Learning Objectives
This is an intermediate-to-advanced level course. It is recommended that those wishing to take this course first take the course ADHD: Nature, Course, Outcomes, and Comorbidity. After completing this course, mental health professionals will be able to:
- List four goals in the assessment of children referred for possible Attention-Deficit/Hyperactivity Disorder (ADHD).
- Outline a clinical interview with parents, teachers, and children for assessment of ADHD.
- Utilize appropriate behavioral rating scales for evaluating ADHD in clients.
- Describe an effective feedback session to parents.
- List three components of parent training in contingency management, using the author’s 10-step program.
- Discuss three FDA-approved medications for use with ADHD.
- Offer behavior management options available for use in school.
The materials in this course are based on the most accurate information available to the author at the time of writing. The scientific literature on ADHD grows daily and new information may emerge that supersedes these course materials. This course will equip clinicians to have a basic understanding of the diagnosis, assessment, and management of ADHD. This course is adapted from the relevant chapters contained in Barkley, R. A. (2015), Attention Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment (4th ed.). New York: Guilford Press and his more recent book, Barkley, R. A. (2022). Treating Children and Adolescents with ADHD: What Every Clinician Needs to Know. New York: Guilford Press.
Outline
- Introduction
- Primary Symptoms of ADHD
- ADHD as a Disorder of Executive Functioning and Self-Regulation
- Self-Regulation and the Development of Executive Functions
- How Do We Know ADHD Is a Disorder of Executive Function?
- The Neuroanatomy of ADHD
- Broad Clinical Implications of the EF-SR Theory of ADHD
- The DSM Criteria Within the EF-SR Theory
- Inattentive to What?
- Emotional Dysregulation as a Core Component
- Does Testing Reveal the EF Deficits in ADHD?
- The EF-SR Theory Leads to Treatments That Help in Real Life
- Treatments That Help Patients Do What They Know When They Need to Use That Knowledge
- Treatments That Rearrange the Environment to Compensate for Executive Function Deficits
- Medications for EF-SR Deficits
- Diagnostic Criteria
- Principles for Diagnosing ADHD Using EF-SR Theory
- Principle 1: Start the Diagnostic Process with the DSM-5-TR Criteria – But Don’t Stop There
- Principle 2: Understand the Importance of Impairments vs. Symptoms
- Principle 3: Always Consider the Neurogenetic Origins of ADHD
- Principle 4: Keep in Mind That the Goal Is Not Just Diagnosis of ADHD but Differential Diagnosis from Other Disorders
- Principle 5: Be Prepared to Confront Myths and Resistance from Parents and Clients (Particularly Teens)
- Principle 6: Be Prepared to Follow Up Diagnosis with Appropriate Treatment
- Assessment
- Assessment Issues
- Information Obtained at the Time of Referral
- Information Obtained in Advance of the Interview
- Parent Interview
- Child Interview
- Teacher Interview
- Rating Scales
- The Role of Psychological Testing
- Legal and Ethical Issues
- The Pediatric Medical Examination
- The Medical Interview
- Physical Examination
- Laboratory Tests
- The Feedback Session
- Conclusion on Assessment
- Treatment Approaches
- Re-examining Treatment Assumptions
- Treatments for ADHD: Introduction
- Parent Counseling and Behavior Management Training
- Parent Education and Counseling
- Be Alert to a Parental Grief Reaction
- Introduce the Concept of a Delayed Executive Age
- Emphasize That All Effective Treatments Must Be at the Point of Performance
- Introduce the 12 Best Principles for Parents
- Make Health and Lifestyle Recommendations
- Behavioral Parent Training (BPT)
- Are BPT Programs Necessary for Children Taking ADHD Medication?
- How BPT Programs Are Structured
- Program Effectiveness and Predictors of BPT Success
- Side Effects of BPT
- Cognitive-Behavioral Therapies (CBT) for Teens with ADHD
- Mindfulness Meditation Training of Teens with ADHD
- Friendship Coaching: Training Parents to Improve Child Social Skills
- Psychopharmacology
- Understanding the Full Value of Medications Through the EF-SR Theory
- Stimulant Medication
- Effectiveness, Safety, and Practicality of Stimulant Medication
- Special Considerations with Adolescents
- The Non-Stimulants: Atomoxetine (Strattera®) and Viloxazine (Qelbree®)
- Antihypertensive Medications
- School Management of ADHD
- Ineffective or Unproven Therapies
- Conclusion on Treatment
- Appendix
- References
Introduction
Over the past century, numerous diagnostic labels have been given to clinically referred children having significant deficiencies in behavioral inhibition, sustained attention, resistance to distraction, and the regulation of activity level. Most recently, Attention Deficit-Hyperactivity Disorder (ADHD) (DSM-5-TR, American Psychiatric Association, 2022) is the term used to capture this developmental disorder. Previously employed terms have been brain-injured child syndrome, hyperkinesis, hyperactive child syndrome, minimal brain dysfunction, and Attention Deficit Disorder (with or without Hyperactivity). Such relabeling every decade or so reflects a shifting emphasis in the primacy accorded certain symptom clusters within the disorder based, in part, on the substantial research conducted each year on ADHD and how investigators and theorists interpret those findings. A reasonably thorough history of ADHD can be found in the chapter on that topic in the author’s 4th edition of his Attention Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment.
This course initially presents a brief discussion of ADHD as a disorder of executive functioning and self-regulation (EF-SR Theory). A more detailed presentation on EF and SR is provided in my course on that topic on this website (Executive Functioning: Understanding and Managing Deficits). Here I want to focus more on the implications of this theory for the diagnosis and management of ADHD.
Next, this course provides a summary of the major components involved in the assessment of ADHD followed by an overview of the treatments that have some efficacy for the management of ADHD as shown through scientific research. The literature on treatment is voluminous, however, and so space here permits only a brief discussion and critique of each of the major treatments. More detailed discussions of these treatments can be found in the textbooks by Barkley (2015, 2022), Becker (2020) and Banaschewski, et al. (2018).
Primary Symptoms of ADHD
Here I discuss the traditional symptoms associated with ADHD as might be found in the DSM-IV diagnostic criteria and adjustments that have been made in the DSM-5-TR. Later, I will make the case that ADHD is really a disorder of EF-SR and show what that means for diagnosis, assessment, and management.
Children having ADHD, by definition, display difficulties with attention and/or impulse control relative to the non-ADHD population of children of the same age and sex. Attention is a multi-dimensional construct which can refer to problems with alertness, arousal, selective or focused attention, sustained attention, distractibility, or span of apprehension, among others. Research to date suggests that among these elements, children with ADHD most likely have their greatest difficulties with sustaining attention to tasks (persistence of responding), resisting distractions, and re-engagement in initial tasks once disrupted.
These difficulties are sometimes apparent in free-play settings but are much more evident in situations requiring sustained attention to dull, boring, and/or repetitive tasks. However, even when presented with apparently intrinsically interesting stimuli, such as a television program, or attractive distracting stimuli, such as toys, children who have ADHD may exhibit significantly impaired attention to and comprehension of events relative to children who do not have ADHD. More recently, research is suggesting that the attention problems evident in ADHD are part of a larger domain of cognitive activities known as executive functioning, and especially working memory (i.e., holding information in mind that is being used to guide performance). Specifically, evidence from the development of rating scales indicates that the DSM items used to define the attention deficits in ADHD load on a larger dimension containing items reflecting executive functioning and specifically, working memory.
Often coupled with this difficulty in sustained attention is a deficiency in inhibiting behavior, or impulsiveness. Like attention, impulsiveness is also multidimensional in nature. Rather than cognitive reflectiveness, the deficit in ADHD is mainly in the capacity to inhibit or delay prepotent or automatic responses, particularly in settings in which those responses compete with rules. A prepotent response is that which would gain the immediate reinforcement (reward or escape) available in a given context, or which has a strong history of such reinforcement in the past. Those with ADHD have difficulties with sustained inhibition of such dominant responses over time, as well as with poor delay of gratification, a steeper discounting of the value of delayed over immediate rewards, and impaired adherence to commands to inhibit behavior in social contexts. This inhibitory deficit may also include a difficulty with interrupting an already ongoing response pattern, particularly when given feedback about performance and errors. In the latter case, perseverative responding may be evident despite negative feedback concerning such responding. That problem may be reflecting an insensitivity to errors. Overall, individuals with ADHD have poorer inhibitory control and slower inhibitory processing than are normal.
Numerous studies have shown that children with ADHD tend to be more active, restless, and fidgety (i.e., hyperactive) than children without ADHD. As with the other symptoms, there are significant situational fluctuations in this symptom. It has not always been shown convincingly that hyperactivity distinguishes ADHD children from other clinic-referred groups of children. It may be the pervasiveness of the hyperactivity across settings that separates ADHD from other diagnostic categories.
ADHD symptoms of hyperactivity have been shown to decline significantly across the elementary school years, while problems with attention persist at relatively stable levels during this same period of development in children with ADHD. One explanation that may account for such a state of affairs is that the hyperactivity reflects an early developmental manifestation of a more central deficit in behavioral inhibition. Studies that factor in analyzed behavior ratings certainly show that hyperactivity and poor impulse control form a single dimension of behavior, as shown in the DSM-5-TR. This deficit in inhibition, of which early hyperactivity is a part, may become increasingly reflected in poor self-regulation over various developmental stages, even though the difficulties with excessive activity level may wane with maturation.
Difficulties with adherence to rules and instructions are also evident in children with ADHD. Care is taken here to exclude poor rule-governed behavior that may stem from sensory handicaps (i.e., deafness), impaired language development, or defiance or oppositional behavior. Nevertheless, children with ADHD typically show significant problems with compliance with parental and teacher commands, following experimental instructions in the absence of the experimenter, and with adhering to directives to defer gratification or resist temptations. Like the other symptoms, this problem with rule-governed behavior is a multi-dimensional construct. It remains to be shown which aspects of this construct are specifically impaired in ADHD.
ADHD as a Disorder of Executive Functioning and Self-Regulation
The diagnostic criteria for ADHD are based on the disorder’s most obvious behavioral symptoms. Viewed through that thin lens, as shown above, ADHD is surely a disorder comprised of inattention, impulsivity, and hyperactivity. But calling ADHD an attention disorder is like referring to autism spectrum disorder as “hand flapping, stereotyped movement, or odd behavior disorder.” If we look at ADHD through a much thicker lens, we find it is far more than a set of obvious behaviors.
Underneath those surface symptoms, ADHD is actually a disorder of self-regulation, making it more accurately self-regulation deficit disorder (SRDD). I am not the first to make this claim. The highly esteemed Canadian psychologist Virginia Douglas asserted 40 years ago (1980, 1988) that ADHD was a disorder of self-control, although she did not clearly define operationally what that term meant and what mental functions people employ for self-control that were deficient in people with ADHD. Now we recognize that self-regulation relies on executive function and its underlying brain networks. Therefore, ADHD could also be called EFDD.
The reason I prefer the term SRDD is that it is the obvious and repeated failure to demonstrate self-regulation that is so apparent to those with ADHD, their families, and clinicians who are trying to evaluate and manage it. The deficits in executive function create that phenotype, but they are not so visible in the patient with ADHD, being largely private or mental activities, especially by adulthood. For instance, patients with ADHD may repeatedly forget to take their car keys when leaving and thus lock themselves out of their own home, may forget why they went into a room to get something, or forget that they agreed to meet someone for a meeting over lunch. These are obvious problems, yet the underlying deficits in verbal and nonverbal working memory and governance of action plans by the sense of time that gives rise to them, remain unseen to others. The label SRDD is a useful reminder for clinicians that what you are seeing in those with ADHD is a heterogeneous set of wide-ranging, impairing problems with the executive functions and the self-regulation they provide.
Even though most or all investigators today recognize that executive functions involve the mental abilities necessary for goal-directed action, there is still plenty of disagreement on the exact definition of executive function (20-30 definitions and counting), on what makes a mental function executive in nature, and on just how many functions fall under this umbrella (3–33 at last count!). The widespread idea that executive functions involve those cognitive abilities needed for goal-directed action, and thus enable an intentional stance toward the future, remains too vague for an operational definition. I address that critical problem shortly. What is important here to understand, if you are to accurately diagnose and effectively treat those with ADHD, is what abilities qualify as executive functions and how they operate in disrupting daily adaptive functioning.
Self-Regulation and the Development of Executive Functions
There’s a missing link between the neuroanatomical malformations and the cognitive and behavioral symptoms associated with ADHD. That link is provided by viewing ADHD symptoms as executive function deficits. But to understand what executive function is, we first have to come up with an operational definition of just what constitutes an executive function, and then show how the seven major executive functions meet that definition. That solution comes from our understanding that executive function involves self-regulation.
B. F. Skinner and others have defined self-regulation as the self-direction of actions that are intended to modify subsequent behavior in order to alter the likelihood of a delayed (future) consequence.
In my theory, an executive function is defined as a specific type or form of self-directed action. Here, then, is our operational definition of self-regulation. Cognitive or behavioral actions directed at oneself in order to change a subsequent behavior in an attempt to alter the future are, by definition, executive in nature. Cognitive and behavioral actions that are not self-directed for such purposes are not executive. We can usefully define the seven major executive functions as seven major types of actions-to-the-self that serve to modify subsequent behavior and thereby strive to change future events for that individual.
I have further proposed that each EF is a human behavior or cognitive action initially directed toward the external world early in human development. It will eventually become self-directed and then progressively internalized (privatized) to form a largely mental self-directed activity – something done in the conscious mind.
The specific case of private self-speech illustrates this more general process. In it, children start by directing speech out loud to the external environment generally and to others specifically. They then enter a phase where they direct their speech at themselves, even when no one is in that context with them – yet it is still external speech; it is observable. Then, gradually, children internalize such self-directed speech. Privatize is more accurate, which is to say that this process involves the brain inhibiting peripheral neural activity and muscle movements while still activating the speech centers of the brain. Eventually, this gradual process of privatization reaches a point where the self-speech can’t be observed publicly at all. Children now have a mind’s voice that only they can hear. I have argued that this illustrates the more general process by which all seven executive functions develop:
At first, children’s actions are directed at the world around them. Infants have not yet developed EFs, so for instance when they learn to speak, they talk out loud to and about their surroundings, especially to other people in their environment.
Next, they direct their actions back at themselves, most of which may be observable. For instance, children talk to themselves even when no one else is present.
Subsequently, they internalize these self-directed actions through a process of inhibition of the associated peripheral movements while activating relevant brain regions and networks. For instance, self-speech gradually becomes quieter, involving barely audible whispers, then just facial movement, then subvocal actions, and finally suppression of the oral musculature. This progression is what we see in second- and third-graders who talk to themselves while doing math worksheets: Their mouths are moving, as if whispering to themselves, but they’re making no audible sound, perhaps also while touching their fingers to aid their counting.
Finally, children can engage in these actions to themselves without visible peripheral motor and vocal movements. In the case of self-speech, the movements of the face, larynx, and diaphragm are being largely inhibited while the central speech centers of the brain are activated. Both speech and gesture in the example above of the second-grader doing math will eventually be peripherally inhibited, while remaining centrally activated in the brain, and will thus become a cognitive form of executive function – a mind-tool for self-regulation. The self-directed actions are now occurring within the brain, but the associated nerve signals are not emitted into the spinal cord. Now these actions are internal and private. In our example, children can now talk to themselves in their mind without anyone seeing or hearing the speech. Children of this age often announce to their parents the discovery that there is a voice in their head. An entirely mental or cognitive form of behavior and self-regulation has now emerged. Thinking, in this case self-speech, then serves to govern motor actions, such as behavior toward goals.
Even later in development, people may create external cues to further assist the self-governing activities they are doing in their mind. For instance, as written language is acquired, people learn to write notes to themselves (“to do” lists) as yet another method of self-regulation using self-speech. Or they may place nonverbal cues, such as objects or pictures, in useful locations in their visual or sensory fields to further aid the stimulus control of their private forms of self-regulation.
This newly emerging private self can now mentally test out various ideas without engaging in their external or public performances and thereby avoid experiencing the real-world consequences that would have occurred with those publicly executed counterparts. Private or mental simulation of possible action plans is now possible, allowing for the natural selection of the most optimal among them while the mistaken ones die in our place, as Karl Popper once noted. In the case of self-speech, this means older children or teens can rehearse mentally what they want to say later publicly to improve their eventual public verbal performances. This can also be done for various motor activities using private visual-motor rehearsals.
A plurality of researchers identified at least seven executive functions. These are self-awareness, inhibition, nonverbal and verbal working memory, emotional self-regulation, self-motivation, and planning/problem-solving (or manipulation of mental representations). My theory argues that all of these are forms of self-directed actions and all emerge via the same general developmental process noted earlier. Therefore, each executive function can be redefined by the action to the self that is involved in it:
- Self-directed attention (self-awareness);
- Self-restraint (volitional inhibition);
- Self-directed sensory-motor actions (visual imagery or nonverbal working memory);
- Self-directed speech (verbal working memory);
- The self-direction of emotions (emotional self-regulation), and thereby;
- Self-motivation, and eventually;
- Self-directed play (usually mental manipulations for planning and problem solving).
Over development, the maturation of these executive functions allows children greater degrees of freedom from being controlled purely by external events, and others in the moment to become fully independent and self-controlling entities. That is because what is controlling their behavior is changing from early childhood to adulthood as represented in these four transitions from external to self (internal) control:
- From control by external events to self-control via mental representations (self-speech, visual imagery, etc.);
- From control by others to control by the self (using mental self-directed executive functions);
- From the present or now to the mentally conjectured future; and
- From small, immediate rewards (gratification) to delayed, larger rewards.
In ADHD, the delayed and disrupted development of all seven executive functions greatly interferes with these extremely important transitions in what sources are regulating one’s behavior – the immediate and external world or the self and mental foresight.
Clinically, I’ve found it useful to explain the executive functions and their hierarchical development by referring to them – especially for children – simply as the mind’s mirror, brakes, eye, voice, heart, fuel tank, and playground, respectively. All this is where the child or teen with ADHD is delayed in development. That leads to an equally useful principle to explain to parents and others. Children with ADHD have an executive age (EA) that is significantly below their chronological age (CA), and thus one cannot expect or demand them to self-regulate the way that their typical peers are able to do. EFDD = CA - EA.
The corollary of that idea is to reduce our expectations to match the child’s executive age and make necessary accommodations in the environment that support the child’s behavior and performance, thus making the child less impaired, if not less ADHD. The extent of this lag in executive age will vary across children with ADHD, perhaps ranging from 20%-45% below their chronological age. But that is not as important as realizing that the lag exists, is substantial, isn’t going away anytime soon, and requires accommodations.
Of course, there are much greater clinical implications of the EF-SR theory to consider, which I do throughout this book. Yet even this one idea about delayed executive age is incredibly valuable to parents and teachers in understanding children and teens with ADHD and making accommodations for them.
The self-directed actions that comprise the executive functions are essential for the contemplation of a hypothetical future – essentially a goal. That hypothetical future is then juxtaposed against the present, which can lead to both the formation of an intention or goal and the plan to attain it. Thus, as many other experts have said, executive function is future-directed. But lacking in such statements is the key point – the executive functions are self-directed actions for behavioral self-modification so as to improve one’s future.
How Do We Know ADHD Is a Disorder of Executive Function?
As the great neuroscientist Joaquin Fuster so eloquently argued in his 1997 book on the prefrontal lobes, the quintessential function of that brain region is the formation of goals and the cross-temporal construction, organization, and maintenance of behavior needed to attain those desired goals, or what constitutes a hypothetical future. In other words, the role of executive function is to allow us to behave in ways that serve the future we want. So, if what we see in ADHD at a much deeper level than inattention, hyperactivity, and impulsivity is a deficit in self-regulation, it must be rooted in problems with these executive functions. And, in fact, neuroanatomy tells us that is so.
The Neuroanatomy of ADHD
The areas of the brain most reliably associated with ADHD (Faraone et al., 2024) are the prefrontal cortex, the anterior cingulate, the basal ganglia (especially the striatum), the cerebellum (especially the central vermis), and the amygdala (not always reliably implicated). Research demonstrates that these regions are functionally interconnected to form one of the seven major brain networks – the executive system. In my view, that system underlies the human capacity for self-regulation and, as Fuster concluded, for the cross-temporal organization of behavior toward goals (future-oriented action). There are at least four or five subnetworks in the executive network, each of them associated with different parts of the brain, that can help us understand how executive functions help us self-regulate – or, in the case of ADHD – make it difficult to do so:
- The Inhibitory Executive Network: Think of this subnetwork as allowing us to resist responding to goal-irrelevant events, or distraction. It’s responsible for the voluntary inhibition of ongoing behavior and emotions, as well as the suppression of competing responses to goal-irrelevant events, both internal and external.
- The “What” or Cold Executive Network: Essentially, this network allows what we think about (mainly imagery and self-talk) to guide what we do. It also permits the higher-level function of the manipulation of goal-related mental representations (analysis and synthesis, or mental play) so as to support planning and problem solving.
- The “When” (Timing) Executive Network: When we choose to act can be as or more critical to the success of a plan than what we had planned to do, and it’s this subnetwork that gives us a subjective sense of time and the temporal sequencing of thought and action as well as the timeliness in executing such actions.
- The Hot (Emotional) or “Why” Executive Network: This is probably the subnetwork that makes the final decisions about goal choices and the selection of planned actions to attain them. But it also permits the top-down regulation of emotion in the service of those goals and our longer-term welfare, probably through the use of self-imagery and self-talk, or the working memory network above.
You may be wondering where hyperactivity fits into the executive function neuroanatomy picture of ADHD. In part, it certainly arises from defective functioning of the inhibitory network. But in addition to the subnetworks listed above, is the motor activity regulation network. Disturbances in this network are thought to also give rise to the hyperactive symptoms of the disorder.
If what you are seeing in a patient includes problems with goal-directed attention and volitional inhibition, resistance to distraction, working memory (forgetfulness in daily activities), sense of time and timing, time management, planning and problem-solving, self-organization, emotional self-regulation, self-motivation, and self-awareness – essentially the major executive functions – and not just the traditional DSM-5-TR ADHD symptoms, then a patient may well qualify for a diagnosis of ADHD and certainly has executive function deficits underlying them. When you see this in patient after patient with ADHD, it is easy to come to see that, logically, ADHD must be EFDD at its root.
What does this mean clinically? It means that:
- ADHD comprises a far broader array of cognitive and behavioral deficiencies than is reflected in the current clinical view as set forth in the DSM-5-TR. To call this merely an attention disorder is both to trivialize the condition and be clinically unproductive.
- You need to listen for the deficits in the various executive functions as you interview patients about these executive function domains, going beyond a mere exploration of just the DSM-5-TR ADHD symptoms.
- It is this broader array of executive function deficits that accounts for the range of impairments that people with ADHD experience across most domains of major life activities.
- These executive function deficits are the things that will require accommodations and other treatments well beyond what might be suggested from the traditional ADHD symptom dimensions.
- Because the executive function subnetworks functionally interconnect – that is, they interact in varying ways from patient to patient – ADHD will be heterogeneous across cases. Don’t expect symptomatic presentations to be identical or even highly similar. When you know that some networks may be more (or less) adversely affected by the various etiologies of ADHD than others, you know that close scrutiny will be required by the astute diagnostician to appreciate the diversity of clinical symptoms patients may demonstrate.
Viewing ADHD through the lens of executive functioning should, at the very least, underscore the urgency of diagnosing ADHD and treating it promptly. A child who is bouncing off the walls all day is not just at risk of frequent discipline in preschool settings or poor academic performance later in formal schooling, but of frequent and serious accidental injury and even early mortality. One who impulsively can’t wait for things, or take turns, or who can’t pay attention long enough to clean his room, is not just going to have trouble keeping friends or finding his backpack amid the mess; he is going to fail to attend to heightened risks during his routine activities. In everything from cellphone-distracted cycling (and, later, driving) to daring physical feats and excessive Internet gaming, the child will engage in impulsive risk-taking both in and away from home. As a result, children with ADHD suffer frequent closed head trauma, substance experimentation and risk for addiction, and pursue more appealing activities to the exclusion of fulfilling home and school responsibilities, among other harms. This child is at risk of missing out on succeeding in the full panoply of human experiences and achievements throughout the life span if undiagnosed and untreated.
How will this perspective affect the way you diagnose and treat a child or teenager’s ADHD? The rest of this course provides clinical guidance for diagnosis, assessment, and management, but all of this benefits from seeing ADHD through the lens of EF-SR theory.
Broad Clinical Implications of the EF-SR Theory of ADHD
My EF-SR theory provides a more complex neuropsychological picture of where ADHD originates and how deeply into their lives it can affect those who have the disorder than that depicted by simple inattention, hyperactivity, and impulsivity. Yet that simpler view is what the clinicians have available to work with initially in diagnosing their patients, because it is what the DSM presents. Using my EF-SR theory, we can begin to see where the DSM criteria alone are going to be insufficient for clinicians to rely on, except as a starting point. I offer numerous recommendations in the next chapter concerning the implications of this theory for assessment and diagnosis. But here I can address the question of how we can map the DSM ADHD symptoms onto the EF-SR theory.
The DSM Criteria Within the EF-SR Theory
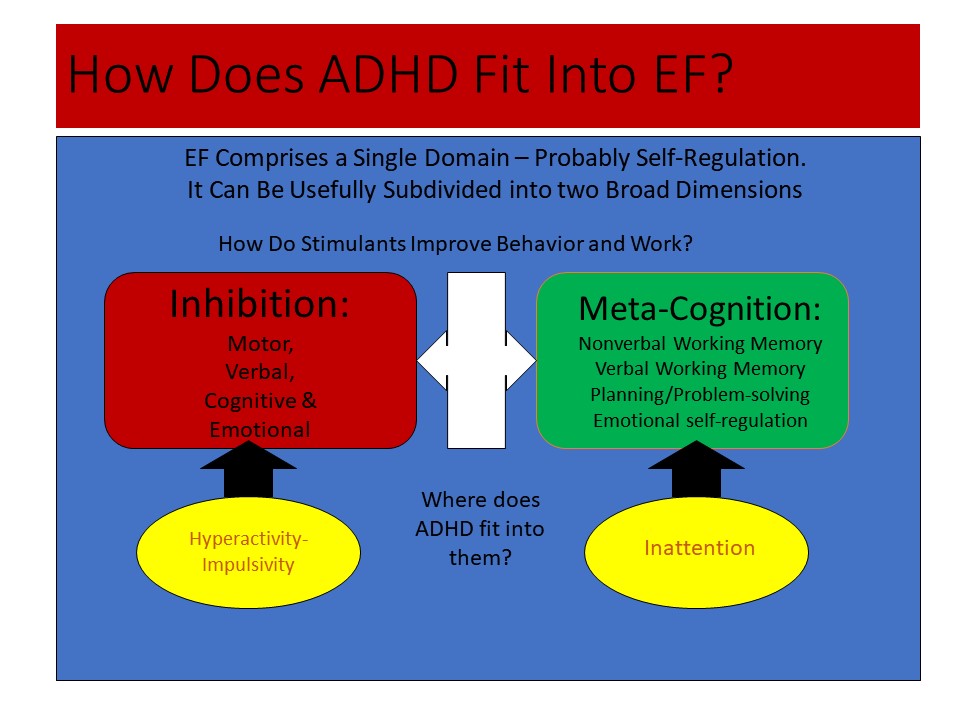
Figure 1, below, shows that executive function comprises one primary construct. All research on executive function measures reveals such a single major construct, which I view as self-regulation. That broad domain of executive function can be divided into two: inhibition and metacognition, which, as shown in the figure, can be further dissected into smaller dimensions of executive functions that are partially coupled to each other. The lower half of the figure shows that the two traditional symptom dimensions of ADHD (inattention and hyperactive-impulsive behavior) are simply subsets of the two main dimensions of executive function. This means executive function is both one thing (self-regulation) and many things (it can be subdivided into narrow-band executive functions related to broader bands of inhibition and metacognition).
Figure 1. How Does ADHD Fit Into EF?
Inattentive to What?
The EF-SR theory can further enlighten us as to the nature of the inattention occurring in ADHD; this is incredibly illuminating for clinically understanding ADHD but also for its differential diagnosis from other mental disorders that adversely affect attention, but in entirely different ways. Consider that attention represents a relationship between a stimulus and the perceptual-motor response of the individual who orients to it, explores it, and then may stay engaged with it. Attention therefore represents a form of stimulus control.
But just what kinds of stimuli or events are failing to control or elicit such engagement from people with ADHD compared to other types of such stimuli or events? Those with ADHD have little trouble paying attention to the now – the momentary present and external environment; in fact, that’s the problem. What is going on immediately in front of them in that moment has a much stronger impact on engagement of their responses than do the private, mental representations about the tasks they have been asked to do or the future they plan for themselves and the behavioral sequences or schemas needed to make that future happen. Those mental representations are held in the two working memory systems – visual and verbal. Thus, what people with ADHD are inattentive to are those mental representations – about tasks, goals, time, and delayed consequences and the future in general – which are thus far less able to capture or control the actions of the individual with ADHD. Such representations are simply not compelling enough to govern their immediate behavior relative to the events playing out around them.
Reframing the inattention of those with ADHD in this way can vastly improve differential diagnosis, helping us distinguish between the inattention seen in ADHD and that seen in many other psychiatric and neurodevelopmental disorders. Disorders such as depression, anxiety, or even autism spectrum disorder can also result in a type of inattention. But people with these disorders are inattentive to events or stimuli in the now – just the opposite of ADHD. Instead, mental representations (thoughts) about their problems, worries, fears, or just their daydreams or mind-wandering (as in autism) are all too powerful in capturing and sustaining the engagement of the individual, decoupling the attention of the person from the external world and shifting it to a focus on mental events. People with these other disorders are mentally preoccupied instead of engaged with the ongoing flow of the now and the things on which they should be working. You can see this in the mental rumination of depression, in memory re-experiencing as in anxiety or PTSD, in self-absorption over possible adverse consequences that might happen to them – improbable as they are likely to be – and certainly in the obsessions of someone with OCD. Likewise, people suffering from the new attention disorder of sluggish cognitive tempo may be preoccupied simply with mental daydreaming or mind-wandering to the point that it is maladaptive or pathological. In sum, where people with ADHD are decoupled from being governed by thoughts and plans related to tasks and goals (the future), and thus overly attentive to the external now, those having other disorders are decoupled from events in the external world and overly attentive to mental events or thoughts.
Emotional Dysregulation as a Core Component
The EF-SR Theory, in contrast to the DSM-5-TR formulation of ADHD, also shows us the important role of poor emotional self-regulation as a central feature of ADHD. The current clinical conceptualization of and criteria for diagnosing ADHD makes no mention of this problem as being an inherent part of the disorder. But overwhelming evidence shows that poor restraint of emotional expression and deficient emotional self-regulation are major problems for people with the disorder. And, during the first 170 years of its medical history, ADHD and its precursor disorder names were believed to involve deficits in emotional inhibition and self-regulation along with the core problems with attention and hyperactive-impulsive behavior. So the idea of ADHD involving problems self-regulating emotion is not a new one.
But beginning in the 1960s, especially with the second edition of the DSM, the symptoms of emotional impulsiveness (which likely overlaps with emotional lability) and deficient emotional self-regulation were divorced from the core deficits of ADHD. Why is unknown, but it was a major mistake, in my opinion. To me, two related constructs comprise the larger one of emotional dysregulation – the impulsive expression of triggered emotions and the deficit in subsequently modifying, moderating, and otherwise effectively coping with them in support of one’s long-term welfare. If noted at all in descriptions of ADHD after 1968, these problems were treated as merely associated ones that may arise in some cases perhaps as a consequence of a comorbid disorder. But now, compelling evidence exists to argue for the return of emotional dysregulation to the status of a core component of ADHD in its conceptualization and DSM diagnostic criteria:
- Emotional dysregulation has a long history as a central feature of ADHD in its clinical conceptualization.
- Current neuropsychological theories of ADHD and executive functioning consider emotional dysregulation a central component.
- The neuroanatomical findings associated with ADHD would likely give rise to commensurate symptoms of emotional dysregulation given that the “hot” or emotional executive circuit provides for the “top down” regulation of the amygdala and, consequently, the limbic system (emotional brain).
- Reviews of this issue reveal various forms of emotional dysregulation (low frustration tolerance, impatience, quickness to anger, and being easily excited to emotional reactions generally) in 21%-72% of cases of ADHD in children (and 32%-78% of cases in adults).
The clinical benefits of including emotional dysregulation are substantial:
- Understanding comorbidity: Returning emotional dysregulation to a central place in ADHD would put clinicians on the lookout for comorbidities with oppositional defiant disorder (ODD), conduct disorder, and anxiety and depression in adolescence. Half of the eight symptoms of ODD involve emotional responses involving temper, anger, hostility, and being easily annoyed; and ADHD is highly comorbid with ODD (65%-85%). Children with ADHD are halfway toward meeting the criteria for ODD by virtue of their impulsive emotions, particularly those involving impatience, frustration, anger, quickness to react, and being excessively excitable or easy to arouse. The social conflict component of childhood ODD, which comprises the other four of the eight ODD symptoms, arises mainly from social learning within families and accounts for association of ODD with later conduct disorder by adolescence.
- Understanding impairments: Emotional dysregulation is a strong predictor of social impairments in several domains of major life activities (peers, work, driving, marriage/cohabiting, and parenting) seen in ADHD even after controlling for any contributions of the traditional ADHD symptom dimensions.
- Differential diagnosis: Including emotional dysregulation as a core component of ADHD would reduce misdiagnosing mood disorders in ADHD as a means of accounting for the emotional difficulties evident in it. Those difficulties are not entirely arising from comorbidity, contrary to the DSM-5-TR. Clinicians can differentiate the emotional symptoms of ADHD from those of mood disorders by focusing on several parameters: Emotions are of short duration, usually situation-specific, often provoked, and so are reactive to a triggering event; and they seem rational or understandable – the emotion makes sense to typical people given the provocation, but the reaction is too impulsive and strong and not moderated by efforts at self-regulation. In contrast, symptoms of a mood disorder show the opposite pattern – the emotion is of a long duration (hence, a mood), it is cross-situational, it is usually unprovoked, and irrational (we find it difficult to understand why the person feels as they do for so long), and it is capricious, labile, and extreme.
- Effective treatments: ADHD medications appear to reduce the emotional dysregulation component of ADHD as much as they do traditional ADHD symptom dimensions, yet each medication category may do so through different neural mechanisms and networks. The evidence base is not yet sufficient to make a definitive conclusion here. And effects of medications on emotion-regulation may be more evident in adults with ADHD than children with the condition. But what evidence does exist points to ADHD medications likely having some positive impact on reducing emotional dysregulation in ADHD. The bottom line is, I believe, that emotional dysregulation should not be ignored when a diagnosis of ADHD is being made or a treatment plan is being devised. Psychosocial interventions for ADHD should also include programs targeted at helping patients with their emotional dysregulation specifically, rather than just reducing traditional ADHD symptom dimensions. Cognitive behavioral therapy programs targeting this aspect of executive-function deficits (and maybe mindfulness-based practices) seem capable of doing so in adults with ADHD, especially if they take medication while undergoing training.
Does Testing Reveal the EF Deficits in ADHD?
Some of my scientific colleagues argue that ADHD is not a disorder of executive functioning, citing the fact that only a minority of people with ADHD fail their executive function tests and test batteries. Unfortunately, this argument does not explain the serious and pervasive deficits in executive function, self-regulation, and the cross-temporal organization of behavior so evident in daily life in those with ADHD, as shown by self- and other-ratings and in clinical interviews. Telling, here, is the substantial body of evidence showing that ratings and observations of executive functioning in daily life are not significantly correlated with the results from those executive function test batteries.
So clearly, whatever executive function tests may be measuring, it is not executive functioning in daily life. Critics of the EF-SR Theory of ADHD see this as just more evidence against rating scales; they see the tests as being the gold standard for assessing executive function. Some also assert the false criticism that such ratings are subjective and so limited in what they can tell us about executive functioning. I and others see this lack of a correlation between tests and ratings as evidence against the ecological validity of the tests – they are not the gold standard for measuring executive function. Moreover, these tests are poor at predicting impairment in major life activities known to be rife with executive function and self-regulation. Multiple studies using rating scales of executive functioning in daily life clearly attest to the fact that a vast majority of patients with ADHD are impaired in the major executive function domains: time management, self-organization and problem solving, self-restraint, self-motivation, and the self-regulation of emotions.
