-org.lib.pepperdine.edu/10.1037/pro0000046
Owen, J., Tao,
K. W., Imel, Z. E., Wampold, B. E., & Rodolfa, E. (2014). Addressing racial and ethnic microaggressions in therapy. Professional
Psychology: Research and Practice, 45(4), 283-290.
doi:10.1037/a0037420
Owen, J. J., Tao, K., Leach,
M. M., & Rodolfa, E. (2011). Clients'
perceptions of their psychotherapists' multicultural orientation. Psychotherapy, 48(3),
274–82. https://doi.org/10.1037/a0022065
Perez-Rojas, A. E., Palma,
B., Bhatia, A., Jackson, J., Norwood, E., Hayes, J. A., & Gelso, C. J.
(2017). The
development and initial validation of the Countertransference Management Scale.
Psychotherapy, 54(3), 307–319. https://doi.org/10.1037/pst0000126
Pieterse,
A. L. (2018). Attending to racial trauma in clinical supervision: Enhancing client and supervisee outcomes. The Clinical Supervisor, 37(1), 204 220. https://doi.org/10.1080/07325223.2018.1443304
Pieterse, A. L., Austin, C.
L., Nicolas, A. I., Martin, C., Agiliga, A., & Kirkinis, K. (2023, April
20). Essential
Elements for Working With Racial Trauma: A Guide for Health Service
Psychologists. Professional Psychology: Research and Practice. Advance
online publication. https://dx.doi.org/10.1037/pro0000512
Rolland, L., Costa, B., &
Dewaele, J. (2021). Negotiating
the language(s) for psychotherapy talk: A mixed methods study from the
perspective of multilingual clients. Counselling & Psychotherapy
Research, 21(1), 107–117. https://doi:10.1002/capr.12369
Rolland, L., Dewaele, J.-M., &
Costa, B. (2017). Multilingualism
and psychotherapy: Exploring multilingual clients’ experiences of language
practices in psychotherapy. International Journal of Multilingualism, 14(1),
69–85. https://doi.org/10.1080/14790718.2017.1259009
Shafranske,
E. P. (2016). Finding a place for spirituality in psychology training: Use of competency-based clinical supervision. Spirituality in Clinical Practice, 3(1), 18–21. https://doi.org/10.1037/scp0000098
Singh,
A. A., & dickey, l. m. (2017). Affirmative counseling with transgender and gender nonconforming clients. In K. A. DeBord,
A. R. Fischer, K. J. Bieschke, & R. M. Perez (Eds.), Handbook of sexual orientation and gender diversity in counseling and psychotherapy (pp. 157–182). American Psychological
Association. https://doi.org/10.1037/15959-007
Stewart, Abigail &
Dottolo, Andrea. (2006). Feminist Psychology. Signs: Journalof
Women in Culture and Society, 31.
493-509. doi: 10.1086/491683.
Soto A, Smith TB, Griner D,
Domenech Rodriguez M, Bernal G. (2018). Cultural
adaptations and therapist multicultural competence: Two meta-analytic reviews. Journal
of Clinical Psychology (11):1907-1923. doi: 10.1002/jclp.22679.
Sue, D. W. (2010). Microaggressions
in everyday life: Race, gender, and sexual orientation, Wiley. Sue, D. W., Alsaidi, S.,
Awad, M. N., Glaeser, E., Calle, C. Z., & Mendez, N. (2019).
Disarming racial microaggressions: Microintervention strategies for targets,
White allies, and bystanders. American Psychologist, 74(1),
128–142. https://doi.org/10.1037/amp0000296
Sue, D. W., Arredondo, P.,
& McDavis, R. J. (1992). Multicultural counseling competencies
and standards: A call to the profession. Journal of Multicultural Counseling
and Development, 20(2), 64–88. https://doi.org/10.1002/j.2161-1912.1992.tb00563.x
Sue, D. W., Capodilupo, C.
M., Torino, G. C., Bucceri, J. M., Holder, A. M. B., Nadal,
K. L., & Esquilin, M. (2007). Racial microaggressions in everyday life:
Implications for clinical practice. American Psychologist, 62(4), 271-286. doi:10.1037/0003-066X.62.4.271
Tervalon, M., &
Murray-Garcia, J. (1998). Cultural humility versus cultural competence: A critical
distinction in defining physician training outcomes in multicultural education. Journal of Health Care for the Poor and Underserved, 9, 117-125. Retrieved
from http://www.press.jhu.edu/journals/journal_of_health_care_for_the_poor_and_underserved/
Tversky, A., & Kahneman,
D. (1973). Availability: A heuristic for judging frequency
and probability. Cognitive Psychology, 5, 207–232.
doi:10.1016/0010-0285(73)90033-9
Valencia-Garcia, D., &
Montoya, H. (2018). Lost in translation: Training issues forbilingual
students in health service psychology. Training and Education in
Professional Psychology, 12(3), 142–148.
https://doi-org.lib.pepperdine.edu/10.1037/tep0000199
Vieten,
C., & Lukoff, D. (2022). Spiritual and religious competencies in psychology. American Psychologist, 77(1), 26–38. https://doi.org/10.1037/amp0000821
Watson, P., Norman, S. B., Maguen,
S., & Hamblen, J. National Center for PTSD,
U.S. Department of Veteran Affairs (n.d.) Moral injury in healthcare workers https://www.ptsd.va.gov/professional/treat/cooccurring/moral_injury_hcw.asp
Wilcox, M. M., Franks, D. N.,
Taylor, T. O., Monceaux, C. P., & Harris, K. (2020).
Who’s multiculturally competent? Everybody and nobody: A multimethod
examination. The Counseling Psychologist, 48(4), 466–497.doi.org/10.1177/0011000020904709



 ContinuingEdCourses.Net is approved by the American Psychological Association (APA) to sponsor continuing education for psychologists. ContinuingEdCourses.Net maintains responsibility for this program and its content.
ContinuingEdCourses.Net is approved by the American Psychological Association (APA) to sponsor continuing education for psychologists. ContinuingEdCourses.Net maintains responsibility for this program and its content. ContinuingEdCourses.Net, provider #1107, is approved as an ACE provider to offer social work continuing education by the Association of Social Work Boards (ASWB) Approved Continuing Education (ACE) program. Regulatory boards are the final authority on courses accepted for continuing education credit. ACE provider approval period: 3/9/2005-3/9/2027.
ContinuingEdCourses.Net, provider #1107, is approved as an ACE provider to offer social work continuing education by the Association of Social Work Boards (ASWB) Approved Continuing Education (ACE) program. Regulatory boards are the final authority on courses accepted for continuing education credit. ACE provider approval period: 3/9/2005-3/9/2027. ContinuingEdCourses.Net has been approved by the National Board for Certified Counselors (NBCC) as an Approved Continuing Education Provider (ACEP), ACEP #6323. Programs that do not qualify for NBCC credit are clearly identified. ContinuingEdCourses.Net is solely responsible for all aspects of the programs.
ContinuingEdCourses.Net has been approved by the National Board for Certified Counselors (NBCC) as an Approved Continuing Education Provider (ACEP), ACEP #6323. Programs that do not qualify for NBCC credit are clearly identified. ContinuingEdCourses.Net is solely responsible for all aspects of the programs. ContinuingEdCourses.Net is recognized by the New York State Education Department's State Board for Psychology (NYSED-PSY) as an approved provider of continuing education for licensed psychologists #PSY-0048.
ContinuingEdCourses.Net is recognized by the New York State Education Department's State Board for Psychology (NYSED-PSY) as an approved provider of continuing education for licensed psychologists #PSY-0048.