A further criticism of the use of psychometric and other tests for evaluating ADHD is that they have given rise to theories about the nature of ADHD that predict nothing of clinically useful consequence outside of their own test results or those tests with highly similar formats. So, the wise clinician is likely to respond to such theories as delay aversion, a limited cognitive energy pool, etc., with ”So what?” What exactly does it mean in real life to display, for example, delay aversion on a lab task of that construct other than intolerance of delays on tests? What does it predict about the individuals’ life outside the lab and how they are functioning in various important domains? What does it tell us about other risks they are likely to experience given that testing deficit? Does it inform us as to the occupations they should consider or avoid, or the accommodations in work or educational settings they should request? In sum, what does it say about how to help those patients in relevant and important natural settings where impairments exist? And does it inform us about what other treatments may need to be done to address this core problem, such as with aversion to delay?
The answer to them all is a resounding “No.” In other words, you cannot take such deficient test performances to “the clinical bank” because they have no practical cash value, so to speak, for guiding us in helping clients. The lab tasks are bereft of clinical meaning for providing assistance with differential diagnosis or patient care.
The strength and utility of the EF-SR theory of ADHD is not only that it is neuroanatomically and neuropsychologically sound but that it leads to astute diagnosis and helpful treatments for each individual patient – treatment recommendations that would not arise from other theories of ADHD or of executive function.
The EF-SR Theory Leads to Treatments That Help in Real Life
If the maxim “There is nothing so practical as a good theory” is true, then the EF-SR theory is a good one. It is, above all else, practical in its clinical implications.
Treatments That Help Patients Do What They Know When They Need to Use That Knowledge
Executive functions allow people to show what they know in their functioning in daily life activities to improve their longer-term welfare. But ADHD interferes with the connectivity of the knowledge brain (posterior hemispheres) with the performance brain (frontal executive systems). Therefore, ADHD should be seen not as a problem with knowing what to do but as a problem with doing what one knows and doing so consistently at critical points of performance where such knowledge is most effectively deployed.
The ramifications of this idea are profound. If ADHD is based in EF-SR deficits, then it should not be treated largely with approaches that emphasize knowledge acquisition, such as skill training. Yet most psychosocial treatments try to do so (e.g., social skills training for children, executive function cognitive rehabilitation apps for adults, behavior modification for skill acquisition). These are doomed to fail as they do not address the real problem here: the use of one’s knowledge where and when it would have been beneficial to do so, known as the point of performance.
The point of performance is that place and time in the natural setting where that knowledge is useful to employ to improve the consequences for oneself (and often others). It is the application of knowledge in daily life that is the problem here, not ignorance of knowledge or stupidity. To improve a performance disorder, one alters points of performance to prompt individuals to show (utilize) what they know and reinforce the repeated use of the knowledge there. In other words, to be effective, psychosocial treatment for ADHD and executive function disorders must involve altering key elements of the environment to prompt people to recall and then use what they know for better adaptive functioning in that setting and context.
Treatments That Rearrange the Environment to Compensate for Executive Function Deficits
Treatments and remedies that help patients reduce the impact of executive function deficits by modifying the environment are discussed in more depth later in this course. These are some examples:
- Deficient working memory is an obstacle to success in school, at work, and in all social settings, so critical information must be offloaded and externalized to other storage devices in order to guide task performance. Think sticky notes, reminders, journals, to-do lists, and calendars.
- ADHD creates time blindness, so shorter tasks require external time reminders, and longer tasks call for timers plus breaking tasks down into smaller units or quotas.
- ADHD creates motivation deficit disorder, so to keep them working toward goals, those with the disorder need more external rewards, more often, and more frequent accountability to others.
- Mental problem-solving is very difficult in ADHD, so elements of the problem need to be made manual and tangible. For children, think marbles to count, a number line, or an abacus to use in support of mental arithmetic. For adults, think about software that can represent components of a task, such as those used in interior decoration, architectural design, accounting spreadsheets, word processing, musical composition, etc. Or think about the trades where the task is already manual, the components are physical, the goal is more immediate, and supervision and accountability by peers and foremen more immediate and frequent.
- ADHD drains the executive function resource (effort) pool quickly, so patients need smaller work quotas, frequent breaks from work, periodic movement before and during work, and other accommodations and supports ranging from encouraging self-talk, to using external pictures of goals, to self-pep-talks, medication, and maybe even periodic sips of sweetened beverages to get to replenish the effort pool.
Medications for EF-SR Deficits
ADHD medications are known to act on the EF-SR brain substrates and networks and thus improve the executive functions. Those altered or malformed substrates and networks come into being during development and function as they do based on suites of atypical genes that create problems in the regional formation, integration, and ongoing functional connectivity interacting with or resulting from other etiologies that can likewise damage them. Using such neurogenetic medications will reduce the EF-SR deficits, albeit mostly temporarily, and thus reduce the likelihood of impairments in these various major domains of daily life. More specific recommendations to address the various EF-SR deficits posed by ADHD in the natural ecology are discussed later in this course.
Diagnostic Criteria
Between 1980 and the present, efforts have been made to develop more specific guidelines for the classification of children as ADHD. These efforts have been based increasingly on an empirical approach to developing a taxonomy of child psychopathology. Although guidelines appeared in the DSM-II (American Psychiatric Association, 1968), these comprised merely a single sentence along with the admonition not to grant the diagnosis if demonstrable brain injury was present. A more concerted effort at developing criteria appeared in the DSM-III (American Psychiatric Association, 1980), though still unempirical. These criteria were not examined in any field trial but were developed primarily from expert opinion. In the next revision of the DSM-III (American Psychiatric Association, 1987), an attempt was made to draw upon the results of factor-analytic studies of child-behavior rating scales to aid the selection of symptoms that might be included for ADHD. A small-scale field trial employing 500 children from multiple clinical sites was conducted to narrow down the potential list of symptoms, and a cutoff score on this list was chosen that best differentiated children with ADHD from other diagnostic groups.
In DSM-IV (American Psychiatric Association, 2000), the criteria were based on a better field trial and more thorough analysis of its results. Despite the increasingly empirical foundation of the DSM, there remained a few problems with these criteria having to do with developmental sensitivity to the disorder, possible gender bias in diagnosis, an empirically unjustified age of onset of seven years old, and a vexing requirement for cross-setting impairment that is compounded with the problem of poor parent-teacher agreement. Also problematic for the generality of these criteria, is the fact that the field trial used primarily male children, ages four to 16 years old, who were largely of Caucasian ethnicity. Consequently, adjustments or allowances must be made when one wishes to apply the DSM criteria to females, young adults, and non-Caucasian ethnic groups. For example, the symptoms of “often leaves their seat” or difficulties with “playing quietly” may be less relevant to adults with ADHD. Moreover, children whose onset of symptoms was sometime during the childhood years (prior to 13) should be considered as having a valid disorder rather than adhering strictly to the DSM-IV age-of-onset of seven years old as the demarcation of a valid case of disorder.
Where sex differences exist, they indicate that girls with ADHD show less severe symptoms of both inattention and hyperactive-impulsive behavior, especially in school, fewer symptoms of Oppositional Defiant Disorder (ODD) and Conduct Disorder (CD), greater intellectual deficits, and more symptoms of anxiety and depression than do ADHD boys. Some recent studies indicate that girls with ADHD may employ more relational aggression than their non-ADHD peers. However, the symptoms per se differ little between the sexes, even though the age at referral, comorbid disorders, and domains of impairment may differ (Babinski, 2024).
The publication of the DSM-5 in 2013 brought with it a few changes to the DSM-IV criteria. While the original 18 symptoms from the DSM-IV remain in use, as do the two dimensions for their presentation, they are followed by clarifications in parentheses to guide clinicians in applying those symptoms to teens and adults. The threshold of six of nine symptoms on either of the two lists of symptoms remains for application to children and teens. But for adults, this threshold is reduced to five symptoms. The requirements in DSM-IV that symptoms occur often or more frequently, that they be developmentally inappropriate, and that they have persisted for at least the prior six months are all carried forward into DSM-5 and DSM-5-TR. The age of onset has been adjusted upward from seven to 12 years of age, consistent with evidence that the lower onset was invalid, too restrictive, and contributed to clinical unreliability of diagnosis.
Also remaining are the requirements for symptoms to be impairing across several settings and that there be impairment in major life activities. A new requirement is that symptoms given by self-report must be corroborated through someone else who knows the subject well or through other sources. The subtypes have been removed respecting abundant evidence that ADHD is a single disorder that varies in severity in the human population, which is not changed by the fact that some people have more inattention than hyperactive-impulsive symptoms and vice-versa. Even so, clinicians will be provided the opportunity to specify which symptom dimension may be more predominant, as in ADHD Predominantly Inattentive Presentation. There is a Predominantly Hyperactive-Impulsive Presentation and then the traditional Combined Presentation. Finally, ADHD can now be diagnosed with autistic spectrum disorders, just as it can be with many other disorders; a comorbidity previously precluded in DSM-IV.
Principles for Diagnosing ADHD Using EF-SR Theory
For all the reasons laid out above, ADHD must be diagnosed thoughtfully, based on multiple intertwined factors, with executive function and self-regulation deficits understood as the roots of the disorder, and with promoting patients’ healthy functioning throughout life as the primary goal. The following are the principles I have found most useful in guiding the diagnostic process, along with their informational underpinnings from theory and research.
Principle 1: Start the Diagnostic Process with the DSM-5-TR Criteria – But Don’t Stop There
The diagnostic criteria used to recognize ADHD, as defined in DSM-5-TR, are the most scientifically validated to date relative to earlier editions and are based on hundreds of studies as well as expert consensus opinion. They can be summarized as follows:
- Manifests six or more of nine symptoms of either inattention or of hyperactive-impulsive behavior (five symptoms for adults);
- Symptoms are developmentally inappropriate;
- Have existed for at least six months;
- Occur across settings (two or more);
- Result in impairment in major life activities;
- Developed by age 12 years;
- Are not best explained by another disorder; and
- Can appear as three “Presentations” [not Subtypes]: Inattentive, Hyperactive, or Combined.
Advances in developing diagnostic criteria over the prior editions of the DSM have certainly resulted in more precise specification of symptoms, along with two symptom lists; an emphasis on childhood or early adolescent onset of the disorder in most cases; and a requirement for both cross-setting pervasiveness of symptoms and evidence of impairment in one or more major life activities. Even so, numerous evidence-based recommendations were made to the committee tasked with revising the ADHD criteria for improving their rigor and diagnostic accuracy, as well as for better representation of what was known about the core problems inherent in the disorder. Sadly, many of the recommendations were rejected by committees higher up in the organization, apparently partly out of fear of significantly increasing the prevalence of the disorder. Though the few revisions that were finally accepted were commendable improvements, they were half-measures.
Moreover, these criteria can be further improved and adjusted when viewed through the lens of the EF-SR theory. By incorporating more of the recommended revisions to the old DSM criteria and improving the sampling of EF-SR deficits in the symptom lists, you can use even more rigorous and representative criteria than the DSM-5-TR.
DSM-5-TR Does Not Fully Capture ADHD Because the Criteria Are Not Based on the EF-SR Theory
The official criteria now emphasize the neurodevelopmental origins of ADHD, based on the roles played by genetics (and possibly epigenetics) as well as nongenetic neurological factors in its etiology, but they do not go so far as to use this understanding to conceptualize ADHD as a disorder of EF and SR. This limitation narrows the concept of ADHD, trivializes its nature to just an attention deficit, and detracts from the focus that diagnosing clinicians must maintain on the wide-ranging deficits in executive function and self-regulation inherent in ADHD and the impairments caused by them. It restricts diagnosis and ultimately treatment for many patients.
Presentations, Not Subtypes
DSM-5-TR no longer conceptualizes ADHD as comprising three separate subtypes as if they were qualitatively distinct categories. This change makes sense since there is little if any evidence of meaningful differences among the earlier subtypes. Instead, ADHD is now seen as a single disorder representing the extreme end of a continuum that can vary in the population in each of its two highly interrelated symptom dimensions. This is merely a way for clinicians to note the relative severity of symptom dimensions at the present moment and not a signal of qualitatively distinct and lasting types, and it creates two problems:
- EF-SR theory argues that those ADHD symptom dimensions reflect larger ones involved in EF (executive inhibition and metacognition).
- A subset of cases fitting into the primarily inattentive presentation may not be ADHD at all but rather represent a second attention disorder known as sluggish cognitive tempo (SCT), that has recently been relabeled cognitive disengagement syndrome (CDS) (see Becker, et al., 2022 for a recent review of research findings). This presentation could be viewed as a disorder that is distinct from yet partially overlaps with ADHD. It is important to identify because of its unique explanatory power in predicting correlates, comorbidities, outcomes, and even treatment response. Placing SCT (CDS) cases into the inattentive presentation is fine as far as documenting a diagnosis for the sake of insurance reimbursement or institutional data collection goes, as there is nowhere else to designate it officially, but understand that it misrepresents (misdiagnoses) SCT (CDS) as if it were ADHD (or what some clinicians are calling ADD) when the evidence to date shows it certainly is not.
ADHD Can Now Be Diagnosed in the Presence of ASD
This is a welcome change, because it is now known that the comorbidity of ADHD with autism spectrum disorder is substantial and not just a secondary consequence of having ASD (see my other course on ADHD in children for a discussion of comorbidity).
Added Qualifier Symptoms
While the symptom lists for ADHD in DSM-5-TR remain the same, qualifier symptoms have been added parenthetically to assist clinicians with understanding the expression of that symptom at older ages beyond childhood. There are at least three problems with these clarifiers:
- A study that Laura Knouse and I conducted suggested that those clarifications may actually represent newly invented and separate symptoms of the disorder, yet none of these clarifications arose out of prior research that tested them for their affiliation with ADHD, for their relationship to the root symptom they are supposed to clarify, for their accuracy in detecting ADHD, or for their relationship to impairment in major life activities – all essential for inserting new symptoms into such widely used clinical diagnostic criteria for a disorder.
- Adding such new and untested symptoms could broaden eligibility for the disorder by up to 6% in older teens and adults – but without resetting the threshold for determining presence of the disorder (six symptoms for children, five for adults).
- Some clarifications (e.g., internally distracted) are as highly correlated, or more so, with anxiety as with the root symptom, which could lead to cross-contamination of the ADHD criteria with those of another disorder.
These clarifications also were not informed by any theory of ADHD. So, until the status of the parenthetical clarifiers is better researched, clinicians should likely ignore them in making a diagnosis of ADHD in a teen (or an adult) if the goal is consistency in identifying comparable cases between the new DSM-5-TR and the earlier DSM-IV it replaced.
Surmounting Other Shortcomings of the DSM Criteria
Various limitations have been evident in the DSM criteria across the manual’s many editions. It’s important to be aware of those that persist and how to deal with them in order to produce the most accurate diagnosis for your patients.
1. Particularly when assessing adolescents (or adults), don’t place so much emphasis on the hyperactive symptoms.
Six symptoms out of nine on the DSM list reflect excessive activity, even though for at least the last 40 years impulsivity has been viewed as just as much if not more involved in ADHD as hyperactivity. Hyperactivity is at best reflective of early childhood disinhibition of motor movement and declines so steeply over development that such symptoms are of little diagnostic value by late adolescence and certainly by adulthood. This is one reason clinicians before the 1980s thought the disorder was outgrown by adolescence. Today the symptom list is losing its sensitivity to detecting true disorder over development.
2. Look for additional symptoms of impulsivity.
Poor inhibition should be reflected not just in speech (currently the DSM criteria include only three verbal symptoms) but in other domains such as motor behavior, cognition, motivation, and emotion. Ask parents whether their children:
- Often fail to consider the consequences of their actions;
- Have trouble motivating themselves to persist toward goals;
- Have trouble deferring gratification or waiting for rewards;
- Lack willpower, self-discipline, drive, determination, and “stick to it-itiveness”; or
- Seem unusually impatient, easily emotionally aroused, easily frustrated and quick to anger.
None of these aspects of disinhibition or poor self-regulation are included in the DSM-5-TR (or earlier) criteria, yet abundant research shows they are as common in people with ADHD as are the traditional DSM symptoms and, with age, more so than those of hyperactivity. Be sure to ask about them anyway.
3. Use rating scales of ADHD symptoms that have their norms broken down by gender and not just age.
The DSM-5-TR criteria fail to recognize that females may be as impaired as males, but at lower symptom thresholds because (a) females become impaired in certain domains of functioning at lower levels of symptoms than do males, and (b) males were overrepresented in field trials for earlier versions of the DSM, thus making the symptom threshold male-biased. Research suggests that females in the general population, at least in childhood and adolescence, do not show as much of the symptoms as their male peers, making it harder for a female to meet the DSM criteria even though she may be just as impaired as a male.
4. Think of inattention as metacognitive or other executive function deficits in daily life, particularly those reflecting self-awareness, working memory, poor self-organization, poor emotional self-regulation, and deficient time management.
That way, you will know to go beyond focusing merely on DSM symptoms in your assessment of your clients in interviews and in your selection of rating scales, among other assessment methods. You will also know in your open-ended initial interview to listen for these types of complaints in order to better help you identify whether ADHD is present or not. You also can better understand the pervasive impact of clients’ symptoms on their daily functioning in major life activities as they explain to you all of the domains in which they are ineffectively functioning. Furthermore, you can better explain the nature of their disorder to them in the feedback conference when your evaluation is completed, allowing them to better understand why their condition is so serious, impairing, and pervasive across major domains of life. It will also help you to appreciate why teens (and young adults) may seem to be outgrowing ADHD, based on DSM criteria, when they are far less likely to be outgrowing their EF-SR deficits and may even be demonstrating increased impairment with age.
What follows are the most telling symptoms of EF deficits in each domain of EF in daily life from my EF rating scale for children and teens. Consider reviewing them during the interview if you do not use such a rating scale in your evaluation:
The 20 Most Pertinent EF Items from the Short-Form Interview from the Barkley Deficits in Executive Functioning Scale – Parent Interview
(The item becomes a symptom when it is endorsed as occurring often or very often.)
Time Management:
- Procrastinates or puts off doing things until the last minute.
- Has a poor sense of time.
- Wastes or doesn’t manage their time well.
- Has trouble planning ahead or preparing for upcoming events.
Self-Organization
- Has trouble explaining their ideas as well or as quickly as others.
- Has difficulty explaining things in their proper order or sequence.
- Can’t seem to get to the point of their explanations.
- Doesn’t seem to process information quickly or accurately.
Self-Restraint (Inhibition)
- Makes impulsive comments.
- Likely to do things without considering the consequences for doing them.
- Acts without thinking things over.
- Doesn’t stop and talk things over with themselves before deciding to do something.
Self-Motivation
- Takes short-cuts in their chores, schoolwork, or other assignments and does not do all that they are supposed to do.
- Does not put much effort into their chores, schoolwork, or other assignments.
- Seems lazy or unmotivated.
- Inconsistent in the quality or quantity of their work performance.
Emotional Self-Regulation
- Has trouble calming themselves down once they are emotionally upset.
- Not able to be reasonable once they are emotional.
- Cannot seem to distract themselves away from whatever is upsetting them emotionally to help calm down. Can’t refocus their mind to a more positive framework.
- Not able to re-channel or redirect their emotions into more positive ways or outlets when they get upset.
From R. A. Barkley (2012). Barkley Deficits in Executive Functioning Scale – Children and Adolescents. New York: Guilford Press. Copyright Guilford Press. Reprinted with permission.
5. Don’t adhere too rigidly to thresholds for meeting diagnostic criteria when there are clear signs of significant impairment.
You are not making a dichotomous decision – disorder or no disorder – or dealing with symptoms whose presence or absence creates a sharp distinction between the two. Keep in mind that ADHD (and EF-SR)is not a category but a dimension. Empirical research asserts that ADHD falls along a continuum in the general population. It is a developmental disorder distinguished more from others by a quantitative difference from normative behavior than as a qualitatively distinct category. So, you will see clients who don’t meet all of the DSM criteria yet who are experiencing impairment and seek out your assistance to alleviate or at least compensate for it. As practitioners, we are valued by society not so much because we can make diagnoses but because we relieve suffering; the rendering of a diagnosis is a means to that end and not the end itself. This means you should diagnose ADHD if:
- Your clients or their caregivers state that the child or teen has a high number of ADHD (and EF) symptoms (place above the 20th–16th percentile or so in severity) and there is evidence of impairment in major life activities (harm), even if the client fails to meet all DSM-5-TR criteria.
- Symptoms developed sometime during development, usually before age 21-24 or so, and meet all other criteria for the disorder. DSM-5-TR has raised the age of onset for ADHD from age 7 to age 12, but research repeatedly shows that both patients and those who know them well are not reliable or accurate in recalling the age of onset of the symptoms and hence, the disorder. It is a mistake therefore to consider age of onset in diagnosing ADHD, all else hitting the stated thresholds.
6. Always consider the source of information when assessing a child or teen for ADHD.
The DSM has a requirement for cross-setting occurrence of some symptoms in the diagnostic criteria, but some care must be taken not to confuse that with differences in the reports of others being called on to provide information about the individual. At the individual level of analysis, there can be substantial differences in the number and severity of symptoms reported by different observers across the different contexts they supervise. For example, it is well known that parent and teacher agreement on any dimension of psychopathology in children or teens is notoriously low, with correlations averaging just 0.25%-0.30%. To avoid conflating such natural reporter disagreement with cross-setting occurrence, the DSM should be understood to require that only one or more symptoms need to be present in any given situation as reported by one source, while more symptoms producing impairment may be reported in other settings by other sources. It is the total number of different symptoms endorsed across such reporters that needs to rise to the required symptom threshold (six for children, five for adults). You do not need six (or five) from all sources.
The same caution about conflicting observer reports applies to comparing self-reports by children and teens with ADHD and their parent or others’ reports of their ADHD symptoms. Up until the client is in his or her twenties, the correlation between self- and other reports is only modest, reflecting low degrees of agreement. The EF-SR theory of ADHD explains this phenomenon: the development of executive functions that create self-awareness lag behind in those with ADHD. Therefore, you should adhere to the newly inserted criterion in DSM-5 to corroborate what patients are reporting through another source. If no parent, sibling, or long-term caregiver is available, then available archival records may have to suffice, such as earlier medical/psychiatric records, educational transcripts, or report cards, driving records, work history, etc.
7. Think of – and explain – ADHD as being the diabetes of mental health.
DSM-5-TR specifies that impairment may exist in home, educational, peer, or occupational settings, but, because it still focuses on ADHD as deficits in attention or activity regulation, it does not convey how far beyond these domains ADHD has an adverse impact. When you view ADHD as founded in deficits in executive functions and self-regulation, which are requirements for functioning well in most domains of life, you can not only better understand why your clients are struggling to function effectively in so many domains of life and health, but also better explain to them and their loved ones why that is the case. And why it is imperative that the disorder be treated on an ongoing basis as if it were the diabetes of psychiatry – an important implication of adopting the treatment framework provided by the EF-SR theory.
8. Don’t assume that ADHD disappears in adolescence.
DSM criteria are progressively less developmentally sensitive with increasing age. They lose their capacity to detect true disorder to some extent by adulthood. But if we apply developmentally relative criteria for a diagnosis, such as exceeding the 93rd (+1.5 SD) or 98th (+2 SD) percentile relative to same-age peers and requiring evidence of impairment, up to 56% and 49% of childhood cases, respectively, continue to be symptomatic even if not fully diagnosable by DSM criteria. And if we had employed more symptoms of EF-SR deficits beyond the traditional ADHD symptoms, even more cases would be classified as developmentally deviant. Note that using a developmental approach to diagnosis identifies twice as many cases as being persistent in their disorder as do the DSM criteria. If the presence of impairment was the only criterion employed, then over 80%-85% were still impaired in one or more daily life activities by adult follow-up. During my research collecting population representative norms for my EF rating scales (see separate manuals for children and adults), I observed that despite the well-known decline in ADHD symptoms in the general population with age from childhood into adulthood (and onward) [as seen on ADHD rating scales], there was little or no obvious decline in the various EF components on those ratings across childhood (ages 6-18), such as for self-organization, time management, self-motivation, self-restraint, and planning/problem-solving. What this likely means is that the ADHD symptom lists are not capturing the far wider range of EF deficits associated with this disorder that are not declining with development as much as are the more childhood-focused traditional DSM symptoms.
Principle 2: Understand the Importance of Impairments vs. Symptoms
What qualifies ADHD as a “real” or valid disorder, in my opinion, is that it meets the well-reasoned criteria for a harmful dysfunction as set forth by Jerome Wakefield. Wakefield defined mental disorders as:
- Dysfunction(s) in one or more evolved psychological adaptations (abilities) that are universal to the species (part of the human design)…
- that lead to harm to the individual, including increased mortality, morbidity, and impairment (ineffective functioning in major life activities).
Abundant evidence shows that ADHD easily meets both criteria, so it is clearly a valid disorder.
But if the dysfunction is on a continuum, as is ADHD, and not categorical, at what point does it become a disorder? When symptom severity reaches the point where it causes harm – adverse consequences or impairment - for the individual (the environment kicks back). This explains why I encourage clinicians to use impairment as an important factor in diagnosing ADHD even when symptom criteria are below the DSM thresholds.
Impairments are far more wide-ranging and multifarious than the DSM criteria indicate – in large part because the DSM still views ADHD as a disorder of inattention and hyperactivity rather than more broadly as a disorder of self-regulation. To render an accurate diagnosis, it’s important to look at how ADHD can affect children and teenagers in every domain of life and assess whether some clients are exhibiting such harms. Later, I list some of the instruments you can use to measure impairments. The Figure below offers an overview of the domains of impairment for both children and adults:
Figure 2. Impairments Linked to ADHD
For diagnostic and assessment purposes, here are impairments most likely to affect children that you can evaluate:
Family Relationships
It is essential that you evaluate the family while assessing a child or teenager for ADHD, not merely in the course of ascertaining whether the child has ADHD, but also to uncover all the factors that will likely affect treatment. A large amount of research has shown that a child’s ADHD can have a negative impact on the child’s relationship with parents and with siblings. If the parents or siblings also have ADHD or other psychiatric diagnoses, the problems are often compounded and bidirectional. Learning what types of problems exist in the family during the diagnostic process can help you develop a comprehensive treatment plan that stands the greatest possible chance of helping the child with ADHD and, in turn, the whole family.
Principle 3, below, will help you apply a neurogenetic framework to your approach to evaluating a child or teen for ADHD, including the importance of considering whether biological relatives also have ADHD or other relevant mental health problems.
Educational Impairments
One of the most well-documented domains of impairment for all age groups of people with ADHD is that of education. When ADHD is viewed through the lens of the EF-SR theory, the reason for this is obvious. Few domains apart from occupational performance in adults are as demanding of self-regulation and delayed gratification as schooling. An overview of the research evidence follows:
- The vast majority of people with ADHD experience impairment in the educational setting, probably well over 90%. And the extent of impairment is more severe in this domain than in most, if not all, others.
- People with ADHD generally manifest lower preschool academic readiness skills, lower academic achievement skills after entering formal school settings, greater skills deficits, widespread performance deficits in core academic subjects, and poorer academic-enabling behaviors such as self-organization, time management, problem solving, that make one available for learning. These are in addition to their other ADHD symptoms, EF deficits, peer relationship problems, comorbid psychiatric disorders, and health problems as identified here and in later chapters in this course.
- In academic skills, people with ADHD show significant deficits in reading, math, spelling, and handwriting competencies as well as a higher probability of qualifying for SLDs (33%-45%+), as discussed in Chapter 4.
- Performance deficits include high rates of off-task behavior, variable on-task behavior, less efficient approaches to work performance, careless work behavior, inability to sustain motivation to work as long as typical children, and reduced self-monitoring and self-correction of work. Moreover, their emotional self-regulation deficits and impulsive emotional displays result in significant behavioral management issues for teachers and are the single best predictor of peer rejection in school.
- Deficits in academic performance are more a function of the degree of EF symptoms than of the hyperactive-impulsive symptom dimension, which contributes more to disruptive behavioral management issues in school and difficulties in less-supervised settings (lunchroom, hallway, bus, playground) and outside-of-school risks.
- Significant transitions in academic settings over development, such as the shift from elementary to middle school, from the latter to high school, or – for the minority who try it – from high school to college, may be associated with a worsening of symptoms and further impairments. That is due in part to a reduction in external structure, assistance, and supervision and to the increased emphasis on self-regulation and independence associated with such transitions.
- Follow-up studies also show higher than typical rates of adverse academic outcomes, such as grade retention, suspensions, and expulsions; and possibly failure to complete compulsory education. Fortunately, the latter risk has declined lately, probably due to the inclusion of ADHD in the special education laws that provide more recent generations with more assistance in completing school or a modified avenue through which to graduate than was available to earlier generations. Even so, cases with ADHD are less likely than control groups to enter college or, if they enter, to graduate from college, although the most intelligent may do so.
Assessing the educational problems associated with ADHD is complex and should include tests of basic achievement skills. For professionals working in school settings, the evaluation might also include rating scales of academic performance and school enablers, along with curriculum-based assessment and direct observations of in-school functioning, among other more ethological approaches to documenting difficulties (see textbook by DuPaul & Stoner in References).
Interventions for the educational impairments of children and teens with ADHD need to target not only the modification of ADHD symptoms and related problematic behaviors, but also academic skills, performance-related behavior, and academic-enabling abilities if improvements in more than just behavior are to be achieved. Additional interventions may be needed to target directly the increased risk for dropping out of school.
In view of the above, you need to be very familiar with special educational laws and services so that you can better advise parents of services for which their children may be eligible and how to access them. Some clinics have gone so far as to hire educational specialists with a background in special education to work as a liaison between their clinic and the school system so as to further assist clients with their educational needs. Also, you should be very familiar with the types of psycho-educational and behavioral management methods that have some evidence-base so that you can optimally counsel families and even specific teachers about classroom management strategies and curriculum adjustments. Whether advising children or teens, you may find it helpful to review the texts by DuPaul and Stoner on assessing and managing ADHD in school as well as that by Lewandowski and Lovett on testing accommodations for students with disabilities.
Health Impairments
Research evidence is mounting that ADHD increases mortality, risk of injury, and a panoply of adverse health outcomes. Obviously, a child being evaluated for ADHD should have a physical checkup to rule out non-ADHD causes of ADHD symptoms and related impairments. But in general, a diagnosing clinician should be looking for indications of accidental injuries and poisonings, poor dental hygiene and trauma, motor and language delays, disrupted sleep, seizures, and migraines in children that could be connected to ADHD. As children mature, the health risks multiply, largely due to risky behaviors caused by deficits in self-regulation. Thus, by adolescence, clinicians must be attuned to additional health adversities related to risky sex, sexually transmitted disease, risk for pregnancy, obesity, impulsive eating pathology (in females), adverse driving outcomes (citations, crashes, revocations), alcohol, tobacco, marijuana, and other drug experimentation or abuse, and Internet addiction, among others.
This area is an example of how illuminating it can be to look at ADHD as more than a simple disorder of attention. Imagine a teacher reports that a student you are evaluating gets easily distracted and behaves very impulsively in class. If asked, the physical ed teacher could report that this child has minor but frequent injuries in gym class despite safety warnings. The physical ed teacher just thinks the student is overly enthusiastic, and no one at the school has made the connection between this risk-taking sports behavior and the child’s impulsivity in the classroom. But you can – and in the process see the EF/SR deficits that underlie the child’s experiences in all domains of life, including health, and so help the family see the importance of treatment to prevent further impairments in the future.
Just as ADHD is linked to increased adverse consequences in nearly every major domain of life-activity studied to date, so too does it adversely impact lifestyle, diet, health, and other aspects of wellness. Throughout the ordinary day, people must make countless choices about eating, exercise, avoidance of hazardous substances, use of alcohol, tobacco, and other legal substances, exercise, use of over-the-counter as well as prescription medications, personal hygiene, dental health, sexual behavior, driving, and risk-taking in general. While these decisions are usually more the domain of adolescence than childhood, teenagers are involved in such choices at earlier and earlier ages, so it’s important for clinicians to talk to parents about these risks even if their child isn’t facing them right now. Involving, as it does, disinhibition, a preference for small immediate over delayed larger consequences, and poor self-regulation generally, ADHD leads to a variety of unhealthy choices across all of these choice-points that, cumulatively, will have a negative impact on their health and risk for medical illness as well as for earlier mortality and a shortened life-expectancy (Barkley et al., 2019; O’Nions et al., 2025). Impulsivity is also the single best predictor of suicide attempts and successful suicide in high school for teens with ADHD.
For instance, ADHD in children - and more recently in adults - has been repeatedly linked to an increased risk (two to five times) for accidental injuries of all types (trauma, burns, poisonings, penetrating eye injuries, etc.), for more severe injuries, as well as for repeated injuries. The comorbidity of ODD/aggression with ADHD in children further exacerbates these risks. Likewise, children who are admitted to hospitals due to accidental injuries are three times more likely to have ADHD (approx. 30%) than are children admitted for other reasons. The adverse driving outcomes noted earlier, including more vehicular crashes, pose additional opportunities for early morbidity and mortality. And then there is the fact that SRDD further increases the risk for suicidal ideation (along with comorbid depression), attempts (associated with impulsivity), and completions, as noted earlier. The involvement of teens and adults with ADHD in various antisocial activities and intimate partner violence further elevates their risk for greater injury and death.
Clinicians should be alert for health problems that are already a part of a child’s history since they may support a diagnosis of ADHD. Parents should also be informed of the health risks to their children when they have been diagnosed, so that efforts to offset the increased health risks can be incorporated into a treatment plan in which parents can participate.
Principle 3: Always Consider the Neurogenetic Origins of ADHD
ADHD is classified as a “neurodevelopmental” disorder because the evidence for the involvement of neurological, genetic, epigenetic, neurotoxins and other biologically related factors in its occurrence and development is beyond dispute (Faraone et al., 2024). Where there is any role for the environment in etiology, it is through its interaction with primarily genetic and other neurological factors (toxins, infections, trauma) and not through main effects, particularly for social influences. Even then, the environmental factor, such as alcohol consumption in pregnancy, or social deprivation or malnutrition, must be sufficient to adversely affect brain functioning and result in ADHD as a consequence (as found in adoptees from orphanages in poverty-stricken or war-torn countries). Indeed, it is safe to proclaim given the hundreds of studies attesting to these assertions that there is no currently available credible scientific theory of ADHD that can account for its existence by purely social means.
To be clear, social environments
are influential in their impact on ADHD – primarily on the risks for subsequent impairments in major life activities, risks for comorbid disorders, and access to diagnostic, treatment, and educational resources. All of this may impact current and perhaps eventual adult outcomes of the disorder. But the prevailing evidence makes clear that those social factors alone do not create ADHD de novo in an otherwise normal or typical child or teen.
This incontrovertible fact is important in diagnosing ADHD, in treating it, and in helping parents accommodate to the news that their child has this chronic condition, not unlike diabetes, that comes with lifelong health risks and other challenges
but through no fault of theirs concerning how the child is being raised.
Suffice it here to say that what we know about the neurogenetic nature of ADHD makes it plain that a professional evaluation must always include evaluating biological relatives of the child undergoing the assessment, as noted under
Principle 2.
Principle 4: Keep in Mind That the Goal Is Not Just Diagnosis of ADHD, but Differential Diagnosis from Other Disorders
ADHD can be, and often is, confused with other diagnoses involving deficits in attention and impulsivity. As you may have learned in my other course on ADHD in children, one early goal involved in assessment is to rule out these other disorders as the source of the symptoms and impairments a child brings to your office. Yet ADHD also often co-occurs with other disorders, and it will be your job to identify any of those that the client you are evaluating may have in addition to ADHD.
Principle 5: Be Prepared to Confront Myths and Resistance from Parents and Clients (Particularly Teens)
Despite the vast quantity of reliable research evidence accumulated over several decades, misinformation about ADHD still abounds. Being prepared to counter common myths and misconceptions can help you transform skeptical parents into knowledgeable collaborators in a child or teen’s treatment. Myths and misunderstandings such as the following:
“ADHD isn’t real.”
Contrary to reports from various sources, the disorder has not increased wildly in prevalence in recent decades, and is not, therefore, merely a fabricated “affliction du jour.” And it surely has not increased due to the widespread adoption of screen-based technologies on which people spend increasing amounts of their time, or of a diet high in sugar, or any number of other once-claimed environmental causes that, when removed, would resolve ADHD.
ADHD is among the most widely and deeply studied psychiatric conditions known, and prevalence rates are consistent across the world, ranging between 5% and 8%. ADHD appears in all ethnicities, nationalities, and socioeconomic groups (although there is some variation largely related to the latter factor). You can assure parents that these figures may even be slightly high since they include cases that represent that other attention disorder noted earlier, sluggish cognitive tempo. What matters is that ADHD as currently defined is found throughout the world’s populace. Interestingly, however, observations of impairments through development show that children can outgrow the classically defined ADHD diagnosis but continue to have a disorder of EF-SR. You can explain this to parents according to the facts and approach provided in Chapter 5. Understanding the wide-ranging impairments of ADHD viewed through EF-SR theory can help dispel parents’ arguments that their child doesn’t seem at all like others they have known who have been diagnosed with ADHD.
Be cognizant of the fact that many parents, when a clinician delivers a diagnosis of ADHD, are either in denial or, if not, are very susceptible to experiencing a significant amount of grief. No one likes to hear that their child has a debilitating chronic health condition. Be sure to focus on the fact that the purpose of diagnosis is to allow for effective treatment – and that most children offered such interventions will be able to reduce or compensate for their symptoms and reduce potential impairments over a long and fruitful lifetime. You can even suggest that they Google “ADHD success stories” to see the wide range of athletes, celebrities, musicians, chefs, actors, comedians, entrepreneurs, and others who have done well despite the disorder because they got diagnosed and treated for it.
“My child couldn’t have ADHD, because it’s caused by bad parenting, and I know I’ve been a good parent.”
Parents who carry this myth around are often wracked with guilt over whether they have inadvertently caused their child harm. They may have heard others blame ADHD on parents, or they themselves may have been blamed for their child’s atypical behavior by those close to them. No wonder they prefer to reject the entire diagnosis. You can, however, encourage them to accept the diagnosis without taking on the blame.
“Are you sure my child has ADHD? I’ve heard it’s vastly over-diagnosed.”
As noted above, ADHD may seem slightly over-diagnosed simply by virtue of including cases of the inattentive type, or sluggish cognitive tempo disorder. It has also resulted from mainstream media accounts of ADHD that focused on some government reports, especially that of the CDC, that determined rates of ADHD in the U.S. using just a single vague survey question and thus was highly prone to greatly over-identify possible cases of the disorder. On the other hand, the fact that a much higher proportion of boys than girls are diagnosed with ADHD in childhood, and that this gap narrows with age, may indicate that we have been missing cases of ADHD in girls until they mature enough to suffer and report impairments on their own and thus seek evaluation. Also, there is a second age-range of onset for girls associated with the onset of their menses in adolescence that may have further contributed to this under-recognition of girls in childhood. (Other explanations could, however, account for this phenomenon, and more research is needed.) ADHD may even be underrecognized in teenage boys and men because so often, diagnosis has relied on the existence of hyperactivity, which does decline with age, while evidence of executive function and self-regulation deficits does not. When we view ADHD as a disorder of EF-SR, we may in fact discover we have been underdiagnosing ADHD.
“Girls don’t get ADHD, so how can you tell me my daughter has it?”
Thanks to increasing research that includes girls and women (females at birth), we now know that ADHD most assuredly occurs in females and probably in many cases just as young at onset as in boys. The problem lies in the fact that the same EF-SR deficits that exist in boys often manifest themselves differently in girls. Where boys may be “hyperactive” in terms of movement, girls may show this symptom as verbal hyperactivity or increased socializing. And, as noted earlier, girls can have a second age of onset of their condition in adolescence such that by the late teens and early adulthood, ADHD is nearly as common in females as in males.
“Even if my child does have ADHD, why should he/she be treated for something that is actually a gift?”
I have been debunking this persistent myth for years, and yet you’ll find some parents still adhere to it. This may be another response to denial and grief, or a byproduct of the relatively new “neurodiversity” social movement – it’s easier to view ADHD as a “difference” than as a disorder, and it’s more palatable to view ADHD in terms of any benefits that the syndrome may confer. Always point out to parents that their child does have many gifts – strengths that can be capitalized on to help the child overcome ADHD’s impairments. But ADHD has been included in the DSM for good reason: Without treatment, it can severely derail (and even shorten) a child’s life. This claim of ADHD as a gift not only misrepresents the scientific findings on this disorder, but it can minimize the seriousness of the disorder in the parent’s mind and foster false hope to people. After all, if ADHD is really a disorder of EF-SR, then it is undermining one of the most important suites of mental adaptations that humans use to survive and to prosper.
Remind parents that they have come to you for help with problems affecting their child that they have not been able to solve on their own. They have determined that they need professional help. Your diagnosis can lead directly to that help – from special accommodations and services in the educational system, to behavior management skill-building, to medication – to reduce the negative impact of ADHD’s main symptoms. If ADHD were a gift, these forms of support and assistance would never have become available.
By all means, please encourage parents to celebrate those who have coped successfully with ADHD and even succeeded in some occupations well beyond what typical people might have done. Yet neither that coping, nor that success, can be attributed to their ADHD. Instead, it is due to some of the many hundreds of other traits the person possesses in which they may have some talent. People are not good artists, actresses, comedians, musicians, chefs, athletes, TV personalities, and entrepreneurs, etc. because of their ADHD. They are so in spite of it. They just happened to be blessed with exceptional talents unrelated to their ADHD that allowed them to excel even with their ADHD.
People with ADHD are certainly less inhibited. And it is well known that one’s creativity can be enhanced somewhat by being less inhibited than others. Such mildly lower levels of inhibition promote thinking about or even trying far-fetched ideas that others would ignore because they are unusual, impractical, or seemingly irrelevant. This finding among the general population does not mean that people with ADHD who have far more severe disinhibition are even more creative as a result. But it might lead to specific instances in which some already highly gifted, talented, or creative people who happen to have ADHD are somewhat more inventive in their ideas or more likely to take risks in their business or specialty. But that is a very small segment of the total ADHD population. Some of those far-fetched ideas just might pay off handsomely.
Likewise, ADHD conveys to people a high level of energy and typically unfocused activity. This can be directed for good or bad. But if someone with ADHD is also blessed with high athletic abilities or an entrepreneurial talent and is surrounded by loved ones who can channel that excess energy and utilize exceptional area resources to further develop it (e.g., Michael Phelps, Simone Biles, Adam Levine), then good things may come of it. It is this interaction of talent with excess activity coupled with direction by loved ones and their recruiting of resources that can promote that talent and may well help that person to succeed where others with ADHD might not.
Viewing ADHD as a disorder of EF and SR, as in the EF-SR theory summarized above, makes us appreciate just how serious a condition it is and makes it evident why it is linked to so many domains of adverse outcomes.
“If I accept that my child has ADHD, you’re going to want to prescribe medication, and I don’t want my child to take pills that may not be safe.”
That medications for ADHD (or for any other psychiatric disorder) may not be safe and may also be unnecessary is naturally a major concern for many parents. It should not be belittled, as no parent should give a prescription psychoactive drug to a child unquestioningly. Your initial response to this fear can be to assure the parents and the child/teen that all proven interventions will be considered as part of any treatment regimen you or another clinician who follows up on your diagnosis will propose. Nothing will be forced on you, the parent. You can also provide basic statistics on the safety of the medications commonly prescribed for ADHD and get into more detail as treatments are reviewed. The best way to confront misinformation is with more information, so refer parents to other sources for more.
Principle 6: Be Prepared to Follow Up Diagnosis with Appropriate Treatment
This may seem so obvious as to go without saying. But it is sometimes easy to forget, especially in the rigidly structured health insurance system with which we operate, that diagnosis is not an end in and of itself. Depending on your professional circumstances, some clients will transfer to other clinicians for treatment. But even in those cases, you have much to offer in the way of insights to pass on about how your diagnosis informs treatment options.
Always remember that the helping professions do not exist to make diagnoses but to relieve suffering and harm (including impairment). Making a diagnosis is but one means to that end and not the end itself. Throughout the assessment process, you will obviously be taking notes for the client’s file about what recommendations certain findings indicate may be needed to address impairments in various domains of the child or teen’s life. In addition, you should be equipped with:
- A solid foundation of knowledge of all the evidence-based treatment options available today (also knowledge of what is unproven or has been found to be harmful).
- Openness to consulting with specialists as needed, especially educational consultants (for both diagnosis and treatment).
- Familiarity with the services available in your community. Being able to refer clients to needed specialists nearby will be a large part of the benefit you can offer, and having alternatives in mind when local services are in short supply will always be welcome. You are the expert, and parents will greatly appreciate the fact that you are not leaving them with a diagnosis and no way to treat it.
Assessment
Probably the four most important components of a comprehensive evaluation of a client with ADHD are the clinical interview, the medical examination, the completion and scoring of behavior rating scales, and the administration of certain psychological tests to rule in or out high-risk comorbid disorders such as developmental/intellectual delay and learning disabilities. When feasible, clinicians may wish to supplement these components of the evaluation with objective assessments of the ADHD symptoms, such as psychological tests of attention or direct behavioral observations. These tests are not essential to reaching a diagnosis, however, or to treatment planning, but when abnormal findings are detected, they may yield further information about the presence and severity of cognitive impairments that could be associated with some cases of ADHD. The problem is that the presence of normal scores are largely meaningless given the high proportion of ADHD cases that place in the normal range on such tests. In other words, abnormal scores may be meaningful in indicating the presence of a disorder (not necessarily ADHD) while normal scores should go uninterpreted given the high false negative rate of many ADHD tests.
In this course, I describe the details of conducting clinical interviews with parents, teachers, and children/adolescents when it is the child or adolescent who is presenting for evaluation of ADHD. I also briefly discuss the essential features of the medical examination of ADHD children and issues that examination needs to address. This discussion is followed by an overview of some of the most useful behavior-rating scales to incorporate into the clinical evaluation. A brief review of the role of psychological tests and direct observations in the evaluation is then presented. Readers wishing to acquire some of the clinical tools referenced here can find them listed in the References section. The information contained herein was initially drawn chiefly from my earlier chapters on assessment in my Handbook for Diagnosis and Treatment (Barkley, 2015) and more recently from my book, Treating Children and Adolescents with ADHD: What Every Clinician Needs to Know Barkley 2022).
Assessment Issues
Clinicians should bear in mind several goals when evaluating children for ADHD. A major goal of such an assessment is the determination of the presence or absence of ADHD as well as the differential diagnosis of ADHD from other childhood psychiatric disorders. This differential diagnosis requires extensive clinical knowledge of these other psychiatric disorders, and readers are referred to the DSM-5-TR for diagnostic criteria and to textbooks on child psychopathology for a review of the major childhood disorders (see Mash & Barkley, 2014). In any child evaluation, it may be necessary to draw on measures that are normed for the individual’s ethnic background, if such instruments are available, to preclude the over-diagnosis of minority children when diagnostic criteria developed on white American children are extrapolated to other ethnic groups. For further discussion on gender, socioeconomic status, and cross-cultural issues related to diagnosis and prevalence of ADHD, please see the first course in this series titled ADHD: Nature, Course, Outcomes, and Comorbidity.
A second purpose of the evaluation is to begin delineating the types of interventions needed to address the psychiatric disorders and psychological, academic, and social impairments identified in the course of assessment. As noted later, these may include individual counseling, parent training in behavior management, family therapy, classroom behavior modification, psychiatric medications, and formal special educational services, to name just a few.
Another important purpose of the evaluation is to determine conditions that often coexist with ADHD. Their approximate rate of occurrence is:
- Oppositional defiant disorder (ODD; 45-84%)
- Specific learning disabilities (SLDs; 35%-50%+)
- Developmental coordination disorder (DCD; 40%-50%)
- Communication disorders (20%-30%)
- Conduct disorder (CD; 5%-56%)
- Substance use disorders in adolescence (SUDs; 15%-25%)
- Anxiety (25%-50%)
- Depression (up to 30%)
- Disruptive mood dysregulation disorder (DMDD; 20%-25%)
- Autism spectrum disorder (ASD; 15%-25%)
Then, to a much lesser extent, there can be bipolar disorder (BPD; 0%-10%), intellectual disability (ID; 5%-10%), PTSD (5%-6%), tic disorders (TD; 10%-20%), and obsessive-compulsive behavior/disorders (OCB; 2-5%).
Not only must one assess for these comorbidities, but one should consider the manner in which these conditions may affect prognosis or treatment decision-making. For instance, the presence of high levels of physically assaultive behavior by a child with ADHD may indicate that a parent training program is contraindicated, at least for the time being, because such training in limit-setting and behavior-modification could temporarily increase child violence toward parents when limits on noncompliance with parental commands are established.
Or, consider the presence of high levels of anxiety specifically – and internalizing symptoms more generally – in children with ADHD. Research shows that such symptoms may be a predictor of poorer responses to stimulant medication, although the point is arguable due to mixed results across studies on this issue. Similarly, the presence of high levels of irritable mood, severely hostile and defiant behavior, and periodic episodes of serious physical aggression and destructive behavior may be early markers for Disruptive Mood Dysregulation Disorder. If coupled with mania, grandiosity, and sleep or sexual disturbances, they may be early markers for later Bipolar Disorder (Manic-Depression) in children. Oppositional behavior is almost universal in both disorders, though of a more extreme nature than on its own. Such a disorder is likely to require the use of several psychiatric medications in conjunction with a parent training program and occasionally even inpatient hospitalization.
A further objective of the evaluation is to identify the pattern of the child’s psychological strengths and weaknesses and to consider how these strengths and weaknesses may affect treatment planning. This identification may also include gaining some impression as to the parents’ own abilities to carry out the treatment program as well as the family’s social and economic circumstances and the treatment resources that may (or may not) be available within their community and cultural group. Some determination also must be made as to the child’s eligibility for special educational services within his or her school district if eligible disorders such as developmental delay, learning disabilities, or speech and language problems, are present.
As the foregoing discussion illustrates, the evaluation of a child for the presence of diagnosable ADHD is but one of many purposes of the clinical evaluation. A brief discussion now follows regarding the different methods of assessment that may be used in the evaluation of ADHD children.
Information Obtained
at the Time of Referral
The initial phase of a diagnostic interview might not be conducted by the clinician but by a support staff member. The initial phone intake provides invaluable information when conducted by a well-trained individual; otherwise, it is a lost opportunity. When a parent calls to request an evaluation, it is useful to collect the following information:
- What is the reason for the parent’s request? Is it an open-ended question, such as “What’s wrong with my child?”, or a specific one, such as “Does my child have ADHD?”
- Who referred the family? Is the family self-referred because members recently read a newspaper article or saw a television program which raised their concerns? Is the family referred by the child’s school because of school-related rather than parental concerns? Is the family referred by a pediatrician or another health or mental health professional who suspects ADHD but wants diagnostic confirmation?
- Has the child been previously evaluated or tested by someone else? Is the family looking for a second opinion, or for a reevaluation of ADHD that was diagnosed when the child was younger?
- Does the child have any other diagnosed conditions, such as mood disorders, substance abuse, or other developmental delays? Has the child been tested and diagnosed by the school system to have learning disabilities or cognitive delays?
- Is the child already on medication? Are the parents seeking an evaluation of their child’s response to medication rather than a diagnostic evaluation? If the child is on stimulant medication, would the parents consent to withholding the medication on the day of the evaluation, or even the day before, to allow observations of the child off their medication during the evaluation?
The content of the diagnostic interview is influenced by all these factors and important information can be collected and reviewed ahead of time when the reason for the referral is clear.
Once the child is referred for services, the clinician must glean some important details from the telephone interview. This information also allows the clinician to set in motion some initial procedures. In particular, it is important at this point to do the following:
- obtain any releases of information to permit reports of previous professional evaluations to be sought,
- contact the child’s treating physician for further information on health status and medication treatment if any,
- obtain the results of the most recent evaluation from the child’s school or have the parent initiate one immediately if school performance concerns are part of the referral complaints,
- mail out the packet of parent and teacher behavior rating forms to be completed and returned before the initial appointment, being sure to include the written release of information permission form with the school forms, and
- obtain any information from social service agencies that may be involved in providing services to this child.
Information Obtained in Advance of the Interview
Clinicians may want to send out a packet of questionnaires to parents and teachers following the parents’ call to their clinic but in advance of the scheduled appointment. In fact, the parents of children referred to our clinic are not given an appointment date until these packets of information are completed and returned to the clinic. This system ensures that the packets are completed reasonably promptly and that the information is available for review by the clinician prior to meeting with the family, making the evaluation process far more efficient in its collection of important information. In these days of increasing cost-consciousness concerning mental health evaluations, particularly in managed care environments, efficiency of the evaluation is paramount, and time spent directly with the family is often limited and at a premium. In addition to a form cover-letter from the professional asking the parents to complete and return the entire packet of information, the packet also contains the General Instruction Sheet, a Child and Family Information Form, and a Developmental and Medical History Form. This packet also includes a reasonably comprehensive child behavior rating scale that covers the major dimensions of child psychopathology, such as the Child Behavior Checklist (CBCL) or the Behavior Assessment System for Children (BASC-3). Also in this packet should be a copy of a rating scale that specifically assesses ADHD symptoms. Such a form can also be found in the clinical manual by DuPaul and colleagues (2014; see References).
If desired, a more comprehensive rating of executive function deficits, nearly always associated with ADHD, can be obtained using either the Barkley Deficits in Executive Functioning Scale – Children and Adolescents, or the Behavior Rating Inventory of Executive Functioning. Clinicians who wish to assess adaptive behavior via the use of a questionnaire might consider including the Normative Adaptive Behavior Checklist in this packet or have parents complete this form on the day of the evaluation. Impairment in major domains of life activities is a required criterion for all Axis I psychiatric disorders in the DSM-5-TR. Some information on impairment can be gleaned from the face pages of the CBCL or BASC-3. More recently, a normed rating scale of impairment has been created that can be included with this packet for obtaining information on 15 different domains of life activities in children (Barkley Functional Impairment Scale – Children and Adolescents). Such information is of clinical interest not only for indications of pervasiveness and severity of behavior problems, but also for focusing discussions around these situations during the evaluation and subsequent parent-training program. These rating scales are discussed later.
It is useful to collect and review previous records before the interview. They might include any one or combination of the following: report cards, standardized testing results, medical records (including neurology, audiology, optometry, speech, and occupational therapy), individual educational plans, psychoeducational testing, psychological testing, and psychotherapy summaries.
A similar packet of information is sent to the teachers of this child, with prior parental written permission, of course. This packet does not contain the Medical and Developmental History Form or any adaptive behavior survey that may have been included for parents. This packet could contain the teacher version of the CBCL or BASC, and the same rating scale for assessing ADHD symptoms noted above. The Social Skills Rating System might also be included if the clinician desires information about the child’s social problems in school as well as his or her academic competence. The clinician can quickly see, for example, if the teacher feels the child is functioning at grade level in various subject areas, how the child has performed on group-administered achievement or aptitude tests, or subjective impressions of the child’s general mood and behavioral functioning. If possible, it is quite useful to contact the child’s teachers for a brief telephone interview prior to meeting with the family. Otherwise, a meeting can take place following the family’s appointment.
Once the parent and teacher packets are returned, the family should be contacted by telephone and given their appointment date. It is our custom also to send out a letter confirming this appointment date with directions for driving to the clinic.
On the day of the appointment, the following is to be done: (1) parental and child interview, (2) completion of self-report rating scales by the parents, and (3) any psychological testing that may be indicated by the nature of the referral (intelligence and achievement testing, etc.).
Parent Interview
The parent interview, although often criticized for its unreliability and subjectivity, is an indispensable part of the evaluation of children and adolescents presenting with concerns about ADHD. No adult is likely to have more wealth of knowledge about, history of interactions with, or sheer time spent with a child than the parents.
Whether wholly accurate or not, parent reports provide the most ecologically valid and important source of information concerning the child’s difficulties. It is the parents’ complaints that often lead to the referral of the child, will affect the parents’ perceptions of and reactions to the child, and will influence the parents’ adherence to the treatment recommendations to be made. Moreover, the reliability and accuracy of the parental interview have much to do with the manner in which it is conducted and the specificity of the questions offered by the examiner. An interview that uses highly specific questions about symptoms of psychopathology that have been empirically demonstrated to have a high degree of association with particular disorders greatly enhances diagnostic reliability.
The interview, particularly a semi-structured interview, allows the clinician in a sense to become another instrument in the assessment process. While scorable data are obtained, the small details and nuances of parent and child reporting resonates with clinician-acquired knowledge (from previous interviews, research, readings, workshops, etc.) in such a way as to flesh out and support final diagnostic conclusions. In other words, the interview provides the phenomenological data that rating scales cannot capture. The interview must also, however, focus on the specific complaints about the child’s psychological adjustment and any functional parameters (eliciting events and their consequences) associated with those problems if psychosocial and educational treatment planning is to be based on the evaluation.
Purposes
The parental interview often serves several purposes:
- It establishes a necessary rapport among the parents, the child, and the examiner that will prove invaluable in enlisting parental cooperation with later aspects of assessment and treatment.
- The interview is an obvious source of highly descriptive information about the child and family, revealing the parents’ particular views of the child’s apparent problems and narrowing the focus of later stages and components of the evaluation.
- It can readily reveal the degree of distress the child’s problems are presenting to the family, especially the parent being interviewed, as well as the overall psychological integrity of the parent. Hypotheses as to the presence of parental personality or psychiatric problems (depression, hostility, marital discord, etc.) may be revealed that will require further evaluation in subsequent components of the evaluation and consideration in formulating treatment recommendations.
- Examiners must be cautious not to over-interpret any informal observations of the child’s behavior during this clinic visit. The office behavior of ADHD children is often far better than that observed at home. Such observations merely raise hypotheses about potential parent-child interaction problems that can be explored in more detail with parents toward the end of this interview as well as during later direct behavioral observations of parent and child during play and task performance together. At this point in the interview, the examiner should inquire how representative the child’s immediate behavior is compared to that seen at home when the parent speaks with other adults in the child’s presence.
- I do not typically have the child in the same room when I conduct the parental interview. Other clinicians, however, may choose to do so. The presence of the child during the parental interview, however, raises thorny issues for the evaluation to which the examiner must be sensitive. Some parents are less forthcoming about their concerns and the details of the child’s specific problems when the child is present, not wishing to sensitize or embarrass the child unnecessarily or to create another reason for arguments at home about the nature of the child’s problems. Others are heedless of the potential problems posed for their child by this procedure, making it even more imperative that the examiner reviews these issues with them before beginning the evaluation. Still other parents may use the child’s presence to further publicly humiliate the child about his or her deficiencies or the distress the child has created for the family by behaving the way he or she does. Suffice it to say here that before starting the interview, the examiner must discuss and review with each unique family whether the advantages of having the child present are outweighed by these potential negative effects.
- The initial parent interview can help to focus the parent’s perceptions of the child’s problems on more important and more specific controlling events within the family. Parents often tend to emphasize historical or developmental causes of a global nature in discussing their children’s problems, such as what they did or failed to do with the child earlier in development that has led to this problem (i.e., placing the child in infant daycare, an earlier divorce, the child’s diet in earlier years, etc.). The interactional interview discussed later can serve to shift the parents’ attention to more immediate antecedents and consequences surrounding child behaviors, thereby preparing the parents for the initial stages of parent training in child management skills.
- The interview is designed to formulate a diagnosis and to develop treatment recommendations. Although diagnosis is not always considered necessary for treatment planning (a statement of the child’s developmental and behavioral deficits is often adequate), the diagnosis of ADHD, however, does provide some utility in terms of predicting a developmental course and prognosis for the child, determining eligibility for some special educational placements, and predicting potential response to a trial on stimulant medication. Many child behavior problems are believed to remit over short periods in as many as 75% of the cases. However, ADHD is a relatively chronic condition warranting much more cautious conclusions about eventual prognosis, and preparation of the family for coping with these later problems.
- A parental interview may serve as sheer catharsis, especially if this is the first professional evaluation of the child or when previous evaluations have proven highly conflicting in their results and recommendations. Ample time should be permitted to allow parents to ventilate this distress, hostility, or frustration. It may be helpful to note at this point that many parents of ADHD children have reported similarly distressing, confusing, or outright hostile previous encounters with professionals and educators about their child, as well as with well-intentioned but overly enmeshed or misinformed relatives. Compassion and empathy for the plight of the parents at this point can often result in a substantial degree of rapport with and gratitude toward the examiner and a greater motivation to follow subsequent treatment recommendations. At the very least, parents are likely to feel that they have finally found someone who truly understands the nature of their child’s problems and the distress they have experienced in trying to assist the child and has recommendations to do something about them.
The suggestions that follow for interviewing parents of ADHD children are not intended as rigid guidelines, only as areas that clinicians should consider. Each interview clearly differs according to individual child and family circumstances. Generally, those areas of importance to an evaluation include demographic information, child-related information, school-related information, and details about the parents, other family members, and community resources that may be available to the family.
Demographic Information
If not obtained in advance, routine demographic data concerning the child and family (e.g., ages of child and family members; child’s date of birth; parents’ names, addresses, employers, and occupations; and the child’s school, teachers, and physician) should be obtained at the outset of the appointment. I also use this initial introductory period to review with the family any legal constraints on the confidentiality of information obtained during the interview, such as the clinician’s legal duty (as required by state law) to report to state authorities any instances of suspected child abuse, threats the child (or parents) may make to cause physical harm to other specific individuals (the duty to inform), and threats the child (or parents) may make to harm themselves (e.g., suicide threats).
Major Parental Concerns
The interview then proceeds to the major referral concerns of the parents, and of the professional referring the child when appropriate. General descriptions of concerns by parents must be followed with specific questions by the examiner to elucidate the details of the problems and any apparent precipitants. Such an interview probes for the specific nature, frequency, age of onset, and chronicity of the problematic behaviors. Although some children with ADHD are reported to have been difficult in their temperament since birth or early infancy, the majority appear to be identifiable as deviant from normal by their caregivers between three and four years of age. However, it may be several years later before such children are brought to the attention of professionals. Although the diagnosis of ADHD among preschoolers may be more difficult due to higher rates of disruptive behavior among the normal population at this age, a few recent studies suggest that reliable and valid diagnosis can be made for children as young as three years, seven months old. The parent interview can also obtain information, as needed, on the situational and temporal variation in the behaviors and their consequences. If the problems are chronic, which they often are, determining what prompted the referral at this time reveals much about parental perceptions of the children’s problems, current family circumstances related to the problems’ severity, and parental motivation for treatment.
Review of Major Developmental Domains
Following this part of the interview, the examiner should review with the parents any potential problems that might exist in the developmental domains of motor, language, intellectual, academic, emotional, and social functioning. Such information greatly aids in the differential diagnosis of the child’s problems. Achieving this differential diagnosis requires the examiner to have an adequate knowledge of the diagnostic features of other childhood disorders, some of which may present as ADHD. For instance, many children with Autistic Spectrum Disorders or early Bipolar Disorder may be viewed by their parents as ADHD, as the parents are more likely to have heard about the latter disorder than the former ones and will recognize some of those qualities in their children. Questioning about inappropriate thinking, affect, social relations, and motor peculiarities may reveal a more seriously and pervasively disturbed child. If such symptoms seem to be present, the clinician might consider employing the Child Bipolar Parent Questionnaire (Papolos, Hennen, Cockerham, Thode Jr., & Youngstrom, 2006) to obtain a more thorough review of these symptoms. Inquiry also must be made as to the presence or history of tics or Tourette’s Disorder in the child or the immediate biological family members. When noted, these disorders would result in a recommendation for the more cautious use of stimulant drugs in the treatment of ADHD or, perhaps, lower doses of such medicine than typical to preclude the exacerbation of the child’s tic disorder.
School, Family, and Treatment
Histories
The examiner should also obtain information on the school and family histories. The family history must include a discussion of potential psychiatric difficulties in the parents and siblings, marital difficulties, and any family problems centered on chronic medical conditions, employment problems, or other potential stress events within the family. Of course, the examiner will want to obtain some information about prior treatments received by the child and his or her family for these presenting problems. When the history suggests potentially treatable medical or neurological conditions (allergies, seizures, Tourette’s Disorder, etc.), a referral to a physician is essential. Without evidence of such problems, however, referral to a physician for examination usually fails to reveal any further useful treatment information. But when the use of psychiatric medications is contemplated, a referral to a physician is clearly indicated.
Information about the child’s family is essential for two reasons. First, while ADHD is not caused by family stress or dysfunction, such adverse family factors can contribute to oppositional behavior or frank ODD. Therefore, the family history can help to clarify whether the child’s attentional or behavioral problems are developmental or rather a reaction to or product of stressful events that have taken place. Second, a history of certain psychiatric disorders in the extended family might influence diagnostic impressions or treatment recommendations. For example, because ADHD is hereditary, a strong family history of ADHD in biological relatives lends weight to the ADHD diagnosis, especially when other diagnostic factors are questionable. A family history of Bipolar Disorder in a child with severe behavioral problems might suggest that the child may be at higher risk for the disorder (an eight-fold increase in risk) and particular medication choices that otherwise might not be considered.
The interviewer can organize this section of the parental interview by first asking about the child’s siblings (whether there is anything significant about sibling relationships, whether siblings have any health or developmental problems). Then, questions about the parents may include how long they have been married, the overall stability of their marriage, whether each parent is in good physical health, whether either parent has ever been given a psychiatric diagnosis, and whether either parent has had a learning disability. The clinician should always be cautious of inquiring too much into the parents’ personal concerns. The purpose is to rule out family stress as a cause for the child’s difficulties and to determine what treatment recommendations may be appropriate.
In asking about extended family history, the interviewer should include maternal and paternal relatives.
Although it may seem tedious, it is extremely useful to go through the child’s school history year by year, starting with preschool. The examiner should ask parents open-ended questions: “What did his teachers have to say about him?”, “How did he do academically?”, or “How did he get along socially?” The examiner should avoid pointed, leading questions (e.g., “Did the teacher think he had ADHD?”). Examiners should allow parents to tell them their child’s story and listen for the red flags (e.g., the teacher thought he was immature, he had trouble with work completion, his organizational skills were terrible, he could not keep his hands to himself, or he would not do homework).
Gathering a reliable school history gives the clinician two crucial pieces of the diagnostic puzzle. First, is there evidence of symptoms or characteristics of ADHD in school previous to adolescence? Second, is there evidence of impairment in the child’s academic functioning as a result of these characteristics?
Examiners should ask parents what strategies teachers may have attempted to help the child in class. They should also inquire about tutoring services, school counselors, study skills classes, or peer helpers. The examiner should find out when and why teachers referred the child for psychoeducational testing. If the child is not doing well in school, the examiner should ask whether school personnel have ever offered an explanation. As always, the examiner should listen for clues about possible problems with behavioral regulation, impulse control, or sustained attention. If the child has a diagnosed learning disability, are there problems in school that cannot be explained by that learning disability?
Review
of Childhood Psychiatric Disorders
As part of the general interview of the parent, the examiner must cover the symptoms of the major child psychiatric disorders likely to be seen in ADHD children. A review of the major childhood disorders in the DSM-5-TR in some semi-structured or structured way is imperative if any semblance of a reliable and differential approach to diagnosis and the documentation of comorbid disorders is to occur. The examiner must exercise care in the evaluation of minority children to avoid over-diagnosing psychiatric disorders simply by virtue of ignoring differing cultural standards for child behavior. Should the parent indicate that a symptom is present, one means of precluding over-identification of psychopathology in minority children is to ask the following question: “Do you consider this to be a problem for your child compared to other children of your same ethnicity?” Only if the parent answers “yes” is the symptom to be considered present for purposes of psychiatric diagnosis.
Before proceeding, an explanation is in order as to why ODD and CD are queried first. Many parents arrive at the diagnostic evaluation overwhelmed by emotional stress, frustrations with home behaviors, or endless criticisms about the child from the school; thus they may be inclined to say yes to anything. Starting with ODD and CD questions allows these parents to get some of this frustration out of their system. Thus, when they are asked questions about ADHD, the answers are potentially more reliable and accurate.
In addition, unfortunately some parents actually “shop” for the ADHD diagnosis. They may have an agenda that involves obtaining a diagnosis for their child that is not entirely objective. Beginning the clinical interview with the reason for referral and then the ODD questions may assist the clinician in gaining important clinical impressions about the parents’ agenda. This is also why it can be extremely useful for clinicians to completely eliminate the word “attention” from their vocabulary during the interview. When the clinician asks specific questions about ADHD symptoms, the questions should be phrased in such a way that they are concrete and descriptive.
As noted above, adjustments have been made to the DSM-IV criteria for ADHD that now appear in the DSM-5-TR:
- The cutoff scores on both symptom lists (six of nine) were primarily based on children ages four to 16 in the DSM-IV field trial, making the extrapolation of these thresholds to age ranges outside those in the field trial of uncertain validity. For instance, no adults were involved in that field trial. Additional research on adults with ADHD has shown that a threshold of four or five symptoms would be better for detecting the adult stage of this disorder. So DSM-5-TR recommends a threshold of five on either symptom list for adults. Also, ADHD behaviors tend to decline in frequency within the child population over development, again suggesting that a somewhat higher threshold may be needed for preschool children (ages two to four years old) than is now recommended in DSM-5-TR.
- The specific age of onset of seven years old is not particularly critical for identifying ADHD children. Thus, DSM-5-TR has stipulated that an onset of symptoms occurring before age 12 in childhood is sufficient for purposes of clinical diagnosis.
- The criterion that the duration of symptoms be at least six months was not specifically studied in the field trial and was held over from earlier DSMs, primarily out of tradition. Some research on preschool children suggests that a large number of two- to three-year-olds may manifest the symptoms of ADHD as part of that developmental period and that they may remain present for periods of three to six months or longer. Children whose symptoms persisted for at least one year or more, however, were likely to remain deviant in their behavior pattern into the elementary school years. Although the DSM-5-TR did not change this requirement, adjusting the duration criterion to 12 months for ADHD, especially when evaluating preschool children, would seem to make good clinical sense.
- The criterion that symptoms must be evident in at least two of three settings (home, school, work) has been misinterpreted by clinicians to mean that children have sufficient symptoms of ADHD by both parent and teacher report before they can qualify for the diagnosis. This requirement bumps up against a methodological problem inherent in comparing parent and teacher reports. On average, the relationship of behavior ratings from these two sources tends to be fairly modest, averaging about 0.30. However, if parent and teacher ratings are unlikely to agree across the various behavioral domains being rated, the number of children qualifying for the diagnosis of ADHD is unnecessarily limited, due mainly to measurement artifact. Fortunately, some evidence demonstrates that children who meet DSM criteria by parent reports have a high probability of meeting the criteria by teacher reports. Even so, stipulating that parents and teachers must agree on the diagnostic criteria before a diagnosis can be rendered is probably unwise and unnecessarily restrictive. Clinicians are advised to seek evidence that some symptoms of the disorder existed at some time in the past or present of the child in several settings rather than insisting on the agreement of the parents with a current teacher. Moreover, clinicians should count the number of different symptoms reported by one source (e.g., parent) and then add to it any additional symptoms endorsed by the other (e.g. teacher) not reported by the first source. In sum, the number of symptoms used to make a diagnosis of ADHD is the number of different symptoms reported across all sources of information.
The foregoing issues should be kept in mind when applying the DSM criteria to particular clinical cases. It helps to appreciate the fact that the DSM represents guidelines for diagnosis, not rules of law or dogmatic prescriptions. Some clinical judgment is always going to be needed in the application of such guidelines to individual cases in clinical practice.
To assist clinicians with the differential diagnosis of ADHD from other childhood mental disorders, I compiled a list of differential diagnostic tips (see Table 1, below). Under each disorder, I list those features that would distinguish this disorder, in its pure form, from ADHD. However, many ADHD children may have one or more of these disorders as comorbid conditions with their ADHD; thus the issue here is not which single or primary disorder the child has but what other disorders besides ADHD are present and how they affect treatment planning.
Table 1. Differential Diagnostic Tips
for Distinguishing Other Mental Disorders from ADHD |
Oppositional Defiant Disorder and Conduct Disorder
- Lacks impulsive, disinhibited behavior
- Defiance primarily directed toward mother initially
- Able to cooperate and complete tasks requested by others
- Lacks poor sustained attention and marked restlessness
- Resists initiating demands, whereas ADHD children may initiate but cannot stay on task
- Often associated with parental child management deficits or family dysfunction
- Lacks neuromaturational delays in motor abilities
Learning Disabilities
- Has a significant IQ/achievement discrepancy (+1 standard deviation)
- Places below the 7th percentile in an academic achievement skill
- Lacks an early childhood history of hyperactivity
- Attention problems arise in middle childhood and appear to be task or subject specific
- Not socially aggressive or disruptive
- Not impulsive or disinhibited
Anxiety/Affective Disorders
- Likely to have a focused not sustained attention deficit
- Not impulsive or aggressive; often overinhibited
- Has a strong family history of anxiety disorders
- Restlessness is more like fretful, worrisome behavior, not the “driven,” inquisitive, or overstimulated type
- Lacks preschool history of hyperactive, impulsive behavior
- Not socially disruptive; typically socially reticent
Autism Spectrum Disorder
- Demonstrates significant impairment in social relationships with others manifested by lack of interest in such interactions, lack of eye contact, lack of responsiveness to their name, preference for attending to and interacting with physical features of the environment, and other symptoms of impaired sociability
- Demonstrates impaired language development such that language may not develop, develops late, and may include bizarre use of language and syntax
- May show unusual patterns of stereotyped motor actions and speech that include repetitive gestures, odd posturing and motions, and peculiar facial expressions
Schizotypal Personality Disorder
- Shows oddities/atypical patterns of thinking not seen in ADHD
- Peculiar sensory reactions
- Odd fascinations and strange aversions
- Socially aloof, schizoid, disinterested
- Lacks concern for personal hygiene/dress in adolescence
- Atypical motor mannerisms, stereotypies, and postures
- Labile, capricious, unpredictable moods not tied to reality
- Poor empathy, cause-effect perception
- Poor perception of meaningfulness of events
Juvenile-Onset Mania or Bipolar I Disorder
- Characterized by severe and persistent irritability
- Depressed mood exists more days than not
- Irritable/depressed mood typically punctuated by rage outbursts
- Mood swings often unpredictable or related to minimal events
- Severe temper outbursts and aggression with minimal provocation (thus, ODD is often present and severe)
- Later onset of symptoms than ADHD (but comorbid with early ADHD is commonplace)
- Press of speech and flight of ideas often present
- Psychotic-like symptoms often present during manic episodes
- Family history of Bipolar I Disorder more common
- Expansive mood, grandiosity of ideas, inflated self-esteem, hypersexuality often seen in adults with Bipolar Disorder are sometimes present though not as well formed; children may have the dysphoric type of disorder, however
- Requires that sufficient symptoms of Bipolar Disorder be present after excluding distractibility and hyperactivity (motor agitation) from Bipolar symptom list in DSM-5-TR before granting Bipolar I diagnosis to a child with symptoms of ADHD
- Suicidal ideation is more common than average in child (and suicide attempts more common in family history)
|
For years, some clinicians eschewed diagnosing children, viewing it as a mechanistic and dehumanizing practice that merely results in unnecessary labeling. Moreover, they felt that it got in the way of appreciating the clinical uniqueness of each case, unnecessarily homogenizing the heterogeneity of clinical cases. Some believed that labeling a child’s condition with a diagnosis is unnecessary as it is far more important to articulate the child’s pattern of behavioral and developmental excesses and deficits in planning behavioral treatments. Although there may have been some justification for these views in the past, particularly prior to the development of more empirically based diagnostic criteria, this is no longer the case in view of the wealth of research that went into creating the DSM-5-TR childhood disorders and their criteria. This is not to say that clinicians should not document patterns of behavioral deficits and excesses, as such documentation is important for treatment planning; only that this documentation should not be used as an excuse not to diagnose at all.
Furthermore, given that the protection of civil rights and entitlements such as access to educational and other services may actually hinge on awarding or withholding the diagnosis of ADHD, dispensing with diagnosis altogether could well be considered professional negligence. Moreover, billing insurance companies or government agencies for professional services requires the specification of a DSM diagnosis. For these reasons and others, clinicians, along with the parent of each child referred to them, must review in some systematic way the symptom lists and other diagnostic criteria for various childhood mental disorders.
The parental interview may also reveal that one parent, usually the mother, has more difficulty managing the ADHD child than does the other. Care should be taken to discuss differences in the parents’ approaches to management and any marital problems these differences may have spawned. Such difficulties in child management can often lead to reduced leisure and recreational time for the parents and increased conflict within the marriage and often within the extended family should relatives live nearby. It is often helpful to inquire as to what the parents attribute the causes or origins of their child’s behavioral difficulties, because such exploration may unveil areas of ignorance or misinformation that will require attention during the initial counseling of the family about the child’s disorder(s) and their likely causes. The examiner also should briefly inquire about the nature of parental and family social activities to determine how isolated, or insular, the parents are from the usual social support networks in which many parents are involved. Research shows that the degree of maternal social insularity is significantly associated with failure in subsequent parent training programs. When present to a significant degree, such a finding might support addressing the isolation as an initial goal of treatment rather than progressing directly to child behavior management training with that family.
Psychosocial Functioning
The first topic in this portion of the interview involves peer relationships and recreational activities. A clinical diagnosis of ADHD requires impairment in the child’s functioning in at least two important areas. This area could certainly be one of them. In addition, evidence of impaired peer relationships may lead to important treatment recommendations such as participation in a peer social skills training group or a peer support group.
Parents are asked if the child has trouble making or keeping friends, how the child behaves around other children, and how well the child fits in at school. Parents are also asked if they have concerns about the friends with whom their child spends time (e.g., do parents view them as “troublemakers”). Finally, they are asked about recreational activities in which the child participates outside school and any problems that occurred during those activities.
Compliance with parental requests and parental use of compensatory or motivational strategies also can be explored, especially if the clinician anticipates conducting parent training in child management skills with this family. These questions also substantiate evidence of impairment in family functioning as well as possible treatment recommendations for parent management training. If the interview on parent-child interactions discussed later is not to be used, parents are asked to describe how quickly their child complies with parental requests, if there are discrepancies in the child’s behavior with mother and father, and if parents generally agree on how to manage their child. They are also asked to describe the types of disciplinary strategies they use and whether or not they have tried incentive systems to encourage more appropriate behavior.
At a later appointment, perhaps even during the initial session of parent training, the examiner may wish to pursue more details about the nature of the parent-child interactions surrounding the following of rules by the child. If so, parents should be questioned about the child’s ability to accomplish commands and requests in a satisfactory manner in various settings, to adhere to rules of conduct governing behavior in various situations, and to demonstrate self-control (rule-following) appropriate to the child’s age in the absence of adult supervision. When problems are said to occur, the examiner follows up with the list of questions in Table 2, below. I have found it useful to follow the format set forth in Table 2 in which parents are questioned about their interactions with their children in a variety of home and public situations. When time constraints are problematic, the Home Situations Questionnaire HSQ rating scale (from my book, Defiant Children, 2013) can be used to provide similar types of information. After parents complete the scale, they can be questioned about one or two of the problem situations using the same follow-up questions as in Table 2, below. The HSQ scale is discussed later.
Table 2. Parental Interview Format for Assessing
Child Behavior Problems at Home and in Public |
Situation to be discussed |
If a problem, follow-up questions to ask |
Overall parent-child interactions
Playing alone
Playing with other children
Mealtimes
Getting dressed/undressed
Washing and bathing
When parent is on telephone
Child is watching television
When visitors are in your home
When you are visiting someone else’s home
In public places (stores, restaurants, church, etc.)
When father is in the home
When child is asked to do chores
When child is asked to do school homework
At bedtime
When child is riding in the car
When child is left with a baby-sitter
Any other problem situations |
1. Is this a problem area? If so, then proceed with questions 2-9.
2. What does the child do in this situation that bothers you?
3. What is your response likely to be?
4. What will the child do in response to you?
5. If the problem continues, what will you do next?
6. What is usually the outcome of this situation?
7. How often do these problems occur in this situation?
8. How do you feel about these problems?
9. On a scale of 1 (no problem) to 9 (severe), how severe is this problem
for you? |
Such an approach yields a wealth of information on the nature of parent-child interactions across settings, the type of noncompliance shown by the child (stalling, starting the task but failing to finish it, outright opposition and defiance, etc.), the particular management style employed by parents to deal with noncompliance, and the particular types of coercive behaviors used by the child as part of the noncompliance.
The parental interview can then conclude with a discussion of the child’s positive characteristics and attributes as well as potential rewards and reinforcers desired by the child that will prove useful in later parent training on contingency management methods. Some parents of ADHD children have had such chronic and pervasive management problems that upon initial questioning they may find it hard to report anything positive about their child. Getting them to begin thinking of such attributes is actually an initial step toward treatment as the early phases of parent training will teach parents to focus on and attend to desirable child behaviors.
Child Interview
Some time should always be spent directly interacting with the referred child. The length of this interview depends on the age, intellectual level, and language abilities of the child. For preschool children, the interview may serve merely as a time to become acquainted with the child, noting his or her appearance, behavior, developmental characteristics, and general demeanor. For older children and adolescents, this time can be fruitfully spent inquiring about the child’s views of the reasons for the referral and evaluation, how they see the family functioning, any additional problems they feel they may have, how well they are performing at school, their degree of acceptance by peers and classmates, and what changes in the family they believe might make life at home happier for them. As with the parents, the children can be queried as to potential rewards and reinforcers they find desirable which will prove useful in later contingency management programs.
Children below the age of nine to 12 are not especially reliable in their reports of their own disruptive behavior. The problem is compounded by the frequently diminished self-awareness and impulse control typical of defiant children with ADHD. Such ODD/ADHD children often show little reflection about the examiner’s questions and may lie or distort information in a more socially pleasing direction. Some will report that they have many friends, have no interaction problems at home with their parents, and are doing well at school, in direct contrast with the extensive parental and teacher complaints of inappropriate behavior by these children. Because of this tendency of ADHD children to underreport the seriousness of their behavior, particularly in the realm of disruptive or externalizing behaviors, the diagnosis of ODD or ADHD is never based on the reports of the child. Nevertheless, children’s reports of their internalizing symptoms, such as anxiety and depression, may be more reliable and thus should play some role in the diagnosis of comorbid anxiety or mood disorders in children with ADHD.
Although notation of children’s behavior, compliance, attention span, activity level, and impulse control in the clinic is useful, clinicians must guard against drawing any diagnostic conclusions when the children are not problematic in the clinic or office. Many ODD and ADHD children do not misbehave in the clinician’s office; thus reliance on such observations would clearly lead to false negatives in the diagnosis. In some instances, the behavior of the children with their parents in the waiting area prior to the appointment may be a better indication of management problems at home than is the children’s behavior toward the clinician, particularly when the interaction between child and examiner is one to one.
This is not to say that the office behavior of a child is entirely meaningless. When it is grossly inappropriate or extreme, it may well signal the likelihood of problems in the child’s natural settings, particularly school. It is the presence of relatively normal conduct by the child that may be an unreliable indicator of the child’s normalcy elsewhere. For instance, in a study of 205 four- to six-year-old children, I examined the relationship of office behavior to parent and teacher ratings. Of these children, 158 were identified at kindergarten registration as being 1.5 standard deviations above the mean (93rd percentile) on parent ratings of ADHD and ODD (aggressive) symptoms. These children were subsequently evaluated for nearly four hours in a clinic setting, after which the examiner completed a rating scale of the children’s behavior in the clinic. I then classified the children as falling below or above the 93rd percentile on these clinic ratings using data from a normal control group. The children were also classified as falling above or below this threshold on parent ratings of home behavior and teacher ratings of school behavior using the CBCL. I have found that no significant relationship exists between the children’s clinic behavior (normal or abnormal) and the ratings by their parents. However, a significant relationship exists between abnormal ratings in the clinic and abnormal ratings by the teacher: 70% of the children classified as abnormal in their clinic behavior were also classified as such by the teacher ratings of class behavior, particularly on the externalizing behavior dimension. Normal behavior, however, was not necessarily predictive of normal behavior in either parent or teacher ratings. This finding suggests that abnormal or significantly disruptive behavior during a lengthy clinical evaluation may be a marker for similar behavioral difficulties in a school setting. Nevertheless, the wise clinician will contact the child’s teacher directly to learn about the child’s school adjustment rather than relying entirely on such inferences about school behavior from clinic office behavior. Since this study was completed, standard observation forms for recording child behavior during testing and in school settings have been developed and made commercially available: The Test Observation Form by McConaughy and Achenbach (2004).
Teacher Interview
At some point before or soon after the initial evaluation session with the family, contact with the child’s teachers may be helpful to further clarify the nature of the child’s problems. This contact will most likely occur by telephone unless the clinician works within the child’s school system. Interviews with teachers have all of the same merits as interviews with parents, providing a second ecologically valid source of indispensable information about the child’s psychological adjustment, in this case in the school setting. Like parent reports, teacher reports are also subject to bias, and the integrity of the informant, whether it be the parent or teacher, must always be weighed by judging the validity of the information itself.
Many ADHD children have problems with academic performance and classroom behavior and the details of these difficulties need to be obtained. Initially this information may be obtained by telephone; however, when time and resources permit, a visit to the classroom and direct observation and recording of the child’s behavior can prove quite useful if further documentation of ADHD behaviors is necessary for planning later contingency management programs for the classroom. Although this scenario is unlikely to prove feasible for clinicians working outside school systems, particularly in the climate of increasingly prevalent managed health care plans which severely restrict the evaluation time that will be compensated, for those professionals working within school systems, direct behavioral observations can prove very fruitful for diagnosis, and especially for treatment planning. As noted above, standardized behavioral observation forms have recently been published to permit recording such behavior: The Direct Observation Form also by McConaughy & Achenbach (2004).
Teachers should also be sent the rating scales mentioned earlier. They can be sent as a packet prior to the actual evaluation so that the results are available for discussion with the parents during the interview, as well as with the teacher during the subsequent telephone contact or school visit.
The teacher interview also should focus on the specific nature of the child’s problems in the school environment, again following a behavioral format. The settings, nature, frequency, consequences, and eliciting events for the major behavioral problems also can be explored. The follow-up questions used in the parental interview on parent-child interactions (shown in Table 2, above) may prove useful here as well. Given the greater likelihood of the occurrence of learning disabilities in this population, teachers should be questioned about such potential disorders. When evidence suggests their existence, the evaluation of the child should be expanded to explore the nature and degree of such deficits as viewed by the teacher. Even when learning disabilities do not exist, children who have ADHD are more likely to have problems with sloppy handwriting, careless approaches to tasks, poor organization of their work materials, and academic underachievement relative to their tested abilities. Time should be taken with the teachers to explore the possibility of these problems.
Clinical Tips
- Never base a diagnosis of ADHD on the reports of the child or teen. Children and teens with ADHD are not especially reliable in their reports of their own disruptive behavior. The problem is compounded by the frequently diminished self-awareness and impulse control typical of children with ADHD. Such children often show little reflection about the examiner’s questions and may even lie or distort information in a more socially pleasing direction. In contrast, children’s reports of their internalizing symptoms, such as anxiety and depression, may be more reliable and so should play some role in the diagnosis of those disorders.
- Do not rely heavily on how well the child behaves during the interview. It has been known for more than 40 years that many children with ADHD do not misbehave in clinicians’ offices (see Sleator & Ullmann, 1981). Hence, a heavy reliance on such observations would clearly lead to false negatives in the diagnosis. In some instances, the behavior of the children with their parents in the waiting area prior to the appointment may be a better indication of the children’s management problems at home than is the children’s behavior toward the clinician in a one-to-one interaction.
- Do not use absence of attention and other behavioral problems at school but revealed during the psychological testing as evidence against the diagnosis, in view of the 1-to-1 format of such testing.
- Be aware that ADHD symptoms and their severity may fluctuate somewhat or even markedly across settings and time of day. They can also vary as a consequence of various factors in the situation, such as the schedule of consequences for behavior, novelty, adult supervision, and other factors. Below I show a summation of the results of research on such setting variation. Findings suggest that symptom severity may be generally better in the situations in the left column and typically worse in situations on the right. Therefore, it is wise to focus more time in the evaluation on exploring the settings in the right column where symptoms are more likely to be expressed or be more severe, on average.
Better Here |
Worse Here |
Fun |
Boring |
| Immediate |
Delayed Consequences |
| Frequent |
Infrequent Feedback |
| High |
Low Salience |
| Gaming Apps |
Homework from School |
| High (Smart Technology) |
Low Technology – chores, paperwork |
| Early |
Late in the Day |
| Supervised |
Unsupervised |
| One-to-one |
Group Situations |
| Novelty |
Familiarity |
| Fathers |
Mothers |
| Strangers |
Parents |
| Clinic Exam Room |
Waitng Room |
This pattern is not well explained by viewing ADHD as a disorder of inattention or its other official symptoms. But it is much better accounted for when we look at this pattern through the lens of EF-SR Theory. The situations on the right place a much greater demand on executive function and self-regulation, whereas those on the left much less so. Adopting that theory for understanding ADHD not only allows you to better understand and so assess the nature of ADHD across such situations, it permits you to better explain it to parents, teachers, and adult clients as well.
Rating Scales
Child Behavior Rating Scales for Parent and Teacher Reports
Child behavior checklists and rating scales have become an essential element in the evaluation and diagnosis of children with behavior problems. The availability of several scales with excellent reliable and valid normative data across a wide age range of children makes their incorporation into the assessment protocol quite convenient and extremely useful. Such information is invaluable in determining the statistical deviance of the children’s problem behaviors and the degree to which other problems may be present. As a result, it is useful to mail out a packet of these scales to parents prior to the initial appointment, asking that they be returned on or before the day of the evaluation, as described earlier. Thus the examiner can review and score the scales before interviewing the parents, allowing vague or significant answers to be elucidated in the subsequent interview and focusing the interview on those areas of abnormality highlighted in the responses to scale items.
Numerous child behavior rating scales exist. Despite their limitations, they offer a means of gathering information from informants who may have spent months or years with the child. Apart from interviews, there is no other means of obtaining such a wealth of information with so little investment of time. The fact that such scales provide a means to quantify the opinions of others, often along qualitative dimensions, and to compare these scores to norms collected on large groups of children, is further affirmation of the merits of these instruments. Nevertheless, behavior rating scales are opinions and are subject to the oversights, prejudices, and limitations on reliability and validity that such opinions may have.
Initially, it is advisable to utilize a “broad-band” rating scale that provides coverage of the major dimensions of child psychopathology known to exist, such as depression, anxiety, withdrawal, aggression, delinquent conduct, and, of course, inattentive and hyperactive-impulsive behavior. These scales should be completed by parents and teachers. Such scales would be the BASC-3 and the CBCL, both of which have versions for parents and teachers and satisfactory normative information.
Narrow-band scales that focus specifically on the assessment of symptoms of ADHD should also be employed in the initial screening of children. DuPaul and colleagues collected U.S. norms for another version of an ADHD rating scale, the ADHD-V Rating Scale (DuPaul et al., 2014). To assess the presence of another attention disorder known as SCT, and now CDS, consider using my Sluggish Cognitive Tempo Scale – Children and Adolescents (Barkley, 2018).
The clinician should also examine the pervasiveness of the child’s behavior problems within the home and school settings, as such measures of situational pervasiveness appear to have as much or more stability over time than do the aforementioned scales. The Home Situations Questionnaire (HSQ) (see my book, Defiant Children, 2013, or the new book, Treating ADHD in Children and Adolescents: What Every Clinician Needs to Know, 2022) provides a means for doing so, and normative information for these scales is available. The HSQ requires parents to rate their child’s behavioral problems across 16 different home and public situations. The School Situations Questionnaire (SSQ) similarly obtains teacher reports of problems in 12 different school situations (also in the books above).
As noted earlier, abundant research shows that ADHD is associated with substantial and pervasive deficits in executive functioning (EF) in daily life, even if those deficits are not always evident on neuropsychological tests used with either children or adults. It is therefore recommended that clinicians wishing to evaluate EF in children having ADHD use rating scales of EF in daily life that provide a better (more ecologically valid) means of doing so than do tests. One recent scale developed to do so is my own (Barkley, 2012a), but clinicians may find the earlier BRIEF (Gioia et al., 2000) to be useful for this purpose as well.
Clinicians should also formally evaluate impairment in major life activities in some standardized way. To that end, my new rating scale (Barkley Functional Impairment Scale – Children and Adolescents, 2012b) can help assess a child’s impairment in 15 major life activities relative to norms collected on a U.S. representative sample of children ages six to 18 years old.
The more specialized or narrow-band scales focusing on symptoms of ADHD as well as the HSQ and SSQ can be used to monitor treatment response when given prior to, throughout, and at the end of parent training. They can also be used to monitor the behavioral effects of medication on children with ADHD.
Self-Report Behavior Rating Scales for Children
Achenbach has developed a rating scale quite similar to the CBCL, which is completed by children ages 11 to 18 (Youth Self-Report Form). Most items are similar to those on the parent and teacher forms of the CBCL except that they are worded in the first person. A later revision of this scale (Cross-Informant Version; Achenbach, 2001) now permits direct comparisons of results among the parent, teacher, and youth self-report forms of this popular rating scale. Research suggests that although such self-reports of ADHD children and teens are more deviant than the self-reports of youth without ADHD, the self-reports of problems by the ADHD youth, whether by interview or the CBCL Self-Report Form, are often less severe than the reports provided by parents and teachers. The BASC-3, noted earlier, also has a self-report form that may serve much the same purpose as that for the CBCL.
The reports of children about internalizing symptoms, such as anxiety and depression, are more reliable and likely to be more valid than the reports of parents and teachers about these symptoms in their children. For this reason, the self-reports of defiant children and youth should still be collected, as they may have more pertinence to the diagnosis of comorbid internalizing disorders in children than to the defiant behavior itself.
Adaptive Behavior Scales and Inventories
Research shows that a major area of life functioning affected by ADHD is the realm of general adaptive behavior. Adaptive behavior often refers to the child’s development of skills and abilities that will assist them in becoming more independent, responsible, and self-caring individuals. This domain often includes:
- self-help skills, such as dressing, bathing, feeding, and toileting requirements, as well as telling and using time and understanding and using money;
- interpersonal skills, such as sharing, cooperation, and trust;
- motor skills, such as fine motor (zipping, buttoning, drawing, printing, use of scissors, etc.) and gross motor abilities (walking, hopping, negotiating stairs, bike riding, etc.);
- communication skills; and
- social responsibility, such as degree of freedom permitted within and outside the home, running errands, performing chores, and so on.
So substantial and prevalent is this area of impairment among children with ADHD that some researchers have even argued that a significant discrepancy between IQ and adaptive behavior scores (expressed as standard scores) may be a hallmark of ADHD.
Several instruments are available for the assessment of this domain of functioning. The Vineland Adaptive Behavior Inventory is probably the most commonly used measure for assessing adaptive functioning. It is an interview, however, and takes considerable time to administer. For other scales assessing adaptive behavior, see the review by Evans & Bradley-Johnson (2007). The CBCL and the BASC-3 completed by parents also contains several short scales that provide a cursory screening of several areas of adaptive functioning (Activities, Social, and School) in children, but are no substitute for the in-depth coverage provided by the Vineland or NABC scales.
Peer Relationship Measures
As noted earlier, children with ADHD often demonstrate significant difficulties in their interactions with peers, and such difficulties are associated with an increased likelihood of persistence of their disorder. A number of different methods for assessing peer relations have been employed in research with behavior-problem children, such as direct observation and recording of social interactions, peer and subject completed sociometric ratings, and parent and teacher rating scales of children’s social behavior. Most of these assessment methods have no norms and thus would not be appropriate for use in the clinical evaluation of children with ADHD. For clinical purposes, rating scales may offer the most convenient and cost-effective means for evaluating this important domain of childhood functioning. The CBCL and BASC-3 rating forms described earlier contain scales that evaluate children’s social behavior and norms are available for these scales, permitting their use in clinical settings. The more recently developed Barkley Functional Impairment Scale – Children and Adolescents also covers various domains of social life and has U.S. representative norms (Barkley, 2012) (see References). Three other scales that focus specifically on social skills are the Matson Evaluation of Social Skills with Youngsters (MESSY; Matson, Rotatori, & Helsel, 1983), the Taxonomy of Problem Social Situations for Children (TOPS; Dodge, McClaskey, & Fledman, 1985), and the Social Skills Rating System. The latter also has norms and a software scoring system, making it useful in clinical contexts. I have used it extensively in our research and clinical evaluations.
Parent Self-Report Measures
It has become increasingly apparent that child behavioral disorders, their level of severity, and their response to interventions are, in part, a function of factors affecting parents and the family at large. Several types of psychiatric disorders are likely to occur more often among family members of a child with ADHD than in matched groups of control children. Numerous studies over the past 30 years have demonstrated the further influence of these disorders on the frequency and severity of behavioral problems in ADHD children.
As discussed earlier, the extent of social isolation in mothers of behaviorally disturbed children influences the severity of the children’s behavioral disorders as well as the outcomes of parent training. Separate and interactive contributions of parental psychopathology and marital discord affect the decision to refer children for clinical assistance, the degree of conflict in parent-child interactions, and child antisocial behavior. The degree of parental resistance to training also depends on such factors. Assessing the psychological integrity of parents, therefore, is an essential part of the clinical evaluation of defiant children, the differential diagnosis of their prevailing disorders, and the planning of treatments stemming from such assessments. Thus, the evaluation of children for ADHD is often a family assessment rather than one of the child alone. Although space does not permit a thorough discussion of the clinical assessment of adults and their disorders here, this section provides a brief mention of some assessment methods clinicians may find useful as a preliminary screening for certain variables of import to treatment in ADHD children.
The parents can complete these instruments in the waiting room, during the time their child is being interviewed. (To save time, some professionals may prefer to send these self-report scales out to parents in advance of their appointment, at the same time they send the child-behavior questionnaires to the parents. If so, the clinician needs to prepare a cover letter sensitively explaining to parents the need for obtaining such information.) On the day of the interview, the clinician can indicate to parents that having a complete understanding of a child’s behavior problems requires learning more about both the children and their parents. This process includes gaining more information about the parents’ own psychological adjustment and how they view themselves as succeeding in their role as parents. The rating scales can then be introduced as one means of gaining such information. Few parents refuse to complete these scales after an introduction of this type.
Parental ADHD
Family studies of the aggregation of psychiatric disorders among the biological relatives of children with ADHD and ODD clearly demonstrate an increased prevalence of ADHD and ODD among the parents of these children. In general, there seems to be at least a 40%–50% chance that one of the two parents of the child with ADHD will also have adult ADHD (15%–20% of mothers and 25%–30% of fathers). The manner in which ADHD in a parent might influence the behavior of an ADHD child specifically and the family environment more generally has now been studied. It indicates that such parents are less attentive and responsive to their children, monitor their activities less often, and may be less rewarding of their children’s positive behavior. Adults with ADHD also have been shown to be more likely to have problems with anxiety, depression, personality disorders, alcohol use and abuse, and marital difficulties; to change their employment and residence more often; and to have less education and socioeconomic status than adults without ADHD, all of which can have an impact on the functioning of an ADHD child within such a family.
Greater diversity and severity of psychopathology among parents is particularly apparent among the subgroup of ADHD children with comorbid ODD or CD. More severe ADHD seems to also be associated with younger-age parents, suggesting that pregnancy during their own teenage or young adult years is more characteristic of parents of ADHD than non-ADHD children. It is not difficult to see that these factors, as well as the primary symptoms of ADHD, could influence the manner in which child behavior is managed within the family as well as the quality of home life for such children more generally. Some research in our clinic suggests that when the parent has ADHD, the probability that the child with ADHD will also have ODD increases markedly. Studies suggest that ADHD in a parent may interfere with the ability of that parent to benefit from a typical behavioral parent training program. Treatment of the parent’s ADHD (with medication) may result in greater success in subsequent retraining of the parent. These preliminary findings suggest the importance of determining the presence of ADHD in the parents of children undergoing evaluation for the disorder.
The DSM-5-TR symptom list for ADHD has been cast in the form of two behavior rating scales for use in screening adults for ADHD, one for current behavior and the other for recall of behavior during childhood (Barkley, 2011). Alternatively, Conners has a rating scale for adult ADHD at MultihealthSystems.com). Norms are available for a representative sample of the U.S. adult population and the scale has excellent psychometric properties. Again, clinically significant scores on these scales do not, by themselves, grant the diagnosis of ADHD to a parent, but they should raise suspicion in the clinician’s mind about such a possibility. If so, consideration should be given to referring the parent for further evaluation and, possibly, treatment of adult ADHD.
The use of such scales in screening parents of ADHD children would be a helpful first step in determining whether the parents have ADHD. If the child meets diagnostic criteria for ADHD and these screening scales for ADHD in the parents prove positive (clinically significant), referral of the parents for a more thorough evaluation and differential diagnosis might be in order. At the very least, positive findings from the screening would suggest the need to take them into account in treatment planning and parent training.
Marital Discord
Many instruments exist for evaluating marital discord. The one most often used in research on childhood disorders has been the Locke-Wallace Marital Adjustment Scale (Locke & Wallace, 1959). Marital discord, parental separation, and parental divorce are more common in parents of ADHD children. Parents with such marital difficulties may have children with more severe defiant and aggressive behavior and such parents may also be less successful in parent training programs. Screening parents for marital problems, therefore, provides important clinical information to therapists contemplating a parent training program for such parents. Clinicians are encouraged to incorporate a screening instrument for marital discord into their assessment battery for parents of children with defiant behavior.
Parental Depression and General Psychological Distress
Parents of ADHD children, especially those with comorbid ODD or CD, are frequently more depressed than parents of children without ADHD, which may affect their responsiveness to behavioral parent training programs. The Beck Depression Inventory is often used to provide a quick assessment of parental depression. Greater levels of psychopathology generally, and psychiatric disorders specifically, also have been found in parents of children with ADHD, many of whom also have ADHD. One means of assessing this area of parental difficulties is through the use of the Symptom Checklist 90 – Revised (or the shorter, 27-item version). This instrument not only has a scale assessing depression in adults, but also has scales measuring other dimensions of adult psychopathology and psychological distress. Whether clinicians use this or some other scale, the assessment of parental psychological distress generally, and psychiatric disorders particularly, makes sense in view of their likely impact on the child’s course and the implementation of the child’s treatments typically delivered via the parents.
Parental Stress
Research over the past 15 years suggests that parents of children with behavior problems, especially those children with comorbid ODD and ADHD, report more stress in their families and in their parental role than those of normal or clinic-referred non-ADHD children. One measure frequently used in such research to evaluate this construct has been the Parenting Stress Index (PSI). The original PSI is a 150-item multiple-choice questionnaire which can yield six scores pertaining to child behavioral characteristics (distractibility, mood, etc.), eight scores pertaining to maternal characteristics (e.g., depression, sense of competence as a parent, etc.), and two scores pertaining to situational and life stress events. These scores can be summed to yield three domain or summary scores: Child Domain, Mother Domain, and Total Stress. A shorter version of this scale is available, and clinicians are encouraged to utilize it in evaluating parents of defiant children.
The Role of Psychological Testing
Despite advances in our knowledge about psychological testing and the allure of numbers over perception, the search for accurate and reliable measures of ADHD symptoms has not yielded a litmus test. To date there are no psychological or neuropsychological tests sufficiently reliable and valid enough for use in the diagnosis of ADHD, either in children or adults. Ratings of ADHD and of executive functioning (EF) are far more useful in both documenting the developmental inappropriateness of these symptoms in children as well as in supporting the diagnosis of ADHD. The fact that there is no significant correlation between the neuropsychological tests of EF and ratings of EF in daily life shows the paucity of ecological validity of the EF tests and helps account for why ratings may be clinically useful while tests of EF are not clinically helpful to diagnosis.
The value of psychological testing may therefore be greatest for ruling in or out the presence of intellectual delay or learning disorders (LD) as associated conditions in cases of ADHD. In those instances, brief screening tests of IQ and academic achievement can be given. While only a small percentage of cases of ADHD have intellectual delay, slightly higher than the national average, up to half of them may have learning disabilities. Given this high prevalence of LD in ADHD, all cases of ADHD should receive screening on academic achievement tests.
Legal and Ethical Issues
Apart from the legal and ethical issues involved in the general practice of providing mental health services to children, several such issues may be somewhat more likely to occur in the evaluation of ADHD children. The first involves the issue of custody or guardianship of the child as it pertains to who can request the evaluation of the child for ADHD. Children with ODD, ADHD, or CD are more likely than average to come from families in which the parents have separated or divorced or in which significant marital discord may exist between the biological parents. As a result, the clinician must take care at the point of contact between the family and the clinic or professional to determine who has legal custody of the child and particularly the right to request mental health services on behalf of the minor. It must also be determined in cases of joint custody – an increasingly common status in divorce/custody situations – whether the nonresident parent has the right to dispute the referral for the evaluation, to consent to the evaluation, to attend on the day of appointment, and/or to have access to the final report. This right to review or dispute mental health services may also extend to the provision of treatment to the child. Failing to attend to these issues before the evaluation can lead to contentiousness, frustration, and even legal action among the parties to the evaluation that could have been avoided had greater care been taken to iron out these issues beforehand. Although these issues apply to all evaluations of children, they may be more likely to arise in families seeking assistance for ADHD children.
A second issue that also arises in all evaluations, but may be more likely in cases involving ADHD, is the duty of the clinician to disclose to state agencies any suspected physical or sexual abuse or neglect of the child. Clinicians should routinely forewarn parents of this duty to report when it applies in a particular state before starting the formal evaluation procedures. In view of the greater stress that ADHD or ODD children appear to pose for their parents, as well as the greater psychological distress their parents are likely to report, the risk for abuse of ADHD children, especially those with ODD, Bipolar disorder, or Disruptive Mood Dysregulation Disorder, may be higher than average. The greater likelihood of parental ADHD or other psychiatric disorders may further contribute to this risk, resulting in a greater likelihood that evaluations of children with disruptive behavior disorders will involve suspicions of abuse. Understanding such legal duties as they apply in a given state or region and taking care to exercise them properly, yet with sensitivity to the larger clinical issues, are the responsibility of any clinician involved in providing mental health services to children.
Over the past 20 years, ADHD children have been gaining access to government entitlements, sometimes thought of as legal rights, which makes it necessary for clinicians to be well informed about the legal issues if they are to properly and correctly advise the parents and school staff. For instance, children with ADHD in the United States are now entitled to formal special educational services under the Other Health Impaired Category of the Individuals with Disabilities in Education Act, provided of course that their ADHD is sufficiently serious to interfere significantly with school performance. In addition, such children also have legal protections and entitlements under Section 504 of the Disability Rights Act or the more recent Americans with Disabilities Act as it applies to the provision of an appropriate education for children with disabilities. And should ADHD children have a sufficiently severe disorder and reside in a family of low economic means, they may also be eligible for financial assistance under the Social Security Act. Space precludes a more complete explication of these legal entitlements here. Suffice it to say here that clinicians working with ADHD children need to familiarize themselves with these various rights and entitlements if they are to be effective advocates for the children they serve.
A final legal issue related to ADHD children is that of legal accountability for their actions in view of the argument made elsewhere that their ADHD is a developmental disorder of self-control. Should children with ADHD be held legally responsible for the damage they may cause to property, the injury they may inflict on others, or the crimes they may commit? In short, is ADHD an excuse to behave irresponsibly without being held accountable for the consequences? The answer is unclear and deserves the attention of sharper legal minds than ours. It is my opinion, however, that ADHD explains why certain impulsive acts may have been committed, but it does not sufficiently disturb mental faculties to the point of excusing legal accountability, as might occur, for example, under the insanity defense. Nor should ADHD be permitted to serve as an extenuating factor in the determination of guilt or the sentencing of an individual involved in criminal activities, particularly those involving violent crime. This opinion is predicated on the fact that the vast majority of children with ADHD, even those with comorbid ODD, do not become involved in violent crime, especially predatory crime, as they grow up. A substantial minority are prone to engage in reactive aggression when provoked, however. Moreover, studies attempting to predict criminal conduct within samples of ADHD children followed to adulthood either have not been able to find adequate predictors of such outcomes or have found them to be so weak as to account for a paltry amount of variance in such outcomes. Moreover, those variables that may make a significant contribution to the prediction of criminal or delinquent behavior more often involve measures of parental and family dysfunction as well as social disadvantage and much less so, if at all, measures of ADHD symptoms.
Until this matter receives greater legal scrutiny, it seems wise to view ADHD as one of several explanations for impulsive conduct, but not a direct, primary, or immediate cause of criminal conduct for which the individual should not be held accountable. Individuals with ADHD often know right from wrong as well as do most typical people of similar intellectual ability. Yet they may fail to give due contemplation to such moral matters when faced with a situation that provokes them to criminal action, especially one arising from their impulsive nature.
The Pediatric Medical Examination (with assistance from Mary McMurray, M.D. and Michelle Macias, MD)
It is essential that children being considered for a diagnosis of ADHD have a complete pediatric physical examination. However, traditionally such examinations are brief, relatively superficial, and as a result often unreliable and invalid for achieving a diagnosis of ADHD or identifying other comorbid behavioral, psychiatric, and educational conditions. This is often the result of ignoring the other two essential features of the evaluation of ADHD children: a thorough clinical interview, reviewed earlier, and the use of behavior-rating scales. To properly diagnose and treat these children and adolescents, it is imperative that adequate time be committed to the evaluation for completion of these components. If this is not possible, the physician is compelled to conduct the appropriate medical examination, but withhold the diagnosis until the other components can be accomplished by referral to a mental health professional.
The features of the pediatric examination and the issues that must be entertained therein are described next.
The Medical Interview
Most of the contents of an adequate medical interview are identical to those described previously for the parental interview. However, greater time will clearly be devoted to a more thorough review of the child’s genetic background, pre- and peri-natal events, and developmental and medical history, as well as the child’s current health, nutritional status, and gross sensory-motor development. The time to listen to the parents’ story and the child’s feelings and to explain the nature of the disorder is one of the most important things a physician can offer a family. In this way, the evaluation process itself can often be therapeutic.
One major purpose of the medical interview that distinguishes it from the psychological interview noted previously is its focus on differential diagnosis of ADHD from other medical conditions, particularly those that may be treatable. In rare cases, the ADHD may have arisen secondary to a clear biologically compromising event, such as recovery from severe Reye’s syndrome, surviving an hypoxic-anoxic event such as near-drowning or severe smoke inhalation, significant head trauma, or recovery from an central nervous system infection or cerebral-vascular disease. The physician should obtain details of these surrounding events as well as the child’s developmental, psychiatric, and educational status prior to the event, and any significant changes in these domains of adjustment since the event. The physician should also document ongoing treatments related to such events. In other cases, the ADHD may be associated with significant lead or other metal or toxic poisonings, which will require treatment in their own right.
It is also necessary to determine whether the child’s conduct or learning problems are related to the emergence of a seizure disorder or are secondary to the medication being used to treat the disorder. As many as 20% of epileptic children may have ADHD as a comorbid condition and up to 30% may develop ADHD or have it exacerbated by the use of phenobarbital or dilantin as anticonvulsants. In such cases, changing to a different anticonvulsant may greatly reduce or even ameliorate the attentional deficits and hyperactivity of such children.
A second purpose of the medical exam is to thoroughly evaluate any coexisting conditions that may require medical management. In this case, the child’s ADHD is not seen as arising from these other conditions, but as being comorbid with it. ADHD is often associated with higher risks not only for other psychiatric or learning disorders, but also for motor incoordination, enuresis, encopresis, allergies, otitis media, and greater somatic complaints in general. A pediatric evaluation is desirable or even required for many of these comorbid conditions. For instance, the eligibility of the child for physical or occupational therapy at school or in a rehabilitation center may require a physician’s assessment and written recommendation of the need for such. And, although most cases of enuresis and encopresis are not due to underlying physiological disorders, all cases of these elimination problems should be evaluated by a physician before beginning nutritional and behavioral interventions. Even though many of these cases are “functional” in origin, medications may be prescribed to aid in their treatment, as in the use of atomoxetine, oxybutynin, or imipramine for bedwetting. Certainly children with significant allergies or asthma require frequent medical consultation and management of these conditions, often by specialists who appreciate the behavioral side effects of medications commonly used to treat them. Theophyline, for example, is increasingly recognized as affecting children’s attention span and may exacerbate a preexisting case of ADHD. For these and other reasons, the role of the physician in the evaluation of ADHD should not be underestimated despite overwhelming evidence that by itself it is inadequate as the sole basis for a diagnosis of ADHD.
A third purpose of the medical examination is to determine whether physical conditions exist that are contraindications for treatment with medications. For instance, a history of high blood pressure or cardiac difficulties warrants careful consideration about a trial on a stimulant drug given the known presser effects of these drugs on the cardiovascular system. Some children may have a personal or family history of tic disorders or Tourette’s Disorder, which would dictate a somewhat more cautious approach in prescribing stimulants in view of their greater likelihood of bringing out such movement disorders or increasing the occurrence of those that already exist in about a third of such cases comorbid with ADHD. Note however, that the majority of cases having a tic disorder with ADHD can be prescribed such medications without exacerbating their tic disorder. Instead, the non-stimulants such as atomoxetine or guanfacine XR may be more appropriate if there is concern about tic exacerbation. These examples merely illustrate the myriad medical and developmental factors that need to be carefully assessed in considering whether a particular ADHD child is an appropriate candidate for drug treatment.
Physical Examination
In the course of the physical examination, height, weight, and head circumference require measurement and comparison to standardized graphs. Hearing and vision, as well as blood pressure, should be screened. Findings suggestive of hyper- or hypothyroidism, lead poisoning, anemia, or other chronic illness clearly need to be documented and further workup should be pursued. The formal neurological examination often includes testing of cranial nerves, gross and fine motor coordination, eye movements, finger sequencing, rapid alternating movements, impersistence, synkinesia, motor overflow, choreiform movements, and tandem gait tasks. The exam is often used to look for signs of previous central nervous system insult or of a progressive neurological condition, abnormalities of muscle tone, and a difference in strength, tone, or deep tendon reflex response between the two sides of the body. The existence of nystagmus, ataxia, tremor, decreased visual field, or fundal abnormalities should be determined and further investigation pursued when found. This evaluation should be followed by a careful neurodevelopmental exam covering the following areas: motor coordination, visual-perceptual skills, language skills, and cognitive functioning. Although these tests are certainly not intended to be comprehensive or even moderately in-depth evaluations of these functions, they are invaluable as quick screening methods for relatively gross deficiencies in these neuropsychological functions. When deficits are noted, follow-up with more careful and extensive neuropsychological, speech and language, motor, and academic evaluations may be necessary to more fully document their nature and extent.
Results of routine physical examinations of ADHD children are frequently normal and of little help in diagnosing the condition or suggesting its management. However, the physician certainly needs to rule out the rare possibility of visual or hearing deficits which may give rise to ADHD-like symptoms. Also, on physical inspection, ADHD children may have a greater number of minor physical anomalies in outward appearance (e.g., an unusual palmar crease, two whirls of hair on the head, increased epicanthal fold, or hyperteliorism). However, studies conflict on whether such findings occur more often in ADHD, but certainly they are nonspecific to it, being found in other psychiatric and developmental disorders. Examining for these minor congenital anomalies may only be beneficial when the physician suspects maternal alcohol abuse during pregnancy so as to determine the presence of fetal alcohol syndrome. The existence of small palpebral fissures and midfacial hypoplasia with growth deficiency supports this diagnosis.
Finally, given the considerably greater distress ADHD children present to their caregivers, their risk of being physically abused would seem to be higher than normal. Greater attention by physicians to physical or other signs of abuse during the examination is therefore required.
Results from the routine examination for growth in height and weight is also often normal, although one study reported a younger bone age in children with minimal brain dysfunction, including hyperactivity. Nevertheless, when the physician contemplates a trial on a stimulant drug, it is necessary to have accurate baseline data on physical growth, heart rate, and blood pressure against which to compare subsequent repeat exams during the drug trial or during long-term maintenance on these medications.
Similarly, findings from the routine neurological examination are frequently normal in ADHD children. These children may display a greater prevalence of soft neurological signs suggestive of immature neuromaturational development, but again, these are nonspecific for ADHD and can often be found in learning-disabled, psychotic, autistic, and intellectually disabled children, not to mention a small minority of normal children. Such findings are therefore not diagnostic of ADHD, nor does their absence rule out the condition. Instead, findings of choreiform movements, delayed laterality development, fine or gross motor incoordination, dysdiadochokinesis, or other soft signs may suggest that the child requires more thorough testing by occupational or physical therapists and may be in need of some assistance in school with fine motor tasks or adaptive physical education.
ADHD children may also have a somewhat higher number of abnormal findings on brief mental status examinations or screening tests of higher cortical functions, especially those related to frontal lobe functions (e.g., sequential hand movement tests, spontaneous verbal fluency tests, and go-no-go tests of impulse control). When these are found, more thorough neuropsychological testing may be useful in further delineating the nature of these deficits and providing useful information to educators for making curriculum adjustments for these children. In some cases, findings on brief mental status exams may have more to do with a coexisting learning disability in a particular case than with the child’s ADHD. When problems with visual-spatial-constructional skills or simple language abilities are noted, they are most likely signs of a comorbid learning disorder, as they are not typical of ADHD children generally. It is often the case that these brief mental status examinations show normal behaviors. This does not necessarily imply that all higher cortical functions are intact, as these screening exams are often relatively brief and are crude methods of assessing neuropsychological functions. More sensitive – and lengthier – neuropsychological tests may often reveal deficits not detected during a brief neurological screening or mental status exam. Even so, the routine assessment of ADHD children with extensive neuropsychological test batteries is also likely to have a low yield, as discussed above. It should be undertaken only when there is a question of coexisting learning or processing deficits that require further clarification, and even then tests should be selected carefully to address these specific hypotheses.
Laboratory Tests
A number of studies of ADHD children have used a variety of physical, physiological, and psychophysiological measures to assess potential differences between ADHD and other clinical or control groups of children. Although some of these studies have demonstrated such differences, as in reduced cerebral blood flow to the striatum or diminished orienting galvanic skin responses, none of these laboratory measures are of value in the diagnostic process as yet. Parents, teachers, or even other mental health professionals are sometimes misled by reports of such findings or by the conclusion that ADHD is a biologically based disorder, and they frequently ask for their children to be tested medically to confirm the diagnosis. At this moment, no such tests exist. Consequently, laboratory studies such as blood work, urinalysis, chromosome studies, electroencephalograms, averaged evoked responses, cerebral blood flow, magnetic resonance imaging (MRI), positron emission tomography (PET), or computerized axial tomograms (CT scans) should not be used routinely in the evaluation of ADHD children. Only when the medical and developmental history or physical exam suggests that a treatable medical problem exists, such as a seizure disorder, or that a genetic syndrome is a possibility, would these laboratory procedures be recommended, although such cases are quite rare.
Blood assays of levels of medication have so far proven unhelpful in determining appropriate dosage and therefore are not recommended as part of routine clinical titration and long-term management of these medications.
The Feedback Session
The feedback session with parents concludes the diagnostic evaluation. This session should take place after all the direct testing with the child is completed and scored and after the clinician has reviewed all the data and drawn diagnostic conclusions (the family may need to wait until after the clinician makes any necessary collateral phone calls to the school, current therapist, etc.). As with the parent interview, children under the age of 16 years old are not generally included in the feedback session, but they may be invited in at the end of the session to be given diagnostic conclusions at a level appropriate to their age and cognitive development.
The first step in the feedback session is to give parents some information about ADHD. I generally explain to parents that ADHD is defined as a developmental disorder, not mental illness or the result of stress in families. The developmental delay affects the child’s ability to regulate behavior, control activity level, inhibit impulsive responding, or sustain attention. In other words, the child with ADHD will be more active, impulsive, and less attentive than other children of the same age.
I then explain that there is no direct test for ADHD – no lab test, X-ray, or psychological test that definitely tells us that a child has ADHD. What has to be done instead is to collect a lot of information and analyze it statistically. Everything that has been learned about their child has been scored, and these scores are compared with the scores that have been collected on hundreds if not thousands of children of the same age. If their child’s scores are consistently placing him or her at or above the 95th percentile in the areas of activity level, impulse control, or attention span, those scores suggest ADHD because it suggests that the child is having more difficulty than 95 of 100 children of the same age. This is the level of “developmental deviance” that must be established.
The second step is to establish a history consistent with the notion of a “developmental” problem. Do these symptoms have a long-standing history that stretches back over time, for at least the past year, or since before the age of 12 – not something that cropped up last week or last month, or something that only came about after a trauma occurred in the child’s life.
The third step is to rule out any other logical explanation for the problem. Is there anything else going on that would overrule ADHD as a diagnosis or be a better explanation than ADHD for the problems the child is having?
I then walk parents through the data obtained about their child, step by step, so they can see clearly how the diagnostic conclusion was reached. These steps include the following:
- Explanation and results of the ADHD Rating Scale
- Parent interview responses
- Parent ADHD Rating Scale
- Teacher ADHD Rating Scale
- Executive Function Rating Scales
- Broad-band scale results
- Parent version
- Teacher version
- Functional Impairment Rating Scale
- Parenting Stress Inventory
- Social Skills Rating System
- Adaptive Behavior Inventory
- Results of Psychological Testing
Before any discussion of a treatment plan occurs, parents are asked if they have any questions about the diagnostic process or any comments about the conclusions that were drawn. Parents are always asked if they are surprised that their child was (or was not) diagnosed with ADHD.
By walking parents through the data this way, any confusion can be quickly clarified. Parents should leave the diagnostic interview with the impression that the clinician was comprehensive and competent. This sense of security will help them cope with the grief and disappointment they may experience at being told that their child has a developmental disability, as well as the confidence to follow any treatment recommendations that are made.
Conclusion on Assessment
It should be clear from the foregoing that the assessment of ADHD children is a complex and serious endeavor requiring adequate time (approximately three hours, exclusive of medical exam and psychological testing), knowledge of the relevant research and clinical literature, as well as differential diagnosis, skillful clinical judgment in sorting out the pertinent issues, and sufficient resources to obtain multiple types of information from multiple sources (parents, child, teacher) using a variety of assessment methods. When time and resources permit, direct observations of defiant and ADHD behaviors in the classroom could also be made by school personnel. At the very least, telephone contact with a child’s teacher should be made to follow up on his or her responses to the child behavior rating scales and to obtain greater detail about the classroom behavior problems of the defiant child. To this list of assessment methods would be added others necessary to address any comorbid problems often found in conjunction with ADHD in children.
Treatment Approaches
Research on the treatment of ADHD over the past two decades has focused largely on evaluating multi-modal treatment packages. Innovations have mainly occurred in (a) new delivery systems within psychopharmacology and even new drug development, and (b) evaluating cognitive rehabilitation software aimed at symptoms of inattention and deficient working memory, such as CogMed. This is not to say that more information on the prevailing treatments has not been gained over the past decade; that is hardly the case (Gallagher & Wahba, 2024; Lalonde et al., 2025). For instance, more rigorous research using sham biofeedback as a placebo control has shown the ineffectiveness of neurofeedback (EEG biofeedback) in reducing or alleviating the symptoms of ADHD, especially when blinded evaluations of symptoms by caregivers is employed. Also, behavioral parent training has been shown to be far more beneficial for parent-child conflict and child oppositional behavior than for ADHD symptom reduction. This is to say that few significant breakthroughs in the psychosocial treatment of the disorder have been forthcoming, with perhaps the exception of a new social skills training approach, developed by Amori Mikami, entitled Friendship Coaching (for parents) and MOSAIC (for teachers). Most of the psychosocial treatment research has served to clarify the efficacy (or lack thereof) of already extant treatment approaches, or their combinations.
A major problem in the ADHD treatment literature is a lack of documentation of long-term treatment effectiveness. Almost all of the research has focused on short-term effects (i.e., within three months), with a few studies providing intervention for up to 14 months with follow-up evaluations going on for several years thereafter. Thus, at the time of initial writing of this course, long-term effects beyond a few years had been largely unstudied. This situation has been remedied somewhat by the Multimodal Treatment Study of ADHD, commonly called the MTA study, that has now followed children for 16+ years after receiving 14 months of treatment, and the New York-Montreal multimodal treatment study. These long-term studies have shed some important insight on treatment, especially regarding the efficacy of combining psychosocial and pharmacological treatment, yet they have also shown that treatment gains do not endure once treatment is discontinued. This does not mean one should abandon treatment but that one should approach it like a chronic medical illness, such as diabetes, in which treatment must be continued as needed to control impairing symptoms and reduce the risk for secondary harm from an unmanaged disorder.
Another concern regarding the treatment research on ADHD has been that despite consistent findings of improvement in core symptoms of ADHD, there have been few reports of psychosocial treatment effects on key indicators of functioning such as academic achievement or social skills. For treatment of ADHD to be considered truly effective, there needs to be documentation of effectiveness on key ecological indicators of functioning in major life activities, such as school grades, sustained peer relations, etc. Again, this situation has been somewhat remedied by the MTA as well as other multimodal studies.
Before venturing into a more detailed discussion of the efficacy of specific treatments for ADHD, it will be helpful to re-examine some traditional assumptions about the treatment of this disorder. They are being called into question not only by the theoretical model of Barkley concerning ADHD as a disorder of executive functioning, but by the results of research on etiologies, as well as the results of follow-up studies of children who had received effective treatments for various periods of time and were then followed.
Re-examining Treatment Assumptions
Advances in research on the etiologies of ADHD and in theoretical models about the disorder seem to suggest why few treatment breakthroughs, especially in the psychosocial arena, have occurred. The information yielded from these sources increasingly points to ADHD as being a developmental disorder of probable neuro-genetic and neurological origins in which some unique environmental factors (mainly bio-hazards such as toxins and brain injuries) play a role in the expression of the disorder, though far less than do genetic ones. Therefore, unless new treatments address the underlying neurological substrates or genetic mechanisms that are contributing so strongly to it, the treatment will have fleeting or minimal impact on remedying this disorder.
I am not suggesting that prevention of ADHD is an impossible goal. For instance, some have suggested that reshaping the environments of young preschoolers – such as limiting television watching – might help to prevent some cases of ADHD, although the direction of causation in this correlational relationship remains to be completely understood (children with ADHD are prone to use more televised and Internet media than typical children). Others have made a more compelling case for the reduction of environmental lead given the contribution of lead poisoning before age three years to the risk for later ADHD (see Nigg, 2006). Certainly the reduction of maternal use of alcohol and tobacco products during pregnancy would seem to be useful in view of the linkages noted earlier between these fetal neuro-toxins and risk for ADHD in the offspring of those pregnancies.
This type of preventative research and related interventions should be encouraged. However, this is a course on treatment, and by the time individuals meet diagnostic criteria for ADHD, we believe that they are on a chronic course and need to be treated accordingly. Therefore, the treatment of ADHD is actually symptomatic management as in diabetes. It is management of a chronic developmental condition and involves finding means to cope with, compensate for, and accommodate the developmental deficiencies so as to reduce the numerous secondary harms that can accrue from unmanaged disorder. These means also include the provision of symptomatic relief such as that obtained by various medications.
Given the relatively greater contribution of genotype to environment in explaining individual differences in the symptoms of the disorder, it is highly likely that treatments for ADHD, while providing improvements in the symptoms, do little to change the rank ordering of such individuals relative to each other in their post-treatment levels of ADHD. It is also likely that such treatments, particularly in the psychosocial realm, will prove to be specific to the treatment setting and agents, showing minimal generalization to other agents or settings without actively arranging for its occurrence in those other settings or with those other caregivers.
Some of the psychosocial treatments for ADHD may have carry-over effects, mostly in the form of parents or teachers providing external structure that reduces ADHD-related symptoms and especially related impairments in major life activities. Ideally, these environmental adjustments will alter the developmental trajectory of the child or adolescent with ADHD. However, such interventions are not expected to produce fundamental changes in the underlying deficits of ADHD, rather they only prevent an accumulation of failures and problems secondary to ADHD. Thus, researchers and clinicians should anticipate that long-term studies are more likely to find treatment effects on problems secondary to ADHD than on deficits specific to ADHD.
The theoretical model of ADHD discussed above suggests other reasons why treatment effects may be so limited. This is largely because, according to this model, ADHD does not result from a lack of skill, knowledge, or information. It is, therefore, not going to respond well to interventions emphasizing the transfer of knowledge or of skills, as might occur in psychotherapy, social skills training, cognitive therapies, or academic tutoring. Instead, in Barkley’s (2012, 2015, 2022) model, ADHD is viewed as being a disorder of performance – of doing what one knows rather than knowing what to do. Like patients with injuries to the frontal lobes, those with ADHD find that the disorder has partially cleaved or dissociated intellect from action, or knowledge from performance. Thus, the individual with ADHD may know how to act but may not act that way when placed in social settings where such action would be beneficial to them. The timing and timeliness of behavior is also being disrupted more in ADHD than is the basic knowledge or skill about that behavior.
From this vantage point, treatments for ADHD will be most helpful when they assist with the performance of a particular behavior at the point of performance in the natural environments where and when such behavior should be performed. A corollary of this is that the further away in space and time a treatment is from this point of performance, the less effective it is likely to be in assisting with the management of ADHD. Not only is assistance at the “point of performance” going to prove critical to treatment efficacy, but so is assistance with the time, timing, and timeliness of behavior in those with ADHD, not just in the training of the behavior itself. Nor will there necessarily be any lasting value or maintenance of treatment effects from such assistance if it is summarily removed within a short period of time once the individual is performing the desired behavior. The value of such treatments lies not only in providing assistance with eliciting behavior that is likely to already be in the individual’s repertoire at the point of performance where its display is critical, but in maintaining the performance of that behavior over time in that natural setting.
Disorders of performance like ADHD pose great consternation for the mental health and educational arenas of service. At the core of such problems is the vexing issue of just how to get people to behave in ways that they know are good for them; yet they seem to be unlikely, unable, or unwilling to perform in those ways. Conveying more knowledge does not prove as helpful as altering the motivational parameters and external cues or sources of control associated with the performance of that behavior at its appropriate point of performance. Coupled with this is the realization that such changes in behavior are maintained only so long as those environmental adjustments or accommodations are maintained as well. To expect otherwise would seem to approach the treatment of ADHD with outdated or misguided assumptions about its essential nature.
The conceptual model of executive functioning by this author as extended to ADHD brings with it many other implications for the management of ADHD (see Barkley, 2015). Some of these are briefly mentioned below:
- If the process of regulating behavior by internally represented forms of information (working memory and thinking) is delayed in those with ADHD, then they will be best assisted by “externalizing” those forms of information. Externalizing means providing physical representations of that information in the person’s sensory fields that will be needed in the setting at the point of performance to remind them to show what they know. Since covert or private information (thinking) is weak as a source of stimulus control, making that information overt and public may assist with strengthening control of behavior by that information.
- The organization of the individual’s behavior both within and across time is one of the ultimate disabilities rendered by the disorder. ADHD is to time what nearsightedness is to spatial vision; it has created a temporal myopia in which the individual’s behavior is governed even more than normal by events close to or within the temporal now and immediate context rather than by internal information that pertains to longer term, future events. Those with ADHD could be expected to be “blind to time,” and so assisted by making time itself more externally represented, by reducing or eliminating gaps in time among the components of a behavioral contingency (event, response, outcome), and by serving to bridge such temporal gaps related to future events with the assistance of caregivers and others.
- Given that the model hypothesizes a deficit in internally generated and represented forms of motivation that are needed to support goal-directed behavior, those with ADHD will require the provision of externalized sources of motivation. For instance, the provision of artificial rewards, such as tokens, may be needed throughout the performance of a task or other goal-directed behavior when there is otherwise little or no such immediate consequences associated with that performance. Such artificial reward programs become for the ADHD child similar to what prosthetic devices such as mechanical limbs are to the physically disabled, allowing them to perform more effectively in some tasks and settings with which they otherwise would have considerable difficulty. The motivational disability created by ADHD makes such motivational prostheses nearly essential for most children with ADHD.
- Given the above-listed considerations, parents and teachers should reject any approach to intervention for ADHD that does not involve helping them deal with a child or adolescent by implementing an active intervention at the point of performance. Many parents and teachers seek what might be called the “garage mechanic approach.” According to this model, a child can be dropped off someplace and be “fixed” by the “mechanic” (health care professional) without the parent or teacher “getting their hands dirty.” Such an approach is untenable, and a hands-on approach to intervention by caregivers is strongly recommended. This is true for all interventions, including pharmacotherapy.
Treatments for ADHD: Introduction
The provision of treatment services to children with ADHD has increased dramatically over the past 30 years, owing in large part to four national trends:
- the recognition by special education laws that ADHD is an eligible condition for identification and services in public schools (circa 1991),
- the growth of formally organized advocacy groups (such as Children and Adults with ADHD, see chadd.org) in the late 1980s and 1990s,
- the growth of advertising and educational efforts by pharmaceutical companies promoting new stimulant delivery systems over the past three decades, and more recently new types of medication and new delivery systems for existing medications for the management of ADHD, and
- increased continuing education programs for educational and mental health professionals on the disorder.
For instance, between 1986 and 1996, stimulant prescriptions for ADHD increased to accounting for three-fourths of all physician visits for children with ADHD, with a ten-fold increase in related services such as health counseling, and a three-fold increase in diagnostic services. This trend has continued into the mid-2010s. Nevertheless, this report also documented a decline in the use of follow-up care, apparently due to insurance obstacles, lengthy waiting lists, and limited access to pediatric specialists. Treatment appears to be increasingly provided by primary care professionals who are likely to utilize only medication management, with only 30%-40% of ADHD children being referred to and treated by mental health professionals with programs such as behavioral parent training. Those who are referred to specialists are more likely to have comorbid disorders, greater impairment, and greater family burdens. Such trends have also undoubtedly continued to the present time.
I now present the major treatment approaches employed with ADHD that have some scientifically established effectiveness. These include:
- parent counseling and behavior management training;
- psychopharmacology; and
- school behavior management.
Given the weaknesses inherent in any single treatment modality, the multi-modal approach is preferred here for treating most cases of ADHD because of the inability of medication to adequately address all cases of ADHD, especially those with coexisting disorders, such as learning disabilities, anxiety, depression, or conduct disorder, and all domains of ADHD-related impairment.
Parent Counseling and Behavior Management Training
This section briefly discusses each of the major evidence-based psychosocial treatment paradigms implemented with parents and families of children and adolescents with ADHD:
- parent education and counseling concerning ADHD;
- parent training in behavior management skills, and;
- parent training as social skills coaches. With my executive function/self-regulation theory (EF-SR) as a foundation, effective methods in each category can be made even more useful.
Parent Education and Counseling
In my 40-plus years of clinical experience, I have found parent education and counseling to be the most important step in working with families of children and teens with ADHD. Research we did years ago confirmed this when we compared behavioral parenting training (BPT) with an ADHD information control group: both groups changed nearly as much even though the information-only group was not taught the management skills that the BPT group received.
The lesson we learned was both important and sobering: simply providing correct, science-based information to parents about their child’s condition and the appropriate treatments that might be employed for it was powerful to them. It resulted in the majority of improvement in their reports about their child’s behavior and their relationship with them apart from any value they found in the specific behavior management techniques we taught only to the BPT group. And much of that information about ADHD came from EF-SR theory apart from simply basic knowledge about ADHD etiology, risks of impairment, and evidence-based treatments for ADHD management.
The information provided during the initial session often leads parents to be more receptive to the various interventions to be offered to them. I came to believe that this major shift was a consequence of a reframing of parents’ views of their child’s problems. Instead of viewing their child as “bad” or “naughty” and viewing themselves as incompetent at dealing with it or, even worse, that they were in some way the cause of the ADHD, they had moved to a more scientifically based and compassionate view that their child was born with a neurodevelopmental disorder that was not of their child’s doing or of their own. Parents we spoke to about this transition in their cognitive framework for understanding their child told us that they felt a sense of relief in knowing that they (and their child) were not the cause of ADHD through the way they were dealing with each other.
Clinical Tip:
- Parents’ reframing of ADHD may make them more open to proposed interventions. But don’t expect this to always be the case, particularly where medication is one of the options. Some parents will still want time to think about the use of medication. I view reluctance to introduce neurotropic medications into their child’s body and brain as a natural protective one and not to be maligned; instead, parents need to be informed. For more information on that option, you can refer the parents to the excellent trade book on child psychopharmacology by my friend and colleague, Timothy Wilens, MD, entitled Straight Talk About Psychiatric Medication for Children (Wilens, 2016)), or to the chapters on medications in my own book, Taking Charge of ADHD: The Complete Authoritative Guide for Parents (Barkley, 2020).
I have found that reframing ADHD as a pernicious disorder of executive function and self-regulation tends to lead to parents’ increased compassion for their child’s plight (and their own). Viewing ADHD as a disability, not "just" a problem of inattention, reduces negative judgments about the disorder and promotes forgiveness for a child’s past problems. It also, however, often leads to grief.
Be Alert to a Parental Grief Reaction
A mild, but palpable, grief reaction is normal. Most typical parents do not want to be told that their child has a relatively permanent condition that can be managed such that their child can lead a nearly typical life but, like diabetes, it cannot be cured by available interventions. I have found that parents are surprised by clinicians’ candor in forewarning them that they might experience some grief, but they are grateful as well.
You may find that some parents initially resist the diagnosis as part of denial of its presence or severity. Others experience anger or at least frustration at the many months or years it had taken them to get the right information and diagnosis about their child’s problems, including primary care clinicians who had told them there was nothing wrong or at least nothing to worry about – their child was just being a child, sometimes stated in rather condescending language to the parents. Many parents went right to the sadness or grief stage, experiencing some sense of sorrow for their child and themselves.
Clinical Tips:
- Some parents experience grieving during the feedback conference or shortly thereafter, but for others it might come during the initial parent education session. Parents negotiate the phases of grieving in varying order.
- Whenever it occurs, I believe such grieving is highly therapeutic. Indeed, having no emotional reaction to the diagnosis and the information provided in this session may signal that the parents didn’t really “get it” and might be holding on to some delusions that somewhere there is a quick cure for their child’s problems, perhaps through alternative medicine, dietary supplements, herbal remedies, cognitive training exercises or games, neurofeedback, chiropractic head massage, or other such offerings on the Internet and in their community.
- Some parents may complete the initial feedback or counseling session with you about ADHD yet show little change in their emotional state. This can be an instance of denial, but in other cases it may reflect the fact that these parents have gotten accurate information about ADHD before even consulting with you, and so their grieving has largely already occurred beforehand and what they seek from you is more confirmation of and reassurance about their earlier conclusion that their child has ADHD.
Introduce the Concept of a Delayed Executive Age
Decades ago, I invented the clinical and developmental concept of a child’s executive age. I borrowed it from the older concept of mental age as applied to intelligence and ID. After reviewing numerous research studies, including my own longitudinal research, I came to see ADHD as comprising a delay of 25%-40%+ in a child’s development of the typical EFs and the SR they provided, averaging to about 30%. This is not intended to be a precise number, but a rough clinical estimate to help parents better understand the concept of the neurodevelopmental delay characterizing ADHD.
Here are the points I suggest you make to parents:
- Explain that ADHD is more than a disorder of attention or excess movement, it is a broader, more important one of delayed and deficient executive function and the self-regulation that permits. Briefly note the seven major mental executive functions, and that most or all children with ADHD are delayed in most or all of them. This is going to manifest itself in their daily behavior and functioning through five major problems with executive function in daily life – self-restraint, time management, self-motivation, emotional self-control, and planning and problem-solving. This explanation often resonates quite well with parents as it fits better with their daily observations of their child than does reducing all of the child’s difficulties to a simplistic notion of attention deficits.
- Then note that “Your child is delayed in developing these important executive functions. This means that your child differs from typical children in a quantitative, not a qualitative way.” It is as if your child were not as tall as typical children or less skilled at art; the difference is a matter of degree, not some pathology or grossly abnormal sort of condition.
- “Your child’s delay may be about 30% – more for severe ADHD and less if it is mild. So, if your child is 10, he has the self-control and executive functions of a child of about seven.”
- “This is the approximate developmental level at which you can expect your child to self-regulate. You’ll have to adjust your expectations downward for your child’s self-regulation, independence, self-care, adaptive functioning, and other domains of life that children are required to master as they develop self-control.” I would tell parents that a lot of the conflict they are experiencing with their child or teen with ADHD happens because they are demanding that the child behave like anyone else of that chronological age, especially concerning self-management. And their child simply cannot do so, which sets up an automatic conflict between the parents and their child. It is a conflict the child cannot win because it is not possible, without treatment, for them to behave anywhere near like that of other children when it comes to doing chores, following rules, governing themselves, handling their daily responsibilities, time management, getting schoolwork done, controlling their emotions, etc. Most parents find this to be a profoundly useful insight into the nature of their child’s disorder and daily functioning.
- “To help your child with ADHD, you must restructure your demands and other features of any situation to make them more consistent with someone of their executive age.”
Clinical Tip:
Most parents can immediately see what needs to get done now to make their home life better for them and their child or teen with ADHD. But you can offer a few examples that make the point even clearer:
- “If your child is chronologically 10 and is being given the usual 3rd or 4th grade amounts of work to do for homework, that is just crazy! Therefore, the first order of business is to change the length of that homework to suit a seven-year-old. Break it up into smaller quotas, provide more supervision, help, and feedback to the child, offer up some incentives for getting it done, and find other ways to support a seven-year-old being asked to do 10-year-old amounts of work and organization. That includes talking with the teacher about making the same adjustments to the in-class and homework assignments.”
- “If your 14-year-old daughter with ADHD were asked to babysit a neighbor’s infant, you would have to remember that she has the self-control of a nine-year-old. Thus, the answer is no. We generally don’t let nine-year-old girls or boys babysit infants unattended by another adult. And the same admonition applies if a 14- to16-year-old girl with ADHD wishes to go on solo dates with a boyfriend. Remember that this is a sexually developed yet highly suggestible teen with the self-control of a nine- to 12-year-old going on a date by herself. Should you permit that? I think not. Wouldn’t chaperoned dating or group dating with many other friends and a parent to supervise them be a better option for this teen?” No wonder girls and women with ADHD suffer more sexual victimization than typical peers.
- “Think about your child as a 16-year-old who now wants to drive a car. Parents reflexively permit this because of the teen’s chronological age. But the concept here mandates that they rethink that permission. The way to address it is one of doing a lot of revamping of the normal process by which teens learn to drive independently. That is because you just gave someone with the self-regulation of an 11-year-old a license to drive independently. There are lots of adjustments to this process that need to be made, one of which is to implement a graduated approach to the licensing process that contains various stages of decreasing supervision based on success at the earlier, more supervised levels of driving. Another is to buy a device that plugs into a car’s smart-port that will block cell phone signals when the car is turned on. Or, you can download an app that will make the phone unavailable when it is moving at a speed faster than someone can walk. Another is more frequent checking-in with the teen when he is using the car, which may include GPS tracking through the find-my-phone app on most smart-phones." The point here is not what to do specifically about driving. It is to illustrate how a delay in the teen’s executive age automatically leads to sensible adjustments to our expectations and sensible accommodations to address that delay.
Emphasize That All Effective Treatments Must Be at the Point of Performance
As discussed above, the EF-SR theory of ADHD posits that those with the disorder do not suffer so much from a problem of not knowing what to do when problem situations arise in their life. Their main problem is with not doing what they know to do. Parents of children or youth with ADHD really need to learn this concept because we are all such big believers in the power of pedagogy. You teach it and they’ll do it. But not in the case of ADHD. ADHD, as SRDD, is a performance disorder, not an IDD (or information deficit disorder). It usually does not involve a problem with knowing what to do but with doing what one already knows. And performance problems can only be addressed effectively at those points of performance in the natural setting where that knowledge or skill should have been deployed. Psychosocial treatments work by altering those problematic points of performance to make the person with ADHD more likely to show what he knows. Such treatments do not work when they are instituted elsewhere with no intentional programming of how to change that point of performance, such as occurs in psychotherapy or play therapy, which make few or no provisions for helping people change those critical points of performance.
Parents need to understand this point explicitly if they are to avoid wasting time and money on therapies that make no such efforts to address the problematic points of performance and alter them in ways that make performing the right behaviors more likely. The point of performance for a problem getting classwork done is in that classroom and not at a child guidance clinic that is miles away, after school, where the child with ADHD is playing with dolls or a sand table, and with her behavior being reflected to her with psychotherapeutic intent. The point of performance for homework difficulties is the specific setting in the home and at the usual time when homework is to be done and not the office or home of a tutor once a week. Not that the latter may not be helpful with SLDs or buttressing learning of academic achievement skills. But it’s not going to fix the homework problem in that home. And the point of performance for problem behaviors at recess is that school’s playground at the actual recess periods when that child is released to play freely with others. It is assuredly not a Saturday morning social skills therapy group at a private practitioner’s mental health clinic with six to eight other kids this child has never met before and will never encounter again. Therapies like these instituted away from the key points of problematic performance do not generalize to the real-world points in the natural ecology of that child and are therefore ineffective. So, spend time in this counseling session conveying this essential idea to parents.
Introduce the 12 Best Principles for Parents
Presently, there are no formal parent-training programs or related manuals for families with a child or teen with ADHD that are founded on an EF-SR theory of the disorder. To begin to fill that gap, I have recently published a book for parents on the best principles they need to know that are largely based on this theory. In it (The 12 Principles for Raising a Child with ADHD), I set forth a series of what I consider to be the most essential ideas parents must know about managing ADHD and its EF-SR deficits in their child or teen. Space precludes a detailed examination of these principles here but, briefly, they are as follows:
Principle 1. Use the Keys to Success: Encourage parents to draw from what has contributed to the success of many adults with (a) identifying nontraditional aptitudes in your child; (b) promoting your child’s further development of these aptitudes; (c) finding community resources to further promote those aptitudes into real talents; and (d) never giving up on your child – supporting the child in constructive ways through thick and thin with unconditional acceptance and guidance.
Principle 2. Remember That It’s a Disorder: ADHD has been called the silent disability because it gives off no physical stigmata or other reminders that the child is disordered or developmentally disabled in some way. The signs of the disorder are all in the child’s behavior and cognition. This can delude parents and others into thinking there is nothing wrong with this child other than misbehavior, and people generally misbelieve that such misbehavior arises from the social environment and especially poor parenting. Periodic reminders that ADHD is as much a neurodevelopmental disorder as ASD, ID, cerebral palsy, Down’s syndrome, and other brain-based, widely accepted disabilities except that it arises from the executive, self-regulatory brain, are necessary to maintain the right framework for understanding and raising this child or teen. That framework leads toward acceptance, compassion, and a willingness to help, and away from moral condemnation as simply a “bad child” (with bad parents).
Principle 3. Be a Shepherd, Not an Engineer: This concept emphasizes the neurobiological basis of ADHD and the fact that the child with ADHD will remain in most cases a person with ADHD into adulthood. Alternatively, it means that parents cannot train ADHD out of the child merely by how they choose to deal with their child, and that there are no cures for this condition. But there are lots of ways to manage it, make accommodations for it, and otherwise cope with it so that this child can lead a relatively typical and successful life. There is no cure for child diabetes either, but we don’t give up on treating it. So, please encourage parents to accept the child they got, let go of the idea of the one they wanted, and get busy managing the condition to improve their child’s life (and their own).
Principle 4. Get Your Priorities Straight: Advise parents to reduce the number of directives and chores they give their child with ADHD to those that really matter to the child’s development. A clean bedroom on a school day is not of any developmental relevance.
Principle 5. Mindful Parenting – Be There and Be Aware: Say the following to convey this idea: “When you are with your child with ADHD, really be with your child, fully attentive to the moment, what your child is doing that is well, helpful, or just appropriate and expressive of your care for your child.”
Principle 6. Promote Your Child’s Self-Awareness and Accountability: Suggest that parents give immediate, frequent, salient feedback, approval, praise, and other consequences, after which they can move to prompting self-reporting and accountability.
Principle 7. Touch More, Reward More, and Talk Less: Say "No matter what feedback or advice you are giving, make it personal, go to the child, touch the child’s arm or shoulder as a sign of care and intimacy, make eye contact, and say what you must in brief, genuine language."
Principle 8. Make Time Real: Underscore the importance of supplementing the broken inner clock, using various external means to represent time and its passing during time-sensitive tasks.
Principle 9. Working Memory Isn’t Working: Offload It and Make It Physical! Recommend that parents place key pieces of information on cards, notes, or other media in the visual field at the point of performance to prompt their child to remember the rules for this situation.
Principle 10. Get Organized: Say "Look at all of your child’s work and play spaces and organize them with your child to make them more productive places to be."
Principle 11. Make Problem-Solving External and Concrete: Children with ADHD cannot manipulate mental information involved in problem-solving as well as others. Tell parents they need to find ways to reduce the pieces of a problem to physical forms that a child can see, manipulate, take apart, and recombine to aide mental problem-solving.
Principle 12. Be Proactive: Plan for Difficult Situations at Home and Away: Ask parents to examine their experiences with their child for obvious, recurring problematic situations. Then encourage them to strive to do the following just before starting any one of them:
1. Review verbally with your child several rules that will govern this situation and write them on a card to hand to the child if needed;
2. Have your child repeat them back to you;
3. Explain the rewards available for following the rules;
4. Explain the disciplinary consequences that will happen immediately for not doing so;
5. Give your child active things to do during this situation;
6. Reward throughout the task or event;
7. Act quickly to punish inappropriate behavior or rule violations; and
8. Evaluate with your child collaboratively how the situation played out once it is done.
Make Health and Lifestyle Recommendations
I recommended earlier that you talk to parents during the feedback session about the health risks that often affect those with ADHD so that they can start helping their child avoid these risks right away. The initial counseling or education session is a good time to make recommendations about health- and lifestyle-related problems that were noted in the evaluation. At the very least, this includes the recommendation for most children and teenagers with ADHD to increase their exercise during the week. Evidence is accumulating that routine aerobic exercise multiple times per week has beneficial effects in helping to cope with, manage, or even reduce ADHD symptoms to some degree. Besides such macro-movement, we encourage parents to incorporate micro-movements into various tasks the child may have to do, including school homework, that can help improve attention and productivity. Allowing standing and movement while working seems to help children and teens with ADHD stay on task and complete more work.
Behavioral Parent Training (BPT)
All the programs that have some evidence for their effectiveness largely target oppositional child behavior and parent-child conflict, for which they are proven to be helpful. Studies that focused on children with ADHD show only modest and inconsistent benefits of behavioral parent training
for classical ADHD symptoms or EF deficits, but considerably more for defiance and conduct problems (Chacko et al., 2024; Marguet-Doleac et al., 2023):
- In unblinded parental assessments of treatment effects, some improvements may be noted in ADHD symptoms, though even larger changes are evident in child conduct problems.
- In assessments thought to be blinded or more distal from the training (observations, teacher ratings, etc.), smaller effects, if any, are noted for ADHD, but larger, more robust effects are seen, again, for conduct problems and parent-child conflict.
All BPT programs are founded to varying degrees on social learning theory and behavior modification principles. There is certainly evidence that facets of ODD and even CD are learned and thus can be dealt with fruitfully using social learning and behavioral principles. But ADHD does not arise from such learning, which likely explains the limited and arguable success of these programs for addressing ADHD symptoms and related EF deficits.
Therefore, when considering including BPT in a particular family’s treatment plan, keep in mind that most BPT programs are optimally suited for improving child compliance with parental directives and household rules. Parenting is not the cause of ADHD, and thus improving parent management will not rid the child of the disorder. Conduct and behavioral problems such as ODD are, however, known to have a substantial contribution to their variation by parenting practices. So, it makes sense that most BPT programs would do better for child conduct problems than for ADHD symptoms.
Parents also report substantial improvements in their sense of parental competence, parenting skills, and parenting self-esteem – worthy outcomes even if the impact on child behavioral problems is not as great or evident (for ADHD). In some cases, there is arguable evidence for some improvement in marital satisfaction or parents’ own psychological problems. Perhaps that is due to parents coming to be more consistent with each other in the rules they have for their children and in how they deal with child misbehavior.
Clinical Tips:
- Recommend BPT for a majority of those families of children with ADHD where:
- ODD or related behaviors are problematic;
- Parenting appears to be disrupted (inconsistent, lax, vacillating from lax to harsh, highly emotional, timid, etc.), even if it has not yet engendered ODD at diagnosable levels;
- One parent has ADHD (which can lead to disrupted parenting); or
- The child is suffering from depression or seems to be at risk for later depression (disrupted parenting has also been shown to partially mediate the link of ADHD with concurrent or later child depression).
- For children without ODD, select certain methods from the larger program of BPT to teach for certain issues the parents may have with their child, such as dealing with chores (teach the home point system) or school misbehavior (implement a daily behavior report card). Handouts that you can use with parents for implementing these methods and others dealing with child management can be found in Appendix A. A clinician manual and a trade book are also available for my own BPT program (Defiant Child: A Clinicians Manual for Parent Training and Your Defiant Child: 8 Steps to Better Behavior, respectively). But teaching the entire eight- to 12-week program is usually not necessary.
Are BPT Programs Necessary for Children Taking ADHD Medication?
Given that ADHD medications are two to three times more effective for ADHD (and possibly ODD when it co-exists with ADHD in younger children), why bother with recommending psychosocial programs generally, and BPT in particular?
Here is why:
- 15%-25% of children with ADHD do not respond to any single ADHD medication, and 8%-10% or more may not respond well to any of them or have sufficiently serious adverse reactions to warrant immediate discontinuation. For these groups, alternatives to medication have to be provided.
- Within the first year or two of medication use, 16%-64% of families have desisted using it for a variety of reasons (cost, side effects, onset of adolescence, teen noncooperation, etc.). Parents need other tools to deal with their child’s behavioral problems in such cases.
- Medication cannot cover the entire waking day – there will be periods where the child is off medication, so parents need alternative management tools for those periods.
- 50%-80% of children and teens with ADHD have another disorder that is unlikely to be addressed by ADHD medications. While ODD in young children with ADHD is quite responsive to ADHD medications, changing as many as the symptoms of ADHD are improved, this becomes less likely in older children and teens where the ODD has persisted. In that case, social learning may solidify the ODD interaction patterns of the child or teen with ADHD (as discussed in Chapter 2 on the role of disrupted parenting in the genesis of ODD), thus requiring that countermeasures be used by parents to help the child unlearn these conflict tactics.
- Adding psychosocial programs and specifically BPT to medications usually results in additional benefits as well as increasing the percentage who are likely to respond. In some cases, it also can result in less need for medication, either via lowering doses needed or the number of doses required during the day or week, while maintaining the same level of benefit. And it increases parental acceptability of the recommendation to use medications – parents like to know that more is being offered them to do to help their child than simply filling a prescription.
- There exist special subpopulations of children with ADHD, and even parents, for whom opportunities to learn appropriate social and parenting behaviors were not available (adoptees from third-world orphanages, those in impoverished or crime-ridden geographic regions), and thus that lack of knowledge needs to be redressed.
- Adding BPT to a recommendation for ADHD medication may enhance parents’ acceptance of the medication as it is seen as not an exclusive treatment but as part of a more comprehensive treatment package.
How BPT Programs Are Structured
BPT programs are more structured interventions than simple parent education. Generally, they involve training parents in contingency management and other methods to help reduce problematic behavior. There are numerous well-studied BPT programs available through commercial sources, and their respective clinical manuals or books written for a parent audience are quite adequate for teaching the techniques. The most commonly used programs having some evidence for their effectiveness are:
- Defiant Children (Barkley)
- Community Opportunities for Parent Education (Cunningham)
- Parent-Child Interaction Therapy (PCIT) (Eyberg)
- The Incredible Years Program (Webster-Stratton)
- Positive Parenting Practices (PPP) (Sanders)
- Parents are Teachers (Becker)
- The Noncompliant Child (Forehand and McMahon)
- New Forest Parenting Program (Thompson)
- Parenting Hyperactive Preschoolers (Harvey)
- Treating Explosive Kids (Greene & Ablon)
Many of these programs have been around for decades. The programs by Webster-Stratton, Thompson, and Harvey are targeted mainly at preschool children. The others encompass a wider age-range, up to adolescence. There has been little innovation in these methods over that time except for two programs. One was the development of the program explicitly intended for preschool children with ADHD called the New Forest Program by Thompson and colleagues in Europe, and another was a different program for that age group by Harvey in the United States. Neither is based on my EF-SR theory. Those programs focus to some extent on ADHD-specific symptoms, such as inattention, and with preschool children, but they also convey general behavior management strategies as do traditional BPT programs. The other programs are for conduct- or behavioral-problem children and can be used until adolescence. They focus more on parent-child conflict, compliance, and improving parental consistency of consequences, as described below.
Another innovation occurred when some developers tried augmenting BPT with sessions focusing on parental stress management, mindfulness meditation, or marital/relationship therapy. While these are intuitive add-ons, research showed that there was little increase in program effectiveness.
A third innovation under way now is the development of Internet-based parental self-help versions of these programs, some of which come with periodic in-person assistance from a clinician. Unfortunately, there is no centralized registry for such programs at present for clinicians to access easily.
Most of these programs share many of the same principles and methods, despite some variations among them. Common to nearly all of these, except the last one developed by Green and Ablon , are the following methods taught to parents. (Note: The program by Green and Ablon does not focus so much on contingency management following traditional operant conditioning principles. Instead, it teaches parents collaborative problem-solving in which the child is actively invited into brainstorming possible ways of resolving parent-child conflicts so as to reach agreement with parents on a resolution. Only two studies to date by the developer have been published, both from the same single project. They showed little to no advantage of this approach over traditional BPT (my program specifically) for improving child conduct problems, although some parents reported greater acceptability of the problem-solving methods being taught):
- Increase parental attention, praise, respect, and approval for positive and prosocial child behavior as soon after the behavior as possible.
- Decrease parental expressions of negative emotions toward the child, adopting instead a more business-like but neutral tone of voice.
- Implement planned parental ignoring of those gambits of disruptive “attention-getting” behavior that is not in response to a command or instruction (noncompliance).
- Learn to give more effective commands via adjustments to the style and content by which they are given.
- Make daily responsibilities better-organized and clearer (using posted lists) while also making access to child’s daily privileges contingent on immediate compliance with parental commands, chore charts, and household rules (typically through a home token system but, for teens, through behavior contracts as well).
- Give commands to the child in person and next to the child, not by yelling loudly from several rooms or floors away. Go to the child, affectionately touch the child’s shoulder or arm, get the child to look at your face, say what you want done briefly and in a business-like tone, and if necessary, have the child say it back.
- Decrease the repetition of directives or commands that only serve to delay the inevitable confrontation around noncompliance – for instance, in my program, parents are taught to give one command, count to five, then give a warning, count to five, then implement discipline, such as loss of tokens, privileges, or placement in time-out.
- Back up such commands within 10–15 seconds after stating them with a disciplinary consequence for noncompliance. Simply put, “quit stalling.”
- Prevent escaping from compliance with the command or rule while doing something else, such as watching TV or playing a videogame, after the parent has issued the instruction. Parents are taught to eliminate these sources of competing or distracting activities before or once the command has been given.
- Implement transition planning just before entering settings or initiating activities in which conflict often occurs, in order to be more proactive and head off potential problems (as in my program, Defiant Children).
To these programs, some developers add other parent exercises focused on building up a better relationship with the child or more positive attachment. This is often done through nondirective play periods several times per week in which parents simply comment positively or otherwise attend to ongoing positive child play behavior, as in my program. Research has shown such relationship-building is not necessary for families who seek assistance with problem behaviors in primary care, school, or other community service settings that are not specifically mental health or psychiatric clinics. That is because the child’s problems usually have not reached such an extreme stage that the parent-child relationship is primarily negative. But by the time parents may seek assistance from secondary- or tertiary-level mental health settings, which are the settings in which I usually practiced, these relationship-focused exercises were important and effective to teach as the parent-child relationship can have grown quite conflicted and negative by then.
Clinical Tip:
- The greatest obstacle to recommending these programs to parents (if you are not providing the training yourself) is locating professionals within their geographic region who provide BPT of any sort. This issue of unavailability can be partly circumvented by relying on trade book versions of these interventions that parents could try to implement on their own, such as those listed above. But these will not be so effective for parents of seriously problematic children or where parental psychological limitations make a strictly self-implemented program likely to fail. So, it will be up to you to search your area to identify possible professionals who provide such training. Good places to start are regional university psychology clinics or medical center psychiatry departments that may focus on training their students in such programs. Otherwise, state psychiatric and psychological association websites may offer lists of clinicians annotated with their specialties that could offer suggestions for BPT-trained professionals.
Program Effectiveness and Predictors of BPT Success
The effectiveness of BPT declines with the age of the child, such that it is most effective in early childhood (65%-75% positive response) and remains at that level through elementary school. But by 12-14 years of age, the response rate declines to about 25%-35%. That is still better than traditional approaches to family therapy, but is just a third of the response rate for young children. Such a fall-off in benefit is not unexpected when one considers that adolescents are psychologically and socially individuating from their parents, parental influence over them is declining markedly, peer influence and other out-of-home effects are becoming more prominent in their influence, and genetic differences in personality and especially psychopathology are growing more prominent as influences on family relationships and teen disruptive behavior.
What factors predict success in these programs?
- Parental motivation to attend BPT. Parents who neither requested BPT (as at community screenings identifying high-risk or ADHD/ODD children) nor seem interested in receiving it (when offered by clinicians after an evaluation of their child) are not good candidates, as most of the former families and 28%+ of the latter will not attend any sessions even if they are free of charge.
- Parental Psychological Disorder. Parental ADHD significantly increases risk for failure in BPT, as does parental depression and SUDs. Yet evidence is mixed as to whether treating parental ADHD with medication results in improved participation in BPT. These disorders still need to be managed before or coincidental with the use of BPT in order to offer the chance to at least try to increase the likelihood of a positive response to BPT.
- Chronic health problems in the parent, such as chronic fatigue syndrome, etc. These problems make it harder to apply these methods consistently, suggesting that, where possible, the unaffected parent take on more of the childcare role while the affected parent assumes other household responsibilities instead.
- Parental education. Less-educated parents and those from lower socioeconomic strata will require more one-to-one training rather than group-based training in BPT and may not respond quite as well even then.
Clinical Tips:
- While BPT programs do not address EF-SR deficits directly, some of the methods being taught to parents are consistent with some of the management principles arising out of the EF-SR theory of ADHD:
- The time-blindness and deficits in self-motivation associated with ADHD do respond to the use of artificial rewards and to the use of swift, mild punishment for rule infractions. But the more closely components of contingencies of reinforcement are brought together, the more effective they will be with a child with EF-SR deficits.
- Making instructions brief and clear as well as posting them on chore charts or other bookkeeping methods used in token economies can help with offloading some of the working memory demands in the assigned tasks within these programs and so can be of some help to children and teens with ADHD.
- Transition-planning procedures for becoming more proactive in preparing for immediately subsequent situations that are ordinarily fraught with conflict is another way to make expectations brief, clear, and external for the child with ADHD, once again helping both with the working memory aspects of those activities as well as enhancing motivation to comply through the promise of immediate consequences.
- Be sure to give parents a clear understanding of the rationale for recommending BPT. When you have explained that ADHD does not arise from parenting, why, parents will wonder, do they need such training? As Anil Chacko and colleagues have written elsewhere, addressing this well-known obstacle to BPT – as well as ensuring that parents understand what is expected of them in such training – may help to improve participation in and compliance with it.
- If you are delivering the training, be prepared to assign homework, monitor progress, check weekly for noncompliance, and address obstacles to implementing the skills as they arise. It is not enough to simply convey the information and skill-sets to parents throughout training.
Side Effects of BPT
When treatments are powerful enough to produce behavior change, it should be no surprise that they can have side effects. Yet even though warnings about their occurrence have been sounded for decades, they have received little notice in clinical practice. It is important, therefore, to be aware of the following sorts of adverse events, common to many psychosocial interventions, among others:
- May increase patient and family distress;
- Can increase stigma or fear of stigma in children and teens;
- Family or couples’ sessions may increase conflict with others;
- Can increase patient anxiety, dissociative episodes, re-experiencing of traumatic events, distorted thinking, etc.;
- BPT and behavioral family therapy may increase aggression and family conflict;
- Group training of children and teens can lead to deviancy training;
- May cause a worsening of disorder symptoms or deterioration in treatment targets;
- Can delay getting more effective treatment (i.e., medications);
- May be more expensive than other therapies (medications);
- Often are not monitored or detected by treating clinicians who fail to consider the potential to produce harm; and
- An adverse event may be less likely to be reported to clinician by patient due to perception it may adversely impact relationship.
These and other adverse events (AEs) can occur during BPT (see Barkley, 2018, and Allan & Chacko, 2018, in References). Why? Some of these AEs arise due to variability in children’s psychological characteristics, comorbidity, etc., as well in parental fidelity in implementing the methods. Other AEs may arise from lack of clinician training in implementing these methods. About 10%-24% of parents may report a deterioration in the intended targets of treatment, such as a worsening of their child’s ODD symptoms or other conduct problems, and parent-child/teen conflict as a function of BPT. Some of these cases had quite severe ODD (or possibly DMDD) symptoms. Thus, instituting limit-setting, discipline, or even contingent use of privileges was enough to spark greater conflict between parents and children or even an escalation to violence by the child. Other children may experience an increase in sadness or depression or a decrease in self-worth, especially during the use of disciplinary methods.
Care therefore needs to be taken to ask about such adverse events periodically during training and not just naively assume that there is never any worsening of parent-child relations from such programs. And perhaps, if the child or teen is already noted to be physically violent, alternative programs may need to be used, such as that by Greene on collaborative problem solving. Or clinicians can at least implement only the positive reinforcement aspects of the BPT program.
Clinical Tip:
- For children whose language age or intellectual development is below age two or three, consider using more intensive conditioning programs such as those used for ASD children, given that much of the focus of the BPT program is language-based and that such children may be oppositional primarily due to limited language or mental abilities.
Cognitive-Behavioral Therapies (CBT) for Teens with ADHD
Parent-Adolescent Problem-Solving and Communication Training
Like BPT programs for ODD that are extrapolated to ADHD as discussed above, family training programs for parent-teen conflict (usually related to comorbid ADHD and ODD) have also been extrapolated to teens with ADHD.
One form of CBT for teens and their parents is problem-solving and communication training (PSCT). A version of this approach was initially developed by Gerald Patterson and colleagues, Maureen Forgatch, and later, John Reid, back in the 1970s and ’80s, for use with teens with aggressive behavior or conduct problems. This approach was further refined by Arthur Robin and Sharon Foster in the 1980s. The paradigm focuses on training the parents and the oppositional teen in: (1) steps of problem-solving and negotiation, (2) more positive patterns of communication during problem-solving, and (3) detecting and countering unreasonable beliefs about each other that can work to the detriment of problem-solving (e.g., “my teen is intentionally sabotaging our family life and our rules”; “if my parents loved me, they would let me do as I wish”).
Like BPT, the program focuses primarily on reducing parent-teen conflict and improving problem-solving skills in both parents and teens, as well as on better compliance with rules by the teens. It does not focus on ADHD symptoms or executive function deficits. There is evidence across several studies that the program is better at addressing such parent-teen conflict than is a wait-list control group. Booster sessions are recommended periodically to monitor family interaction problems and help sustain initial treatment gains.
Dr. Robin and I have combined elements of my Defiant Children program focused on behavior management with his PSCT approach. We tested these methods in several studies with teens having both ADHD and ODD. (The various methods are explained in our clinical manual Defiant Teens.) Our research found that both programs improved parent-teen conflict at the group level compared to a traditional family therapy-as-usual control group, although neither of our two programs was better at doing so than the other. However, fewer families dropped out of the BPT program when compared with the PSCT program. We subsequently combined these approaches and compared it to PSCT only. The combination was in some ways superior to either program used alone, particularly in preventing family drop-out from therapy. Keep in mind that we also modified the contingency management methods I developed for children to be more age-appropriate for teens (e.g., replacing time-outs with grounding, replacing token systems with point systems, etc.).
When examined at the individual level of analysis (instead of traditional group comparisons), we noted that these two programs and their combination were helpful for just a minority of families (20%-35%). Between 18% and 38% of families dropped out of these treatments before completion. And 10%-20%+ of families in the respective treatments reported worsening of family conflicts with the teen due to treatment. Just as with BPT, side effects or AEs can occur with behavioral family therapies for teens with ADHD, including deterioration in the intended targets of therapy (see Barkley, 2018b, in References). Yet these modest response rates were superior to what we found with traditional family therapy, which served as our treatment-as-usual comparison group, where only 5%-10% of families improved.
Clinical Tips:
- Future innovations with this program need to combine it with medication for the teen’s ADHD, put more focus on the peer affiliations of the teen and out-of-home activities besides parent-teen problem-solving skills, use additional services to improve competence at school, and seek out more prosocial peer groups or organized peer activities (like sports or scouts) in which to involve the teen.
- I would also recommend finding community resources to further develop any nontraditional aptitudes the teen may have (sports, art, music, drama, entrepreneurial interests, technology, etc.) as a counterweight to the limited success most teens with ADHD are having at school. That limited success can lead them to lose motivation to participate in or even attend classes and becomes a major predictor for drifting into antisocial activities and affiliation with antisocial peers.
Planning and Organizational Training of Teens with ADHD
Self-organization is a major executive function deficit in daily life associated with ADHD. Three programs have been developed that work directly with teens with ADHD on organizational skills related to schoolwork (homework, mainly).
The Sprich-Safren Program
One such program was developed by Sprich and colleagues and is a downward extension of one of the original CBT programs aimed at EF deficits in adult ADHD by Safren and colleagues. Sprich’s program comprises 12 sessions of 45+ minutes each in which therapists work individually with teens. Parents are included in several sessions to make them aware of the skill-sets being taught to their teen and how to promote their use at home. Those sessions also work on parent-teen communication in similar ways to my program with Robin noted above. Like traditional CBT, teens are given a few sessions focusing on some cognitive restructuring methods (identified as adaptive thinking) to assist them with thinking more rationally about their emotions, what may be provoking them, and how to use thought-monitoring and self-speech to try to correct maladaptive feelings and cognitions. Most sessions (modules) work on organization, time management, scheduling, managing distraction, and procrastination/self-motivation. Booster sessions are also provided after treatment termination as a form of relapse prevention.
Research with this program finds it to significantly improve teen ADHD symptoms and EF deficits based on parent ratings and independent evaluators. All teens were on medication during training and thus the program should be seen as complementary with or a supplement to medication and not as an alternative to it. Unclear is how well these benefits are sustained after treatment termination and relapse-prevention sessions. A variation on this program was also studied by other investigators and found to be effective in improving adolescent self-esteem and parent/teacher ratings of inattention. To the authors’ credit, a manual has been commercially published along with a separate workbook for adolescents so that clinicians can use them to implement this program (Sprich & Safren, 2020).
The HOPS Program
Another CBT-like program for teenagers that focuses even more on skill and strategy training of teens with ADHD, and is concentrated on school homework, is the HOPS (Homework Organization and Planning Skills) program by Langberg (2011). Most of the 16 sessions involve a therapist training the adolescent in various methods related to homework recording and scheduling, organization of materials, time management and planning, motivation, among other EF-related domains. Parents are also provided with several sessions to make them aware of the same strategies, to help them with monitoring and supporting their use at home, and even to offer some advice on using contingency management to reinforce teen utilization of the strategies.
Evidence from research shows marked improvement in homework completion and fewer problems surrounding its performance. Noteworthy here too is that a manual is commercially available for mental health clinicians to learn and implement this program as needed with clients, thus making it potentially more widely available.
The STAND Program
A third intervention targeting teen homework and schoolwork intended for ADHD adolescents is the Supporting Teens’ Autonomy Daily paradigm (STAND) developed by Sibley (2020). It also strives to address the EF-related deficits associated with adolescent ADHD, such as time management, organization, planning, and self-motivation, among others. The program uses 10–12 parent-teen one-hour weekly sessions to permit better collaboration between parent and teen in addressing the EF- and schoolwork-related problems and to tailor the methods to the specific family ecologies of each family. Doing so also allows the therapist to implement more PSCT recommendations, like my program above with Robin, to help with parent-teen communication and problem-solving. This approach differs from the two above by incorporating more sessions in which parents are involved in helping teens to implement these skills in the home setting. It also targets self-efficacy, or cognitive beliefs concerning one’s ability to master skills and succeed in meeting challenges encountered in developing adaptive functioning.
Clinical Tips:
- Be alert for adverse effects arising from these organizational training programs in a subset of teens with ADHD. These are discussed in detail by Bourchtein and Langberg (2018) along with suggestions for addressing them. Some of these AEs include increased depression, setting the teen up for additional failure to achieve goals in the program or in school, maladaptive or negative thinking and demoralization, increased apathy toward program goals, increased parent-teen conflict, greater family distress, and outright resistance to such training as described in the family training approaches above for teens with ADHD and ODD/CD.
- It is important to periodically inquire about these and other AEs during treatment, as parents and teens are often reluctant to voice them voluntarily when not prompted to do so.
Mindfulness Meditation Training of Teens with ADHD
Some research has focused on training teens with ADHD in mindfulness-based methods of improving their ADHD, their other reported psychopathologies (depression, anxiety), as well as their homework and schoolwork performance. The studies are few (four or five depending on the methodology being scientific or just clinical pre-post observations) and involve quite small samples. Their results were weak, if any, for ADHD symptoms and arguable for other areas of teen adjustment that were assessed. So, this remains an experimental approach with some promise, but it does not have sufficient evidence to recommend clinical adoption for dealing with teens with ADHD at present. It needs much greater and more rigorous research (see Davis & Mitchell review).
Friendship Coaching: Training Parents to Improve Child Social Skills
Social-skills training as traditionally taught to children and youth with ADHD at most clinics and in schools is not effective in improving the peer relations of children or teens with ADHD. This is likely due to such traditional programs not being designed based on what is known about the problems inherent in the peer relationships and interactions of children and teens with ADHD. As Amori Mikami (2015) has articulated so well, social-skills interventions for children and youth with ADHD need to be founded on empirical evidence of precisely what problems they experience interacting with other children.
The failure of such programs to improve peer relations for teens with ADHD is also due to:
- The focus on skill training, or the imparting of knowledge, in the inchoate belief that the major problem here is that children and youth with ADHD do not know appropriate social skills;
- The fact that the training is often done in groups of children initially unfamiliar to the child with ADHD, thus making generalization back to the teen’s typical social group and ecology highly doubtful; and
- The fact that many such social-skills groups take place in artificial or atypical settings and not in the flow of typical social interactions in the natural ecology of how they occur in the lives of child participants.
But as the EF-SR theory of ADHD makes plain, the greater problem in ADHD is not in knowing what to do but in not doing what you know. Imparting more knowledge about social skills, then, does not automatically translate to using those skills where and when it would have been advisable to do so (the point of performance). To be effective, any program must focus on the performance problems in the typical flow of the child’s interactions with peers, and in those natural settings.
Once the precise nature of a child’s social problems is known, on the other hand, therapists and other caregivers can create various external prompts and support at key points of performance during the natural flow of peer interactions in the typical social ecology of the child. This sort of structure or scaffolding prompts and reinforces the utilization of those social behaviors necessary to improve peer relations with typical peers in natural settings.
Based on her studies of peer problems in children with ADHD and on EF-SR theory, Mikami designed the Parental Friendship Coaching program. It is intended to address the obstacles noted above and others. The program by Mikami:
- Addresses the hypothesized performance deficits in children with ADHD. Because parents are heavily involved in their children’s social interactions, especially during playdates, Parental Friendship Coaching relies on parents to provide their children with in vivo reminders during peer interactions, increasing the probability of generalization of skills. Parents are instructed to reinforce what their child is learning, such that the parent (not the clinician) provides the child with instruction in social skills knowledge.
- Takes account of the social contextual factors that influence peer relationships, whereas traditional social skills training largely ignores the influence that peers’ attitudes, cognitions, and behaviors also have on the social problems of children with ADHD.
- Does not assume that improving the behavior of the child with ADHD will result directly in peers’ increased liking of the child with ADHD. Instead, Friendship Coaching trains the parent to arrange fun, structured social opportunities for peers to see the child with ADHD in a positive light (in some cases, this requires the peers to change their initial negative impressions of the child with ADHD) – all of which require the parents to broaden their own social networks.
- In Friendship Coaching, parents are also trained regarding how to select the “correct” potential friends who will help bring out the best social behavior in the child with ADHD.
Mikami’s Parental Friendship Coaching program consists of eight 90-minute group sessions for parents. There are also two 45-minute individual sessions. In the individual sessions, the therapist emphasizes three topics:
- Parents learn to increase the warmth and positivity in their relationships with their children with ADHD, because parents who have positive relationships with their children may help their children to have good peer relationships since children use their parents’ behaviors as a model to follow in peer interactions.
- Parents learn to coach their children in key social skills. Parents might use discussion and role plays to help children learn the skills. Yet such coaching on social knowledge and skills differs from traditional SST in several ways. First, parents focus more specifically on skills important to helping the child develop friendships. Second, parents learn how to introduce contingencies to improve the generalization of these skills during in vivo peer interactions, monitor their child’s enactment of these skills during the playdate, and if the child is not showing socially skilled behavior, to intervene via reminders or redirection. Parents then debrief their child after the playdate about the behavior the child displayed and provide any reinforcements if needed to encourage the child to display the social skills again--things found in previous research to encourage children’s skillful behavior in peer situations
- Parents are trained to address social contextual factors to maximally facilitate their child’s peer relationships. For example, it is well known that parents who have good social competence and social networks themselves help their children make friends because these parents arrange playdates for their children with the children of their own friends. Friendship Coaching trains parents to judiciously select the correct peers as potential friends for their child, such as peers who seem positively inclined toward their child (or at least not negatively inclined), who are relatively tolerant and open-minded about ADHD symptoms, who have interests like those of their child, and where the peer and their child bring out good behavior (or at least, do not bring out bad behavior) in one another.
Results of research studying this program show that it yields reliable and significant improvements in the social skills of children with ADHD. A similar program has also been developed for use by teachers in regular education settings to help children with ADHD with their social skills in that setting. Regrettably, the two programs are not yet commercially or widely available, but the parent version should be available by early 2022. I look forward to this program becoming more widely available. Until then, I do not recommend standard SST programs. Indeed, 25% of children with ADHD exposed to such SST groups get more aggressive as a function of deviancy training by more aggressive peers in the same group. As Mikami (2018) has discussed, social skills training programs can produce side effects or AEs in a substantial minority of children, including the deviancy training just noted, not to mention changes in self-perceptions and possible stigmatizing by others because of participation in such treatment.
Psychopharmacology
Undoubtedly, the most effective interventions with the largest evidence base for the management of child and teen ADHD is medication (Faraone et al., 2024). ADHD medications:
- Have a sizable evidence base for their effectiveness;
- Offer a window of safety that is incredibly well established;
- Improve 70%-90% of clinical cases, normalizing 50%-60% of such cases;
- Are convenient to administer;
- Provide an alternative when psychosocial treatments produce side effects, don’t work, or don’t work well enough;
- Are less expensive than psychosocial methods of treatment;
- Can be used for years, even into and across adulthood;
- Are active in community settings where no caregivers may be present to provide active psychosocial treatment (unsupervised activities, driving alone or with friends, free time in schools, bus rides, etc.);
- Reduce symptom severity and associated executive/self-regulatory deficits;
- May reduce family stress, parent-child conflict, adult-partner conflict;
- Reduce risks for impairments in major life activities (home, school, peers, community);
- Reduce risks for some health-related problems (obesity, injuries, substance use, etc.);
- Reduce risks for some comorbid disorders, both externalizing (oppositional, conduct) and internalizing (anxiety, depression);
- Reduce economic burden to family and society; and
- May offer the possibility of neuroprotection, (technically, neuro-enhancement) over time (see discussion below).
I review the stimulant and nonstimulant medications for children and teens with ADHD here. The next chapter provides guidance in choosing between these two classes of medications and addressing other medication issues. For even more detail about these medications, consult the References for these two chapters, especially the review by Connor. The FDA-approved medications for ADHD are listed in Table 3 in the Appendix.
Of course, as stated by Zuddas, et al. (2018), before starting medication treatment, clients with ADHD should be evaluated by their physician for:
- History of exercise syncope, undue breathlessness, and other signs of cardiovascular problems;
- Heart rate and blood pressure (plot on percentile chart);
- Height and weight (plotted on growth chart);
- Family history of cardiac disease;
- Physical exam of cardiovascular system;
- Perform an electrocardiogram if there is a past personal or family history of serious cardiac disease, a history of sudden death in young family members, or abnormal findings in personal history or cardiac exam); and
- Risk assessment for substance abuse, misuse, or diversion.
Understanding the Full Value of Medications Through the EF-SR Theory
Despite hundreds of reliable studies showing their effectiveness and safety, you will find that some parents (and some other clinicians) resist using stimulant and nonstimulant medications for ADHD in children and teenagers. Myths spread from misconceptions created in the popular press and digital media, and they tend to be tenacious.
Clinical Tips:
- To counter concerns about ADHD medications, refer parents (or other clinicians you are working with) to whatever chapters in professional textbooks or research reviews on these medications (see References) the parents may seem to welcome hearing.
- An excellent source that may also help parents of children with ADHD learn what they want to know about medications is Straight Talk about Psychiatric Medications for Kids by Dr. Timothy E. Wilens. Another source is my own book for parents, Taking Charge of ADHD: The Complete Authoritative Guide for Parents (see References).
- If you have explained ADHD according to the EF-SR theory, you will find the following explanation of how medication directly treats the origins of ADHD (neurogenetic deficits in executive function and self-regulation abilities) resonates with many parents.
Just as ADHD is far more than merely inattention, restlessness, and verbal impulsivity as it is classically portrayed in the DSM-5-TR, so too are the effects of medications for ADHD doing more than just improving those rather superficial symptom domains. Medications for ADHD are known to produce their improvements by upregulating various EF networks in the brain, including all the executive functions described in Chapter 1 and their underlying brain networks noted in the discussion of etiologies in Appendix C. As explained, much of the disruption in the development, functional variability, and problems with interconnectivity of these brain regions and the networks among them originates in either the genetics of the disorder (or executive function and self-regulation) or in acquired injuries to these brain networks. If ADHD is a neurodevelopmental disorder of largely neural-genetic origins, and less so of acquired ones, there is no logical reason not to view the medications that manage it effectively as neurodevelopmental therapies, or neurogenetic ones as I prefer to call them.
Here is the rationale:
- These medications serve to greatly improve and even normalize the functional activity of these networks and their role in various EFs while the medications are in use.
- There is also growing evidence that these medications may promote further growth, development, and connectivity among the ADHD-related brain regions through their prolonged use, at least in a substantial minority of cases.
- And those regions and networks are functioning defectively largely as a consequence of variation and mutation in the genes that build and operate them or from other factors that may have caused brain maldevelopment.
Why does viewing medication as neurogenetic treatments for a neurogenetic disorder matter? Because it counters the persistent, false claim that stimulant medications for ADHD are masking or merely papering over the “real” origins and problems of ADHD. The neurogenetic deficits in executive function and self-regulation are the real origins and problems of ADHD. These medications are getting right to the root of the disorder, and in many cases they are actually erasing the deficits (as long as the medications continue to be taken). Just as insulin may temporarily correct the underlying anatomical and physiological origins of diabetes, ADHD medications do the same for the underlying executive function and self-regulation deficits that define ADHD.
Also, when parents (and clinicians) view medications through this lens, they can see how very beneficial the medications really are; they can appreciate the wider array of neuropsychological domains and daily adaptive behaviors that these medications improve. To put it another way, with this view of ADHD medications, parents can visualize how their child might benefit in all domains of life, throughout life, as implicated in the extended phenotype of ADHD.
Consider, specifically, that ADHD medications as best demonstrated by the stimulants, are known to improve not just inhibition (self-restraint) for the majority so treated, but also self-awareness, nonverbal and verbal working memory, impulsive emotional expression and the self-regulation of emotions, motivation, and even planning and problem-solving. If EF-SR theory extended to ADHD is correct, that means that ADHD medications are improving: (1) the self-direction of human actions (EFs); (2) their privatization or internalization; and (3) especially their governing influence over behavioral guidance toward goals and the future. They are likely doing so through their effects on the basal ganglia and thalamus, which most likely is the switching station for determining public vs. private expressions of these actions being used for self-regulation. They are also directly benefiting cortical regions and their subcortical networks mediating the working memory systems, the top-down regulation of emotions and motivations for goal-directed actions, and the cortical regions crucial to manipulating cognitive representations to achieve planning and problem-solving.
Via these beneficial, albeit temporary, executive function effects, ADHD medications are improving the treated child’s (1) time management, (2) self-organization and problem solving, (3) self-restraint, (4) self-regulation of emotion, and (5) self-motivation. And furthermore, if that is the case, then they are promoting the transition along the dimensions of what is influencing or controlling human actions from: (1) external events to mental representations about time, goals, and the future; (2) the temporal now to the hypothetical future; (3) immediate consequences to delayed ones and hence delay of gratification; and (4) others to the self.
One only needs to look across the hundreds of studies on the neuropsychological and adaptive effects of these medications to understand that this is so (again, see the References). This is not to say that they do so in equal measure across everyone with ADHD and across all executive functions, which would fail to respect the heterogeneity in the EF-SR deficits seen across clients with ADHD, not to mention their individual differences in comorbidity, brain organization, and genetic functionality. But it is to say that among the 50%+ whose behavior is being normalized, and the 25%-40%+ whose behavior is being significantly improved if not normalized, these are the means in which medications are achieving those improvements.
All of that is why I boldly assert here that ADHD medications are forms of neurogenetic therapies for the EF-SR deficits inherent in ADHD – and that that is why they are by far the best treatment for ADHD in children and adolescents.
The three most commonly used drugs for the management of ADHD symptoms are the stimulants, the nonstimulant atomoxetine, and the antihypertensives (extended release formulations of guanfacine and clonidine, (see Conner’s chapter in my ADHD Handbook, 2015). All of the FDA-approved medications for child ADHD are shown in Table 3 in the Appendix.
Of these, the stimulants are by far the most utilized and most effective in terms of degree of improvement rendered in ADHD symptoms. Use of the stimulants, however, was founded on a virtual chance discovery of their effectiveness and not on any theoretical rationale. A rationale may be emerging though, in view of recent theoretical models that emphasize poor executive functioning more generally as probably being central to the nature of the disorder. Brain regions under-serving inhibition and EF appear to be involved in the etiology of ADHD, these regions are largely dopaminergic, although not entirely, and stimulants (which increase extracellular dopamine and norepinephrine) seem to produce their greatest effects within these same brain regions. Atomoxetine increases extracellular norepinephrine, but produces an indirect increase in dopamine in the prefrontal cortex that may also explain its therapeutic benefit. In contrast, guanfacine and clonidine XR work primarily by fine-tuning the alpha-2 receptors on nerve cells in the frontal cortex, or executive brain, thereby enhancing signal strength and conductivity.
Until recently, it was not clear precisely how these medications affected brain function and particularly their sites and neurochemical modes of action. It now appears as if the major therapeutic effects of the drugs are achieved through alterations in frontal-striatal activity via their impact on at least three or more neurotransmitters important to the functioning of this region and related to response inhibition, these being dopamine, norepinephrine, and epinephrine. The direct rationale, then, for employing some medications with children with ADHD may be that they directly, if only temporarily, improve the deficiencies in these neural systems related to behavioral inhibition, EF, and self-regulation.
Stimulant Medication
Since Bradley (1937) first discovered (accidentally) their successful use with behavior-problem children, the stimulants have received an enormous amount of research with meta-analyses indicating a clear benefit in managing the disorder in the short-term, and some continuing benefit to symptomatic management, risk reduction (accidental injuries, adverse driving outcomes, substance use disorders), comorbidity (especially for oppositional defiant disorder), and academic achievement when used over a longer term. As long as clients comply with treatment, benefits can be found over as long as five years (and likely more, though this has been the limited period studied in research). The results of research on stimulants overwhelmingly indicate that these medications are quite effective for the management of ADHD symptoms in most children older than five years old. Between four and five years of age, the drugs are equally as effective as in older children, with some 82% of cases responding positively. Research in the past decade has shown these medications to be safe and effective down to age three, although with somewhat fewer children responding (55% vs. 75%-80%) and with a slightly lower degree of improvement, and somewhat more cases having side effects than is usually evident in school-age children. Guidelines for the use of stimulant medications with ADHD children have been issued by both the American Academy of Pediatrics and the American Academy of Child and Adolescent Psychiatry.
The most commonly prescribed stimulants are shown in Table 3 in the Appendix. There are six different delivery systems used to convey these drugs into the body. These are shown in Table 4 in the Appendix. The stimulants include methlyphenidate (e.g., Ritalin), d-amphetamine (e.g., Dexedrine), and a combination of amphetamine salts marketed under the name Adderall. Pemoline had been available for treatment of ADHD in earlier decades, but its manufacture was discontinued more than two decades ago as a result of liver complications or failure in a small percentage of cases. It receives no further attention here. Because methylphenidate and the amphetamines share similar characteristics, these drugs are discussed collectively in this section. Bear in mind, however, that amphetamine is a more potent medication and thus produces more improvement in ADHD symptoms (and likely more side effects) than does methylphenidate in equivalent doses.
Methylphenidate and amphetamines are rapidly acting stimulants. In their immediate release (IR) formulations, the stimulants produce effects on behavior within 30 to 45 minutes after oral ingestion and peaking in their behavioral effects within two to four hours. The utility of these IR formulations in managing behavior quickly dissipates within three to seven hours, although minuscule amounts of the medication may remain in the blood for up to 24 hours. Because of their short half-life, they are often prescribed in twice- or thrice-daily doses.
An important development in treatment of ADHD is effective extended release forms of both medications. These do not represent new drugs but new delivery systems for sustaining blood levels of the drug over longer periods so as to reduce dosing to once per day, where possible. Intermediate duration versions of methylphenidate that have therapeutic effects for six to eight hours include Ritalin-SR, based on a wax matrix coating, Metadate-ER, which uses a time-release pellet technology, as do Methylin-ER, Ritalin-LA, Focalin-LA, and Metadate-CD. Adderall is considered by some to be an intermediate-duration stimulant. Once-daily stimulants include Dexedrine Spansules (d-amphetamine), Concerta (OROS methyphenidate, using an osmotic pump), and Adderall XR (a mixture of d- and l-amphetamines, using a time-release pellet technology) that may last up to 10-12 hours. More recently, lisdexamfetamine (Vyvanse) is a variation of Adderall in which the amphetamine is bound up with lysine such that the drug is only activated in the human gut and intestinal lining where an enzyme operates to cleave the lysine from the amphetamine, thereby activating the latter. The drug is as effective as Adderall XR for children. This mechanism may extend the effects of this version of amphetamine for an additional hour or two beyond that of Adderall XR. There is also an FDA-approved liquid form of extended-release methylphenidate (Quillivant XR) and now an orally dissolvable gelatin form that should be useful for children who may have difficulty swallowing tablets or capsules. In late 2018, the FDA approved a delayed-release version of both stimulant medications (Jornay PM) that can be taken at bedtime but does not activate until nine hours later. It then provides all-day symptom management for as long as the other extended release forms of the stimulants do. The advantage to such a delivery system is that it provides treatment upon the child’s awakening, whereas the other delivery systems, when taken in the morning, require time to activate. That leaves an interval in the morning when the child is essentially untreated, thus contributing to increased family conflicts, especially on school mornings.
There is some variability in the effectiveness of these longer-acting preparations. For example, the initial version of sustained-release methylphenidate (Ritalin-SR) using a wax matrix coating had erratic effects on some children and often reduced therapeutic efficacy relative to IR forms of the medication resulting from a truncation of the peak blood level below that required for an acceptable treatment response. This limitation has been overcome in other ER preparations, such as Concerta, Metadate CD, Adderall XR, and Vyvanse. Another unique feature of some of these new delivery packages such as Concerta is that they provide a steady increase in the amount of medicine delivered during the day, thus overcoming problems with diminished effect later in the day. Possibly due to the emphasis on sustained effects, some of the once-daily preparations may have limited effectiveness in the first hour or so following administration. The newly approved Jornay PM serves to overcome this problem.
Although once used predominantly for school days, there has been an increasing clinical trend toward usage throughout the week as well as on school vacations, particularly for the more moderately to severely ADHD and conduct-problem children. This treatment option appears to have a favorable benefit-to-cost ratio. Benefits have been supported by some well-designed, randomized studies. Putative costs of treatment over weekends and school holidays, mostly the concern about possible growth suppression, may not be as serious as was once believed. And treatment seven days a week helps to produce reductions in risk, and improvements in impairments, in various major life activities occurring outside of school.
The behavioral improvements produced by stimulants are in sustained attention, impulse control, and reduction of task-irrelevant activity, especially in settings demanding restraint of behavior. Generally noisy and disruptive behavior also diminishes with medication. Children with ADHD may become more compliant with parental and teacher commands, are better able to sustain such compliance, and often increase their cooperative behavior toward others with whom they may have to accomplish a task as a consequence of stimulant treatment. Research also suggests that children with ADHD are able to perceive the medication as beneficial to the reduction of ADHD symptoms and even describe improvements in their self-esteem, though they may report somewhat more side effects than do their parents and teachers.
Improvements in other domains of behavior in children with ADHD have also been demonstrated. Both overt and covert aggressive behaviors are often reduced by stimulant treatment of children with ADHD who demonstrate abnormally high levels of pre-treatment aggressiveness, although the effect on overt aggression may be somewhat less if conduct disorder is present. The quality of the children’s handwriting may also improve with medication. Academic productivity – or the number of problems completed – and accuracy of work completion also increase, in some cases dramatically, as a function of medication. In general, classroom behavior is significantly improved, as is work productivity, although there is less of an impact on academic accuracy, which is usually not as problematic for children with ADHD as is productivity. For many years, stimulants were thought not to impact academic achievement significantly, but longer-term effects on academic achievement if treatment lasts at least two years have now been documented.
It should be strongly emphasized that the effects of stimulant medication are idiosyncratic. Although reported response rates vary across studies, many reviewers have concluded that 70%-82% of children show a clinically beneficial response to any single stimulant. However, with a trial of a second stimulant, the positive response rate may approach 90%. Unfortunately, there is no way to predict in advance which children will respond to which stimulant. Similarly, among the students who do respond positively to stimulants, there is no basis for predicting which dose will be best. Most children and adolescents show maximal improvement at low to moderate doses of stimulants, but others are most improved at higher doses. In addition to this between-subject variability in doses, there is considerable variability in the domains that respond to medication. For instance, some children may improve in one domain (e.g., behavior) when treated with stimulants, but show no change, or even deteriorate, in other domains (e.g., academic performance). For this reason, I strongly recommend that treatment with stimulant medication be assessed on a case-by-case basis using measures that sample a broad range of domains of functioning.
The most frequently occurring side effects of the stimulants are mild insomnia and appetite reduction, particularly at the noon meal, and subjective reports of stomach ache, headache, and dizziness or jitteriness. These subjective side effects tend to dissipate within a few weeks of beginning medication or can be managed by reducing the dose. Temporary growth suppression (less likely to gain weight or height than unmedicated children) may accompany stimulant treatment, but is not generally severe and is transient with no evidence of growth differences by late adolescence or early adulthood in stimulant treated vs. untreated cases of ADHD. The risk of growth suppression can be managed by ensuring that adequate caloric and nutritional intake is maintained by shifting the distribution of food intake to other times of the day when the child is more amenable to eating.
Some children become irritable and prone to crying late in the afternoon as their medication may be wearing off. This may be accompanied by an increase in hyperactivity. This apparent “rebound” phenomenon appears to be rare and might be controlled by adjusting doses and dose schedules.
In approximately 1% to 2% of children with ADHD treated with stimulants, motor or vocal tics may occur. This is well within the base rate prevalence for tics in the normal population. In others where tics already exist, they can be mildly exacerbated by stimulant treatment in some cases, but may be improved in others. Reviews suggest that the risk for increasing tics in such comorbid children is mostly associated with high doses of amphetamine and not with methylphenidate. It now appears to be relatively safe to use stimulant medications with children with ADHD and comorbid tic disorders, but be prepared to reduce the dose or discontinue medication should the child experience a drug-related exacerbation of their tic symptoms that usually dissipate once medication is stopped.
To avoid potential dose-dependent side effects, I recommend a start-low-and-go-slow approach to titrating doses. That is, one begins with a low dose, slowly titrates the dose upward, and goes higher until finding the most appropriate dose for that child. I believe that dose should be the lowest possible level that produces satisfactory clinical improvement. This is contrary to some clinical practices that titrate doses to the highest tolerable level. Finding the lowest effective dose may be more difficult, but has the potential to save money in medication costs, to reduce risk of side effects, and perhaps improve compliance due to increased comfort with medication.
As mentioned previously, it has been difficult to establish any reliable predictors of response to stimulant medication in children with ADHD. Those characteristics having the most consistent relationship to predicting a positive response have been pre-treatment levels of poor sustained attention and hyperactivity. The more deviant is a child’s level on such factors, the better their response to medication. Predictors of poor or adverse responding have not been as well studied. Some research suggests that higher pre-treatment levels of anxiety are associated with poorer responding to stimulants. The results of more recent research remains mixed on this issue, with some studies finding no relationship of anxiety to stimulant response, while others do. More recently, higher symptoms of comorbid Sluggish Cognitive Tempo (see my ADHD Handbook, 2015) predict a poorer or more limited response to stimulants.
There is little doubt now that the stimulant medications are the most studied and most effective treatment for the symptomatic management of ADHD and its secondary consequences. As a result, for many children with moderate to severe levels of ADHD, this may be the first treatment employed in their clinical management. And for some, where little or no significant comorbid disorders exist, it may be the only treatment required. One multi-site study, in fact, found that among stimulant-responsive children with ADHD, adding various forms of psychosocial treatments, such as parent training, social skills training, psychotherapy, or academic tutoring, added no additional benefits beyond that achieved by medication alone. On the other hand, the results of the MTA study suggest that a more intensive multi-modal treatment may produce a broader range of positive results than are achieved by medication alone, at least for a slightly greater percentage of cases.
Despite some conflicting studies and opinions, there seems to be a general consensus that stimulant treatment is not always effective (i.e., the 20% to 30% non-response rate), nor necessary (i.e., in some cases, psychosocial treatment is sufficient), nor is it always sufficient (i.e., many children meet criteria for improved, but not recovered, when on stimulants). The issue of lack of sufficiency is particularly salient with regard to the appropriate management of the comorbid conditions often seen in ADHD, such as LD, depression, anxiety, or conduct disorder. Given that medication typically does not address all of these presenting problems shown by many children with ADHD, other treatments may be required as adjuncts.
The following issues should be considered in the decision to employ medication for the management of ADHD:
- the age of the child;
- duration and severity of symptoms;
- the risk of injury to the child if untreated (either by accident or abuse) by the present severity of symptoms;
- the success of prior treatments;
- relatively normal levels of anxiety (perhaps);
- the absence of stimulant abuse by the child or adolescent or their caregivers;
- the likelihood that the parents will employ the medication responsibly, in compliance with physician recommendations; and
- the child does not live in a group setting such as a dormitory where supervision of the medication is poor and diversion of the medication to non-ADHD students may be more likely.
Some of these latter concerns related to stimulant abuse (i.e., points 6 to 8) may be somewhat ameliorated by the longer-acting preparations of stimulants, such as Concerta or Vyvanse, that have lower abuse potential than immediate release preparations.
Several suggested paradigms for evaluating stimulant drug response in individual cases have been reported. I recognize that these are not always practical or available in clinical practice but recommend them as exemplars toward which practitioners should strive. The trial includes the traditional and mandatory initial medical check-up of the child to insure that there are no pre-existing conditions that might contra-indicate or complicate the medication trial, such as cardiac problems, unusually high levels of anxiety, and prior history of stimulant abuse, among others. This is followed by the child’s receiving a baseline evaluation on the measures (often rating scales) to be collected across the weeks of the trial (highly recommended). Such baseline evaluations must include ratings of potential side effects of the medication, given that many of these are frequently pre-existing problems with ADHD children that, if not assessed at baseline, could be misconstrued as drug side effects. The child’s participation is then scheduled for a four-week drug-placebo trial during which the child is tested on three different doses of medication (typically methylphenidate at 5, 10, and 15 mg given morning and noon) and a placebo (lactose powder placed in gelatin capsule) (optional). Arrangements are made to have the noon dose of medication given at school on schooldays, if this is an IR formulation of the medication. The parents, teachers, child, and clinical assistant conducting the assessments of the child are all kept blind to the order of medication doses and placebo until the end of the trial.
The major outcome variables are typically ratings completed by parents, teachers, and for children over eight years old, the child receiving the medication. The frequency of ratings should match the frequency of switches between dose levels in the medication trial.
One rating scale assesses the symptoms of ADHD while another is used to obtain information about side effects the child may have experienced that week. These can be given to both parents and teachers. A third rating scale (for parents) assessing functional impairment in 15 domains of life (the Barkley Functional Impairment Scale) should also be included in the trial. Furthermore, the clinical team should solicit non-standardized information relevant to impairment and other clinically or academically meaningful phenomenon. For example, teacher comments can be collected by telephone or the Internet, as are parent comments during weekly clinic visits during the medication assessment.
The ratings may be supplemented by objective data (if available and practical) such as grades and direct observations of behavior in school or in a clinic room. For example, during each weekly clinic visit, the child can be given a set of math problems of appropriate grade level to perform while seated alone in a clinic playroom. Observations can be taken of the child from behind a one-way mirror or with a video camera and the observations can be coded using the Direct Observation Form of the CBCL described above or on the Restricted Academic Situation coding sheet (see my ADHD Clinical Workbooks) for behaviors related to ADHD (i.e., off-task, fidgets, plays with objects, out of seat, etc.). In addition, the amount of work attempted and the accuracy of that work can be scored. Computerized measures such as continuous-performance tasks may also be used to assess response to medication, but the ecological validity of these measures is questionable, and therefore the value of such measures may be limited. We recognize that for the busy private or clinic-based practitioner, these supplemental measures may not be available or cost effective. But the use of rating scales to evaluate ADHD and related symptoms, side effects, and even impairments is strongly recommended.
Different dosing schedules can be evaluated. For example, in one protocol, each drug condition lasts for seven to 10 days before the child progresses to the next drug condition. The order of the drug conditions is random except that the middle and high doses, say 10 and 15 mg of IR methylphenidate, are paired such that the 10 mg condition always precedes the 15 mg condition. This is done to reduce the possibility of unnecessary side effects being provoked by beginning the trial at an initially excessive dose. An alternative approach is to switch doses daily in a counterbalanced, random order. Compared to the former, the daily crossover design helps to better control for unusual events or spurious improvement over time. However, it incurs a much higher response burden compared to weekly ratings and may reduce compliance to the protocol. Furthermore, the daily crossover design may also miss cumulative effects.
At the end of the four-week trial, the results are tabulated, and a recommendation is made concerning possible continuation of the medication and which dose seems most effective. Children not found to be responsive to this stimulant may be tried on another, and if a second stimulant does not work, other medications such as atomoxetine might be considered. Furthermore, consistent with the “start-low-go-slow” approach, children should be routinely tested on a lower dose than selected in the titration trial to see if the lower dose is sufficient. If there is still a need for improvement relative to the higher dose, then the higher dose is well-justified.
Effectiveness, Safety, and Practicality of Stimulant Medication
The rise in the use of stimulant medication is supported by numerous studies documenting the efficacy of these medications. A meta-analytic review of 62 high-quality studies found a medium-sized effect of stimulants on parent-rated behavior (mean .54) and a large effect on teacher-rated behavior (.78). Later reviews have found much the same results. Most of these studies were conducted by experts in university or medical school research programs and therefore they speak more to treatment efficacy than effectiveness as applied in typical community settings. Yet the substantial supportive research across labs, investigators, regions, and even countries, combined with the longstanding successful and ever-increasing use of this treatment in clinical practice, speaks, albeit indirectly, to both effectiveness and practicality. According to the Biglan et al. (2003) criteria, stimulant treatment is a Grade A intervention, meaning that stimulants have a level of support most appropriate for widespread dissemination.
Stimulants used to treat ADHD are very safe. At therapeutic doses, stimulants produce few negative side effects and almost all of these negative effects are symptoms youth either develop tolerance for or are reduced to a tolerable level by lowering the dose or changing to a different stimulant or non-stimulant, such as atomoxetine. Long-term negative consequences are not evident in the research literature, but the potential for mild and transient growth suppression is an issue of ongoing investigation and debate. Concerns about predisposing stimulant-treated children to later substance-use disorders have been refuted by more than 15 studies, despite a single study implying otherwise. When absorbed rapidly (e.g., inhaled nasally or injected intravenously) or taken at high doses, stimulants may result in euphoric effects and health risks similar to cocaine. Such use is uncommon and less likely with longer-acting preparations. Mortality or serious morbidity from prescribed stimulants is rare. Indeed, compared to many other commonly prescribed psychiatric medications, stimulants are among the safest drugs given to children. Nevertheless, safety may be diminished when taking stimulants in combination with other medications (e.g., clonidine) or when potent stimulants, such as Adderall XR or Vyvanse, or high doses are used with children having pre-existing cardiac abnormalities or family histories of sudden cardiac arrest.
Research specific to practical issues with stimulant medication is limited and the preliminary findings raise some questions about the effectiveness of this treatment in primary-care settings. Although taking pills seems to be a simple intervention, there are some significant barriers to daily administration of stimulant medication, including limited access to prescribing physicians, cost, inconvenience, uncertainty about dose or type of medication, side effects, and parent or child resistance to taking medication. Research on compliance is limited, but suggests that children and adolescents with ADHD tend to take less medication than prescribed due to missed doses and termination of treatment against medical advice. The high cost of some new formulations of stimulants ($60-$100 per month) may contribute to an already tenuous compliance situation, though their once-daily extended release delivery systems may counteract such a problem. The problems with compliance have high clinical liability because stimulants exert their effects only when taken as prescribed. Even the longest acting stimulants have no measurable effect 24 hours after administration, so missed doses mean the child is essentially untreated. Thus, while stimulants get high marks for safety and effectiveness, there are some practical barriers to effective use of stimulant medication.
Special Considerations with Adolescents
Although there has been much less research on stimulant treatment for adolescents than children, there is enough research to document that stimulants have similar efficacy from childhood to adolescence. However, due to increased involvement with recreational drugs that could be associated with stimulant abuse or could lead to interactions between therapeutic stimulants and recreational drugs, caution should be taken when prescribing stimulants to adolescents. Also, clinicians need to be aware of the potential for diversion of prescribed stimulant medication by an ADHD teen to other teens for recreational misuse when the ADHD teen resides in a dormitory or other group living situation with other teens, or simply has friends!
A major threat to the effectiveness of stimulant medication is the tendency for adolescents to discontinue their medication as they get older. Thus, compared to children, more vigorous monitoring and promotion of compliance is necessary when working with adolescents. To avoid premature termination of effective stimulant treatment, parents and physicians should encourage adolescents to participate in treatment decisions and self-monitoring during periodic trials of stimulants. For adolescents who do not recognize the value of taking stimulants (assuming an individualized medication trial unambiguously supports the efficacy of the stimulant), it may be necessary to negotiate behavioral contingency contracts related to the appropriate use of stimulants. Thus, in some cases, multimodal treatment with an emphasis on compliance issues may be necessary for effective stimulant treatment of ADHD in adolescents. Unfortunately, the efficacy of multimodal treatments for adolescents with ADHD has yet to be tested in a major controlled trial.
The Non-Stimulants: Atomoxetine (Strattera®) and Viloxazine (Qelbree®)
Atomoxetine was approved by the U. S. Food and Drug Administration in January of 2003 for use in children with ADHD six years of age and older, and in adolescents and adults having ADHD. Viloxazine was approved in 2019 and is comparable to atomoxetine in its mechanism of action. The drugs are highly selective inhibitors of norepinephrine reuptake with minimal to no action at other neurotransmitter sites. Their effectiveness has been established in more than ten large-scale published studies done before or shortly following FDA approval and involving various randomized, controlled clinical trials. The clinical trials clearly established both the efficacy and safety of atomoxetine for use in the management of ADHD. Many studies have been conducted since 2003 demonstrating the safety and effectiveness of this type of drug for ADHD management.
Atomoxetine and viloxazine are not stimulants in that they are not dopamine agonists. They have no abuse potential as studies show that they are not preferred over placebo by stimulant abusers and do not result in symptoms of craving, dependence, or addiction. They are therefore not scheduled, whereas the stimulants are classified as Schedule II agents. Consequently, atomoxetine is a more convenient medication as it can be prescribed without special prescription pads needed in the U.S. for Schedule II agents, can be prescribed with refills, and can be distributed to patients by physicians as samples. The fact that both drugs are unscheduled and have no abuse potential can make them an attractive alternative to families of ADHD children concerned about the use of Schedule II medications for their child.
These drugs may assist in the management of ADHD via inhibition of the norepinephrine transporter, thereby making more norepinephrine available in the extracellular space. This results in a secondary increase of dopamine in the prefrontal cortex. The fact that they do not increase dopamine levels in the nucleus accumbens (the primary dopamine-mediated reward pathway) may explain why they do not have reinforcing or otherwise addictive properties. Because they do not appear to increase dopamine levels in the striatum that helps control motor movements, they seem to have no exacerbating effect on motor and vocal tics.
Research shows that nonstimulants reduce both inattentive and hyperactive-impulsive symptoms of ADHD in more than 70% of cases. The overall effect size (degree of change in group mean scores) of nonstimulants appears to be the same as a methylphenidate preparation, such as Concerta, among children previously untreated with stimulants, but may have a smaller effect size than that seen with the stimulants in the treatment of individuals with ADHD who have had prior stimulant exposure. In controlled studies, atomoxetine has an effect size of about 0.9 to 1.0 among stimulant naïve cases, but an effect size of 0.6 to 0.8 (standard deviations) in cases with prior stimulant treatment. The effect size for the stimulants ranges from 0.8 to 1.2. Peak plasma concentrations for atomoxetine occur in one to two hours after oral ingestion and persist for six to ten hours (half-life of four hours). The medication may therefore be given in either once- or twice-daily dosing. When given in twice-daily divided doses, atomoxetine shows much longer daily coverage for ADHD symptoms than do stimulant medications. In contrast to the tricyclic antidepressants that can also affect norepinephrine re-uptake, atomoxetine demonstrates no cardiovascular toxicity or abnormalities on electrocardiogram. Atomoxetine specifically appears to improve ODD symptoms as well in ADHD children having significant levels of these symptoms. It also results in significant improvements in parent-child relations, peer relations, school behavior and academic performance, and co-existing internalizing symptoms such as depression or anxiety.
Nonstimulants can be considered a first-line agent in the treatment of ADHD in children, adolescents, and adults. Whether it is the first or second choice of a starting medication will depend upon several patient and social ecological characteristics that may exist at the time of a clinical trial. For instance, in ADHD patients with comorbid anxiety, obsessive-compulsive behavior, or tic disorders or Tourette’s syndrome, atomoxetine may be a first-choice agent given that the stimulants may exacerbate such pre-existing conditions. In cases where someone with a history of drug abuse resides with the child or where the child or adolescent has a substance-use disorder or history of such, atomoxetine may be the preferred agent because of its absence of abuse potential. Where the child or teen with ADHD may reside in a dormitory for their school year (boarding school or college), atomoxetine might be considered ahead of stimulants because of its lack of potential for diversion to dorm-mates for their own recreational use. Obviously, in cases where prior stimulant response has been poor, a nonstimulant would be the next medication in line to consider, well ahead of the tricyclic antidepressants or antihypertensive agents such as clonidine that have a greater potential for more serious side effects. And because atomoxetine does not adversely impact sleep onset, it should be considered as an alternative to stimulants where stimulant-induced insomnia is significantly problematic or in cases where sleep problems are pre-existing. Also, in cases where parents are concerned about the use of a Schedule II agent in the management of their child’s behavior – often as a consequence of adverse publicity in the popular media against Ritalin and other stimulants – atomoxetine may prove useful given its unscheduled status and hence greater acceptability among such consumers. However, where there exists an urgent need to gain control over disruptive, hyperactive-impulsive, or otherwise externalizing behavior due to imminent adverse consequences (school suspension, potential abuse of the child by caregivers, etc.), or where none of the pre-existing condition mentioned above are problematic, then stimulants would be the first choice agent due to the shorter titration period and apparently greater rapidity of an onset of a therapeutic response.
Nonstimulants are often prescribed by weight in young children (mg/kg). In children and adolescents up to 70 kg body weight, atomoxetine is initiated at a total daily dose of 0.5 mg/kg. Dose titration occurs at a minimum of every three days to a target total daily dose of approximately 1.2 mg/kg administered either as a single daily dose in the morning or as evenly divided doses in the morning and late afternoon or early evening. In children, adolescents, and adults who weigh more than 70 kg, atomoxetine is initiated at a total daily dose of 40 mg and increased after a minimum of three days to a target total daily dose of approximately 80 mg, given in the morning as two evenly divided daily doses. If no treatment benefit occurs after two to four weeks, the dose of atomoxetine may be increased to a maximum of 100 mg/day. The total daily dose of atomoxetine in children and adolescents should not exceed 1.4 mg/kg/day or 100 mg, whichever is less. During atomoxetine initiation and dose titration, contact with the prescribing physician should occur regularly. Pulse and blood pressure should be assessed on full dose. Height and weight should be followed twice yearly.
The side effects of nonstimulants are well-documented and generally benign, like the stimulants. They include chiefly sedation, gastrointestinal disturbance (nausea), decreased appetite, and upper abdominal pain. Some weight loss may be present over the first two to four months of atomoxetine treatment but tends not to persist beyond the first year. Slight increases in blood pressure and heart rate may occur, as they do with the stimulants, but are typically benign unless hypertension was a pre-existing problem, in which case neither stimulants nor atomoxetine should be considered.
Antihypertensive Medications
Two drugs originally marketed as alpha-andrenergic agonists for treating hypertension – clonidine and guanfacine – now come in an extended release formula (Capvay and Intuniv, respectively), and have become increasingly popular for the treatment of ADHD. These drugs have primarily been used as an alternative or adjunctive medication to stimulants such as methylphenidate. Studies have found that clonidine is superior to placebo in reducing ADHD symptoms and conduct problems. Empirical support for guanfacine exists as well, but was similarly weak, earning these drugs a grade of C (i.e., efficacy based primarily on studies with serious methodological limitations and on a few randomized, controlled studies).
The most commonly reported side effect of these medications is drowsiness, which occurs in about 50% of cases. This side effect is sometimes used to therapeutic advantage with children with ADHD who have difficulty falling asleep or exhibit symptom rebound after a day of taking stimulant medication. Safety concerns about the combination of stimulants and clonidine appear to be diminishing over time following some reports of deaths in the mid-1990s that were associated with, but not proven to be caused by, combining clonidine and methylphenidate. Nevertheless, there are lingering concerns about the potential electrocardiographic effects of clonidine and the potential to worsen pre-existing cardiac arrhythmias.
The need for electrocardiograms at baseline, at every dose change, and every six months when taking an anti-hypertensive agent, is a serious threat to the practicality of this medication. Also, due to possible decreased glucose tolerance, monitoring of blood glucose levels at least every six months is warranted. Furthermore, there are many unpleasant side effects reported with this drug that may hamper compliance, including headache, dry mouth, itchy eyes, weight gain, dizziness, and postural hypotension. In some cases, treatment with anti-hypertensive drugs may create new problems that mimic psychiatric disorders. For instance, there have been some reports of irritability, dysphoria, and attention impairment while on clonidine. Although side effects may be reduced and compliance may be improved with the availability of a patch, this delivery system runs the risk of causing a rash at the site of the patch. Finally, rapid withdrawal from an anti-hypertensive may cause serious problems with symptom rebound and tachycardia. Adverse effects of guanfacine appear to be similar to those of clonidine, with possibly less sedation and more agitation and headaches.
To summarize, compared to all other medications evaluated in this course, the risk-to-benefit ratio of clonidine appears to be fair, while that of guanfacine specifically is better given its lower likelihood of affecting cardiovascular functioning.
School Management of ADHD
Somewhat more research has occurred on the application of behavior management methods in the classroom with ADHD children than with parent training. Moreover, there is voluminous literature on the application of classroom management methods to disruptive child behaviors, many of which include the typical symptoms of ADHD. This research clearly indicates the effectiveness of behavioral techniques in the short-term treatment of academic performance problems in ADHD children (DuPaul et al., 2024). I have an entirely separate course on this website on managing ADHD in school, entitled ADHD Goes to School: Providing Teachers and Parents with Specific Management Strategies. Please consult that course for specific recommendations on classroom management of ADHD.
A meta-analysis of the research literature on school interventions for ADHD was conducted that comprised 70 separate experiments of various within- and between-subjects designs as well as single-case designs. It found an overall mean effect size for contingency management procedures of 0.60 for between-subject designs, nearly 1.00 for within-subject designs, and approximately 1.40 for single-case experimental designs. Interventions aimed at improving academic performance through the manipulation of the curriculum, antecedent conditions, or peer-tutoring produced approximately equal or greater effects sizes. In contrast, cognitive-behavioral treatments when used in the school setting were significantly less effective than these other two forms of interventions. Thus, despite some initial findings of rather limited impact of classroom behavior management on children with ADHD, later studies – and the totality of the extant literature – suggest that behavioral and academic interventions in the classroom can be effective in improving behavioral problems and academic performance in children with ADHD. The greatest and most reliable improvements across studies are evident with contingency management and peer-tutoring approaches, while studies of curriculum modifications, strategy training, and other cognitive-behavioral approaches are less reliable. Moreover, even with the most effective classroom interventions, the behavior of children with ADHD may not be fully normalized by these interventions.
As noted above in discussing laboratory applications of behavior therapy techniques, research suggests some promise in the use of stimulus control procedures with ADHD children, many of which can be readily adapted to the classroom. By reducing task length, “chunking” tasks into smaller units to fit more within the child’s attention span, and setting quotas for the child to achieve within shorter time intervals, some stimulus control methods may increase the success of the ADHD child with academic work. The use of increased stimulation within the task (e.g., color, shape, texture, rate of stimulus presentation) may enhance attention to academic tasks in ADHD children. Teaching styles may play an important role in how well ADHD children attend to lectures by a teacher. More vibrant, enthusiastic teachers who move about more, engage children frequently while teaching, and allow greater participation of the children in the teaching activity may increase sustained attention to the task at hand. Studies have shown that permitting ADHD children to move or participate motorically while learning a task may improve attention and performance. The use of written, displayed rules and timers for setting task time limits, as already described, may further benefit ADHD children in the classroom.
A number of studies have also shown that the contingent application of reinforcers for reduced activity level or increased sustained attention can rapidly alter the levels of these ADHD symptoms. Usually, these programs incorporate token rewards, as some research suggests that praise may not be sufficient to increase or maintain normal levels of on-task behavior in hyperactive children. Early studies in this area showed that group-administered rewards, where all children in class receive a reward contingent on the performance of one child, are as effective as individually administered rewards. One of the problems arising in such research, however, is the demonstration that simply reinforcing greater on-task behavior and decreased activity level did not necessarily translate into increased work productivity or accuracy. Since the latter are the ultimate goals of behavioral intervention in the classroom, these results were somewhat dismaying. Research now suggests that reinforcing the products of classroom behavior (i.e., number and accuracy of problems completed) not only results in increased productivity and accuracy but also indirectly in declines in off-task and hyperactive behavior.
A serious limitation to these promising results has been the lack of follow-up on the maintenance of these treatment gains over time. In addition, none of these studies examined whether generalization of behavioral control occurred in other school settings where no treatment procedures were in effect. Other studies employing a mixture of cognitive-behavioral and contingency-management techniques have failed to find such generalization with ADHD children, suggesting that improvements derived from classroom management methods are quite situation-specific and may not generalize or be maintained once treatment has been terminated.
The role of punishment in the management of classroom behavior in ADHD children has been less well studied. For instance, one study evaluated the effects of continuous and intermittent verbal reprimands and response cost on off-task classroom behaviors. It found that while each of these treatments significantly reduced disruptive and off-task behavior, the continuous use of response cost (loss of recess time, for example) was most effective.
Studies have determined that the sole use of positive reinforcement for controlling ADHD behaviors in the classroom was not sufficient to maintain improved behavior in these children unless punishment in the form of response cost was added to the program. The addition of response cost further increased rates of on-task behavior and academic accuracy. Those gains in behavior could then be maintained by an all-positive program once the response cost procedure was gradually withdrawn. However, abrupt withdrawal of the punishment contingency resulted in declines in on-task behavior and accuracy, suggesting that the manner in which response cost techniques are implemented and then faded out of classroom management programs is important in the maintenance of initial treatment gains. In general, the efficacy of response cost procedures with ADHD children has been well-documented.
What conclusions can be drawn from this literature indicate that contingency management methods can produce immediate, significant, short-term improvement in the behavior, productivity, and accuracy of ADHD children in the classroom. Secondary or tangible reinforcers are more effective in reducing disruptive behavior and increasing performance than are attention or other social reinforcers. The use of positive reinforcement programs alone does not seem to result in as much improvement nor does it maintain that improvement over time as well as does the combination of token reinforcement systems with punishment, such as response cost (i.e., removal of tokens or privileges). Such findings would be expected from the theories of ADHD discussed earlier that suggest a decreased power to self-regulate motivation and a delay in the development of internalized speech and the rule-governed behavior it affords in children with this disorder. What little evidence there is, however, suggests that treatment gains are unlikely to be maintained in these children once treatment has been withdrawn, and that improvements in behavior probably do not generalize to other settings where no treatment is in effect.
Another promising method deserving of further evaluation is the use of daily school behavior report cards employing home-based contingencies for in-class behavior and performance. As discussed above under the author’s parent training program, the method involves having a teacher rate a child’s daily school performance, either one or more times throughout a school day. These ratings are then sent home with the child for review by the parents. The parents then dispense rewards and punishments (usually response cost) at home contingent upon the content of these daily ratings. Many studies have found such home/school behavioral report cards to be useful, either alone or in combination with parent and teacher training in behavior management, in the treatment of ADHD and its related school behavioral problems.
One study examined the effects of using game-like math software to supplement mathematics instruction in three students with ADHD, again using a multiple-baseline-across-participants design. Behavioral observations and curriculum-based math probes revealed significant improvements in math performance from the software supplementation. This method offers some promise of additional supplemental interventions to those discussed above.
Other recent innovative interventions for ADHD children in school settings which have some positive effects include consultation-based support provided to school teachers by school psychologists and other qualified staff, a cost-effective approach that deserves further study. The Challenging Horizons Program uses well-trained paraprofessionals to provide multi-method behavioral treatment, tutoring, teacher consultation, and parent training using a format of group meetings with ADHD teens after school several times per week. The program is instituted at the school, thus enhancing the likelihood of teen participation. Results to date have been impressive. Power et al. (2012) combined parent and teacher behavioral consultations, daily behavior report cards, and behavioral homework interventions into a Family-School Success intervention. Results showed significant benefits for students with ADHD in grades 2-6. The use of peers as tutors has likewise shown some promise in improving the academic performance of students with behavioral disorders.
To summarize the efficacy of classroom-focused contingency management, this should be considered a grade A or B+ treatment depending on which techniques are used. Cognitive techniques and skills training appear to be failed interventions unless the techniques or skills are specifically reinforced at the point of performance. Behavior modification methods that use a combination of reward and punishment seem to have the best results, but there is still some uncertainty about which methods are best and for whom. It does seem to be clear that effects of these interventions are transient and need to be implemented over a very long term. Approaches that train parents to set up reinforcement contingencies based on teacher-to-parent communication (e.g., daily behavior reports) may be the best hope for sustained intervention across the life span of the treatment.
All of the significant barriers to the effectiveness of behavioral management discussed previously for parents apply to teachers as well. There is widespread ignorance, neglect, or poor implementation of these methods. Intensive efforts to educate and support parents and teachers in the use of these methods could make a huge difference in the functioning of many children with learning or behavior problems at school. Unfortunately, even school psychologists may not have the time or expertise to assist in setting up proper behavior management programs, so there is quite a bit of work to be done to make this a grade A intervention that is widely available. Those interested in more specific details on school management of ADHD should take my other course, ADHD Goes to School.
Behind these recommendations lie nine principles that need to be considered in planning management programs for children and teens with ADHD in school settings:
1. Rules and instructions provided to children with ADHD must be clear, brief, and often delivered through more visible and external modes of presentation than is required for the management of a non ADHD population of children.
Stating directions clearly, having the child repeat them out loud, having the child utter them softly to himself or herself while following through on the instruction, and displaying sets of rules or rule‑prompts (e.g., stop signs, big eyes, and big ears for “stop, look, and listen” reminders) prominently throughout the classroom are essential to proper management of ADHD children. Relying on the child’s recollection of the rules as well as upon purely verbal reminders is often ineffective.
2. Consequences used to manage the behavior of ADHD children must be delivered swiftly and more immediately than is needed for those children without ADHD.
Delays in consequences greatly degrade their efficacy for children with ADHD. As will be noted throughout this chapter, the timing and strategic application of consequences with children with ADHD must be more systematic and is far more crucial to their management than in children without ADHD. This is not just true for rewards, but is especially so for punishment, which can be kept mild and still be effective by delivering it as quickly upon the misbehavior as possible – swift, not harsh, justice is the essence of effective punishment.
3. Consequences must be delivered more frequently, not just more immediately, to children with ADHD in view of their motivational deficits.
Behavioral tracking, or the ongoing adherence to rules after the rule has been stated and compliance initiated, appears to be problematic for children with ADHD. Frequent feedback or consequences for rule adherence seems helpful in maintaining appropriate degrees of tracking to rules over time.
4. The type of consequences used with children with ADHD must often be of a higher magnitude, or more powerful, than that needed to manage the behavior of those children without ADHD.
The relative insensitivity of children with ADHD to response consequences dictates that those chosen for inclusion in a behavior management program must have sufficient reinforcement value or magnitude to motivate children with ADHD to perform the desired behaviors. Suffice it to say, then, that mere occasional praise or reprimands are simply not enough to effectively manage children with ADHD.
5. An appropriate and often richer degree of incentives must be provided within a setting or task to reinforce appropriate behavior before punishment can be implemented.
This means that punishment must remain within a relative balance with rewards or it is unlikely to succeed. It is therefore imperative that powerful reinforcement programs be established first and instituted over one to two weeks before implementing punishment in order for the punishment, sparingly used, to be maximally effective. Often children with ADHD will not improve with the use of response cost or time out if the availability of reinforcement is low in the classroom and hence removal from it is unlikely to be punitive. “Positives before negatives” is the order of the day with children with ADHD. When punishment fails, this is the first area that clinicians, consultations, or educators should explore for problems before instituting higher magnitude or more frequent punishment programs.
6. Those reinforcers or particular rewards which are employed must be changed or rotated more frequently with ADHD children than with other children given the penchant of the former for more rapid habituation or satiation to response consequences; apparently rewards in particular.
This means that even though a particular reinforcer seems to be effective for the moment in motivating child compliance, it is likely that it will lose its reinforcement value more rapidly than normal over time. Reward menus in classes, such as those used to back up token systems, must therefore be changed periodically, say every two to three weeks, to maintain the efficacy of the program in motivating appropriate child behavior. Failure to do so is likely to result in the loss in power of the reward program and the premature abandonment of token technologies based on the false assumption that they simply will no longer work. Token systems can be maintained over an entire school year with minimal loss of power in the program provided that the reinforcers are changed frequently to accommodate to this problem of habituation. Such rewards can be returned later to the program once they have been set aside for a while, often with the result that their reinforcement value appears to have been improved by their temporary absence or unavailability.
7. Anticipation is the key with children with ADHD.
This means that teachers must be more mindful of planning ahead in managing children with this disorder, particularly during phases of transition across activities or classes, to insure that the children are cognizant of the shift in rules (and consequences) that is about to occur. It is useful for teachers to take a moment to prompt a child to recall the rules of conduct in the upcoming situation, repeat them orally, and recall what the rewards and punishments will be in the impending situation before entering into that activity or situation. “Think aloud, think ahead” is the important message to educators here. As noted later, by themselves such cognitive self‑instructions are unlikely to be of lasting benefit, but when combined with contingency management procedures can be of considerable aid to the classroom management of ADHD children.
8. Children with ADHD must be held more publicly accountable for their behavior and goal-attainment than children without ADHD.
The weaknesses in executive functioning associated with ADHD result in a child whose behavior is less regulated by internal information (mental representations) and less monitored via self-awareness than is the case in children without ADHD. Addressing such weaknesses requires that the child with ADHD be provided with more external cues about performance demands at key “points of performance” in the school, be monitored more closely by teachers, and be provided with consequences more often across the school day for behavioral control and goal attainment than would be the case in children without ADHD.
9. Behavioral interventions, while successful, only work while they are being implemented and, even then, require continued monitoring and modification over time for maximal effectiveness.
One common scenario is that a student responds initially to a well-tailored program, but then over time, the response deteriorates; in other cases, a behavioral program may fail to modify the behavior at all. This does not mean behavioral programs do not work. Instead, such difficulties signal that the program needs to be modified. It is likely that any one of a number of common problems occurred, such as the rewards lost their value, the program was not implemented consistently, or the program was not based on a functional analysis of the factors related to the problem behavior.
Combined Interventions
Psychopharmacological and behavioral treatments are not, by themselves, typically nor completely adequate to address all of the difficulties likely to be presented by clinic-referred children or adolescents with ADHD. Optimal treatment is likely to comprise a combination of many of these approaches for maximal effectiveness (Lalonde et al., 2025). However, the extent to which combined treatments are superior to medication alone is a controversial issue, especially given the relatively high cost of many psychosocial interventions. Nevertheless, findings from the MTA study imply some potential advantages of combined treatment, tempered by other multi-site studies that may challenge that conclusion.
Some early research studies examined the utility of combining psychosocial and pharmacological treatment packages with interesting results. In many studies, the combination of contingency management training of parents or teachers with stimulant drug therapies is generally little better than either treatment alone for the management of ADHD symptoms. Several studies also found impressive results for classroom behavior management methods but found that the addition of medication provided some added improvements beyond that achieved by behavior management alone. Moreover, the combination may result in the need for less intense behavioral interventions or lower doses of medication than might be the case if either intervention were used alone.
Where there is an advantage to behavioral interventions, it appears to be related to functioning rather than symptom relief, such as reliably increasing rates of academic productivity and accuracy. Despite some failures to obtain additive effects for these two treatments, their combination may still be advantageous given that the stimulants are not usually used in the late afternoons or evenings when parents may need effective behavior management tactics to deal with the ADHD symptoms. Moreover, a minority of children (10%-25%) do not respond positively to the medications, making behavioral interventions one of the few scientifically proven alternatives for these cases.
Several early studies have examined the combined effects of stimulant medication with cognitive-behavioral interventions. The combined program was more effective in increasing on-task behavior during classwork, and decreasing teacher ratings of ADHD symptoms. However, academic productivity is improved only by the use of direct reinforcement for correct responses. In contrast, other research found no benefits of combined drug/cognitive behavioral interventions over either treatment alone on similar domains of functioning of ADHD children.
Some success for combined medication and self-evaluation procedures have been reported when social skills, such as cooperation, have been targets of intervention. Yet, when these same investigators attempted to teach anger-control strategies to ADHD children to enhance self-control during peer interactions, no benefits of combined intervention were found beyond that achieved by self-control training alone. The self-control techniques were the most successful in teaching these children specific coping strategies to employ in provocative interactions with peers which usually lead to angry reactions from the ADHD children. Medication, in contrast, served only to lower the overall level of anger responses but did not enhance the application of specific anger-control strategies. These studies suggest that each form of treatment may have highly specific and unique effects on some aspects of social behavior while not on others.
Limited research has evaluated the effects of behavioral parent training (BPT) alone and combined with child training in self-control strategies on home and school behavioral problems. The results failed to find any significant advantage for the combined treatments. BPT alone improved home behavior problems, but neither resulted in any generalization of treatment effects to the school, where no treatment had occurred. Other research did not find such a treatment combination to be superior to either treatment used alone in producing a significantly larger number of treatment responders. Once again, however, no generalization of the results to the school setting occurred.
Generally speaking, combined treatment that uses family-based behavioral interventions and stimulant medication or atomoxetine should be very safe. There are some possible safety concerns related to the multimodal treatments of ADHD that have been studied. For example, some prominent theories related to conduct problems posit that placing children with behavior problems in groups with other disruptive children could lead to some harmful effects mediated by peer facilitation of antisocial behavior. This was recently found to occur in a social skills training program for ADHD children, particularly among those who were not manifesting significant conduct problems prior to treatment. Also, this author and colleagues have twice documented an adverse effect (escalation of conflicts) during behavioral family therapy for ADHD/ODD teens on a subset of participating families. Researchers studying behavioral interventions typically do not examine their data for such subsets of adverse responders, but should be encouraged by these results to do so. Two special issues of The ADHD Report (February and March, 2018) have focused on the myriad side effects associated with various psychosocial treatments for child and adult ADHD and I advise readers to study those reports to learn more about this topic that is in dire need of greater research.
Ineffective or Unproven Therapies
Numerous questionable treatments have been attempted with children with ADHD over the past century. Vestibular stimulation, biofeedback and relaxation training, and sensory-integration exercises among others, have been described as potentially effective in either uncontrolled case reports, small series of case studies, or in some-treatment vs. no-treatment comparisons, yet are lacking in well-controlled experimental replications of their efficacy. A meta-analysis of studies examining the benefits of physical exercise suggests that it may be preferentially beneficial for participants who are hyperactive and warrants further study of this effect in better-controlled research.
I believe the reason these treatments haven’t been proven effective is that they don’t address the EF-SR deficits inherent in ADHD. Or if they try to do so, as in cognitive rehabilitation apps, they focus more on skill-training or knowledge rather than on performance of that knowledge. And none of them are done at the point of performance in the natural ecology, where such knowledge should have been employed for more effective performance. Therefore, you should not encourage clients to engage in these treatments unless or until they have used the treatments discussed in the second half of the course, which do have good evidence for their effectiveness. Parents may come across such treatments on the Internet or hear about them via friends or media, and you can advise them that the websites of government mental health agencies, such as the National Institute of Mental Health, those of professional associations, such as the American Psychiatric or American Psychological Associations, and those of charities specializing in advocating for the disorder, such as Children and Adults with ADHD, are usually much better informed and contain more credible, science-based information than do commercial websites or those of political advocacy groups. To read about scientific research on a treatment, they can use Google Scholar as their web browser to search just the science journals and medical literature.
Trigeminal Nerve Stimulation (TNS) During Sleep
In 2019, a small pilot study was conducted at UCLA by McGough and colleagues on the use of TNS, a minimal-risk and noninvasive method for performing neuromodulation, with 62 children having ADHD who were randomized to receive TNS or a sham treatment that resembled TNS. This trigeminal nerve purportedly conveys sensory information from peripheral body regions to the brain’s reticular activating system, locus coeruleus, and other centers that play some role in attention and alertness. TNS attempts to influence the trigeminal nerve via activation of its central projections to cortical structures.
The therapy has been used for the treatment of depression as well as for epilepsy. It involves wearing a small stimulator during sleep that emits low-level electrical current via an electrode worn on the forehead over the V1 branch of the trigeminal nerve for a period of eight hours each night for four weeks. Results of the study showed that ADHD symptoms were significantly reduced by the active TNS relative to the placebo condition and that clinician global ratings of impairment were improved as well. The degree of change, or effect size, was of a moderate degree (0.50), comparable to some nonstimulant medications and even some psychosocial treatments. EEG measures revealed an increase in spectral power in the right frontal and frontal midline frequency bands from the active TNS treatment. Some children reported headaches and a sense of fatigue, but none discontinued participation, while others reported increased appetite and weight gain. Heart rate was also noted to increase from the active TNS treatment.
This is the only study on this new form of treatment and must be considered a pilot or proof of concept study. Thus, it is imperative that the treatment be studied by other clinical scientists to see if these initially positive results can be replicated. Despite this need for replication, the manufacturer sought and received FDA approval for this medical device, and it is now clinically available for use under the supervision of a trained physician. I consider the treatment as interesting yet unproven at this time, given the absence of any additional confirmatory studies.
Neurofeedback (EEG Biofeedback)
Another approach to treating ADHD is neurofeedback or EEG (electroencephalogram) biofeedback. More than 40 years ago, scientists began to test EEG biofeedback. Since then some dramatic claims have been made for this kind of treatment for a variety of disorders, including ADHD. There were advertisements stating that EEG biofeedback is an effective alternative to ADHD medications; that it results in permanent changes in the brain physiology underlying ADHD; that it improves IQ, social skills, and even learning disabilities; and that such improvements can last into adulthood in up to 80% of all treated cases of children. Those are fantastic claims for any treatment. They were not subsequently borne out.
The term biofeedback means that a patient is given back information in some form (usually visual) about his biological functioning – in this case his brain activity as measured by electrodes placed near or on the scalp. These sensors detect brain electrical waves and send them to a computer for averaging and display. The computer can then be used to show the person just how much or little brain activity is taking place. In this treatment, the computer can also reward him for practicing ways to increase that activity if it is unusually low. Over a great number of sessions, typically 40 to 80 sessions over three to 10 months or longer – at a cost of several thousand dollars ($100+ per session) – the patient supposedly learns to improve their brain activity. Participants achieve this change in EEG power through mental exercises and some form of signal from the biofeedback equipment. That signal tells them if they have been successful at increasing the desired brain activity related to sustained attention and decreasing the undesired activity associated with daydreaming or distraction. Participants are then rewarded for doing so. In that sense, this treatment is a type of behavioral conditioning method that tries to increase certain behaviors and voluntary mental activities by rewarding them. The result, supposedly, is that the patient’s inattention, hyperactivity, and impulsivity will then also improve.
Research does show that lower levels of brain activity are often associated with ADHD. There is too much theta activity with ADHD, suggesting brain under-activation or under-reactivity to tasks or events, and not enough of the beta activity often associated with heightened alertness and sustained attention. So it makes some sense that trying to teach people with ADHD to increase the brain electrical activity associated with paying attention might be beneficial for controlling those attention deficits.
People can readily learn to change their brain activity, so that is not in dispute here. What is in question is whether such training produces results that generalize to ADHD-related symptoms in natural settings and domains of major life activities. It also needs to be shown that these effects last after the treatment session has ended. A large number of studies on this treatment have been published, but many lack rigorous scientific controls so that their results are open to doubt as being specific to this form of therapy and not just attention-placebo effects. One major problem for most such studies was the lack of an appropriate sham placebo condition and blinded assessments of ADHD symptoms. More recently, there have been several very well-controlled studies, mostly with children, that did use a sham form of biofeedback with blinded evaluations, and they consistently failed to show any beneficial effects on ADHD or related outcome measures for the active training versus the sham placebo feedback condition. Indeed, the better and more rigorous the study conducted, the less likely any benefits have been found. A meta-analysis of 13 randomized controlled trials by Cortese and colleagues (2016) concluded that the evidence available did not support the effectiveness of this therapy for ADHD. I therefore consider the treatment to be disproven at this time.
Moreover, I believe there are considerable drawbacks to this therapy at this time for people with ADHD. For one thing, little if any research has been done with this treatment using adults with ADHD. So, it is not clear if the treatment works on mature adult brain activity rather than maturing or developing child brain functioning. Also, the proponents of this treatment claim that it has no side effects or adverse consequences. But any treatment that is supposed to be this effective has to produce some side effects in a small percentage of people. That is because people can differ in their brain organization and also because clinicians may not always apply the treatment reliably or accurately. All effective treatments, including psychological ones, can produce side effects in some people. It is therefore quite surprising and a cause for skepticism that proponents claim that this one does not. Furthermore, the treatment is expensive, usually costing $100 per hour, supposedly requiring 30–60 sessions, and rarely covered by insurance – that’s $3,000 to $6,000, usually out of pocket. A person with ADHD could receive 12 years of ADHD medication, three years of weekly group therapy, nearly three years of twice-monthly individual therapy by a clinical psychologist, or almost two years of twice-weekly ADHD coaching for the cost of just six months of this treatment, based on current average charges.
My advice, therefore, is to try the most effective and scientifically based treatments first (medication, CBT, counseling, etc.). Only then if clients are not satisfied with their improvements should they try neurofeedback. It should be pursued then only if they have sufficient expendable income to cover the cost of treatment out of pocket. Do NOT encourage clients to take on any debt to fund this treatment or any other so long as its effectiveness remains unclear or disproven in the research literature.
Executive Function (Neuro-Cognitive) Training
Another form of psychological training uses computer games as mental exercises as a form of neurocognitive training. Typically, this involves people practicing mental exercises using games available on various computer software programs (such as BrainAge for Nintendo DS), websites (such as Lumosity.com), or separate hand-held devices (such as in CogMed, which also involves consulting with a professional on a weekly basis). These games target mental functions such as inhibition, resisting distractions, working memory, planning or anticipation, problem-solving and mental flexibility, and other EFs or general cognitive abilities. A person usually has to practice every day for 30-45 minutes or more for most days of the week for benefits to accrue, if then. The costs can run from less than $10 per month for a subscription to the Internet websites that have such games available, to $295 (or less) for a hand-held Nintendo gaming device (the BrainAge software is often free and comes with the device), and on up to $1,200-$1,500 for a hand-held device and associated professional consultation (CogMed). Some of the games can be fun, while others are entertaining initially but may become quite boring after a while. That is why some developers now recommend that parents institute a token reward program to reward children for doing these game-based exercises.
The developers often claim that engaging in such mental exercise is like physical exercise in that it can increase your capacities in the cognitive domains being practiced (attention, impulse control, memory, etc.). There were some early studies by some of the game developers that showed improvements in ADHD symptoms, including both in parent and teacher ratings. However, later studies done by other researchers mostly did not show any benefits at school or even at home if the parents doing the reporting are blind to (not informed about) the treatment and alternative treatment or sham placebo conditions were used as controls. This contradicts many of the claims made by developers of these programs. Recent reviews of this form of treatment by Rapport and colleagues (2015) and later by Sonuga-Barke and Cortese (2018) found that while a person clearly improves in playing these games, and sometimes at tasks very similar to the games, the results do not generalize to everyday activities or domains in which these mental abilities are involved. So, people could get better at a game that involves remembering long strings of digits, yet this often does not mean they are any better in their memory during everyday routines that require good memory.
I therefore consider these forms of treatment to be disproven. Once again, I do not recommend these treatments at this time unless other, more effective treatments have been used first. The results to date are not convincing enough for recommending this training approach as a treatment for ADHD.
Diet: Fish Oils and Other Supplements
Many dietary supplements, such as omega 3/6 fish oil supplements, other antioxidants such as pycnogenol, or vitamin or nutrient supplements (zinc, iron, magnesium) have been proposed as beneficial for treating children with ADHD. Research to date has not shown much if any benefit, with negligible effects or none at all when tested with children with ADHD using rigorous scientific methods (see reviews by Buitelaar, et al., 2018, and Hurt & Arnold, 2015, in References). Children with baseline vitamin deficiencies who have ADHD should certainly receive some dietary supplements so as to try to rectify those deficiencies, as Nigg (2017) recommends. But as a treatment for all ADHD cases in which no deficiencies are evident, the research simply does not support doing so at this time.
Some early clinical evidence was initially positive for the omega 3/6 supplements (case testimonials). The treatment was not studied very scientifically using randomized assignments to treatment or control groups until relatively recently. The more recent randomized trials used larger samples, control groups, placebos, and blinded evaluations of improvement. They found very small improvements from these oils, mainly for inattention, and quite mixed or variable evidence across studies (see reviews by Nigg and colleagues, and Sonuga-Barke and colleagues in References). A small degree of effect may have been found for improving emotional regulation, but even that would need to be replicated. What little improvement on ADHD symptoms that was found in some studies did occur on inattention, but was small in degree and limited to about 25% of the sample, mostly those who were just inattentive and not impulsive or hyperactive. Also, the degree of change in symptoms was rather modest and does not rise to a level sufficient to be considered as a clinical treatment for the disorder.
A recent meta-analysis concluded that there was little benefit from this supplement for those who had ADHD. That is why for now I consider this treatment approach disproven, even if some small effects on inattention might result. Those are hardly a basis on which to classify this as a clinical treatment.
Elimination Diets
Another approach to managing ADHD, typically in children, that has been popular is removing certain substances from the client’s routine diet. This can involve eliminating or reducing sugar, food additives and preservatives, artificial flavors, and artificial coloring. One of the first such approaches, started 40 years ago, was the Feingold diet that argued for eliminating most or all colorings, flavorings, and preservatives in children’s daily diets. These treatments were supposed to cure 60%-80% of all ADHD. When well-conducted scientific studies were done, the results did not support these claims. The most recent meta-analysis of research on the removal of these substances found no effects once children who were also taking ADHD medications were removed from the analyses (see Buitelaar and colleagues in References). There is a very small effect evident in some studies for the removal of food coloring benefiting ADHD symptoms, but the effect is not clinically important even if statistically significant.
Another more recent program from Holland has been called the restrictive elimination diet, or RED. It recommends removal of dairy, gluten, citrus fruits, corn and corn-containing products, and all processed foods from children’s diets and it claims near-miraculous effects of doing so. Some of the most extreme results in the research by the developer of this diet appear highly questionable given that they claim to be three to five times more effective than stimulant medications – a near impossibility.
There is no evidence currently that sugar causes ADHD or that removing it benefits people with ADHD. The same is true so far for additives, preservatives, and flavorings. Moreover, the more rigorous were the studies (using randomized assignment to groups, placebo controls, blinded conditions, etc.), the weaker were the results. The elimination diets are also lacking compelling support, with results appearing to have more to do with whether or not the people rating the results of the diets were blinded to the nature of the diet children were receiving than to an actual demonstrable effect of the diet itself. Those REDs can be quite difficult to implement and, if focused mainly on “organic” foods, can be relatively expensive compared to typical grocery prices. [The research on the various dietary approaches to ADHD has been nicely reviewed by Arnold and Hurt (2015). Their even earlier review with Lofthouse remains informative (Hurt, Lofthouse, & Arnold, 2011) as are the meta-analyses of dietary approaches to ADHD by Nigg and colleagues (2012) and Sonuga-Barke and colleagues (2013).] Both of the latter reviews and a more recent review of all available research up to 2018 concluded that there was no compelling evidence for these restrictive or other dietary approaches in the management of ADHD (see Buitelaar and colleagues in References). Although relatively harmless, except for lost time and expenses, I do not recommend such elimination diets for children or adults with ADHD at this time – to date they are disproven.
Chiropractic Head Massage
Some chiropractors use a treatment for ADHD and learning disorders that involves placing significant pressure at various points around the skull and even inside the mouth on the roof or palate. Known as scalp or skull massage or neurologic organization training, the therapy is based on a rather ridiculous idea – that nerve cells somehow became trapped in the wrong places during early brain development. Placing pressure on the skull over these points of entrapment supposedly causes the nerve cells trapped underneath to be released. That is supposed to enable the nerves to migrate to their appropriate destinations in the brain and spinal cord, and so to function better, and thereby cure the problem. There is absolutely no controlled research on this treatment and so no evidence that such manipulation or massage results in any improvement in ADHD symptoms or learning disorders. The rationale for this method is so absurd that I consider it to be unproven and unlikely to receive serious scientific study.
Complementary and Alternative Treatments
Bader and Adesman (2015) reviewed available evidence for the following complementary and alternative treatments being offered to the public for management of ADHD: yoga, massage, homeopathy, chiropractic adjustments, exercise and green space, acupuncture, occupational therapies, caffeine, transcranial magnetic stimulation of the brain, and arthroposophical therapy (intended to improve rhythm, movement, and synchronization of the body as a means to improve balance between the “nerve sense and “metabolic limb” systems). They concluded that there was promising evidence only for aerobic exercise, though the studies were of low quality at that time. There was no compelling evidence to support the use of any of these other therapies, and a few had no research on them for ADHD at all. So, except for physical exercise, I would consider these other therapies
unproven or disproven.
Conclusion on Treatment
The treatment of children and teens with ADHD is an often complex and certainly longer-term enterprise than was previously thought to be necessary. Viewed now as a chronic disorder for most children, ADHD requires treatments that must be combined and sustained in order to have a long-term impact on the quality of life and developmental outcomes of these children. Treatments appear to succeed by temporarily reducing or normalizing symptoms for as long as treatments are in effect so as to reduce the numerous secondary harms associated with unmanaged ADHD. Though numerous therapies have been proposed for this disorder, those having the greatest empirical support are contingency-management methods applied in classrooms and elsewhere (summer camps); training of parents (BPT) in these same methods to be used in the home and elsewhere (community settings); psychopharmacology, particularly stimulants and atomoxetine; and to a lesser extent, the combination of behavioral treatments with medication.
Evidence for CBT is lacking at this time, while that for social skills training programs paints a mixed picture that is based mainly on studies having significant methodological limitations. Better-controlled and larger studies appear to show little or no treatment effects when the skills or behaviors are not cued and reinforced for occurring at the specific point of performance.
Popular treatments among laypeople, such as dietary manipulations, do not have compelling evidence for their efficacy, nor do several other professionally popular treatments, such as sensory integration training.
Most cases require a combination of the more effective treatments in order to provide effective management of the disorder and its comorbid conditions. Among children who are already stimulant-responsive, it is not clear to what extent intensive psychosocial treatments provide added benefit. Interventions will need to be of high quality and sustained over several years (or more), and re-intervention is highly likely as new developmental transitions occur and new domains of potential impairment become available to the individual with ADHD across their lifespan.
Appendix
(Note: If you clicked a link to these Tables in the text of the course, click the back arrow of your internet browser to return to the text.)
Table 3. AVAILABLE FDA-APPROVED TREATMENTS FOR ADHD |
Generic Name (Brand Name) |
Formulation and Mechanism |
Duration of Activity |
How Supplied |
Usual Absolute and (Weight-based) Dosing Range |
FDA-Approved Maximum Dose for ADHD |
MPH (Ritalin)* |
Tablet of 50 : 50 racemic mixture d,l-threo-MPH |
3-4 hours |
5, 10, and 20 mg tablets |
(0.3-2 mg/kg/day) |
60 mg/day |
Dex-MPH (Focalin)* |
Tablet of d-threo-MPH |
3-5 hours |
2.5, 5, and 10 mg tablets (2.5 mg Focalin equivalent to 5 mg Ritalin) |
(0.15-1 mg/kg/day) |
20 mg/day |
MPH (Methylin)* |
Tablet of 50 : 50 racemic mixture d,l-threo-MPH |
3-4 hours |
5, 10, and 20 mg tablets |
(0.3-2 mg/kg/day) |
60 mg/day |
MPH-SR (Ritalin-SR)* |
Wax-based matrix tablet of 50 : 50 racemic mixture d,l-threo-MPH |
3-8 hours Variable |
20 mg tablets (amount absorbed appears to vary) |
(0.3-2 mg/kg/day) |
60 mg/day |
MPH (Metadate ER)* |
Wax-based matrix tablet of 50:50 |
3-8 hours Variable |
10 and 20 mg |
(0.3-2 mg/kg/day) |
60 mg/day |
MPH (Methylin ER)* |
Hydroxypropyl methylcellulose base tablet of 50:50 racemic mixture d,l-threo-MPH; no preservatives |
8 hours |
10 and 20 mg tablets
|
2.5, 5, and 10 mg chewable tablets
|
5 mg/5 ml and 10 mg/5 ml oral solution |
|
(0.3-2 mg/kg/day) |
60 mg/day |
MPH (Ritalin LA)* |
Two types of beads give bimodal delivery (50% immediate-release and 50% delayed-release) of 50 : 50 racemic mixture d,l-threo-MPH |
8 hours |
20, 30, and 40 mg capsules; can be sprinkled |
(0.3-2 mg/kg/day) |
60 mg/day |
D-MPH (Focalin XR) ‡ |
Two types of beads give bimodal delivery (50% immediate-release and 50% delayed-release) of d-threo-MPH |
10-12 hours |
5, 10, 15, 20, 25, 30, 35, and 40 mg capsules |
0.15-1 mg/kg/day |
30 mg/day in youth; 40 mg/day in adults |
MPH (Metadate CD)* |
Two types of beads give bimodal delivery (30% immediate-release and 70% delayed-release) of 50:50 racemic mixture d,l-threo-MPH |
8 hours |
20 mg capsule; can be sprinkled |
(0.3-2 mg/kg/day) |
60 mg/day |
MPH (Daytrana)* |
MPH transdermal system |
12 hours (patch worn for 9 hours |
10, 15, 20, and 30 mg patches |
0.3-2 mg/kg/day |
30 mg/day |
MPH (Concerta)* ‡ |
Osmotic pressure system delivers 50:50 racemic mixture d,l-threo-MPH |
10-12 hours |
18, 27, 36, and 54 mg caplets |
(0.3-2 mg/kg/day) |
72 mg/day |
MPH (Quillivant XR) |
Extended-release liquid |
10-12 hours |
25 mg/5 mL |
(0.3-2 mg/kg/day) |
60 mg/day |
MPH (Jornay PM) |
12 hr. Delayed release tablet (microbeads) |
12+ hours |
20, 40, 60, 80, 100 mg |
60-80 mg |
100 mg/day |
AMPH† (Dexedrine Tablets) |
d-AMPH tablet |
4-5 hours |
5 mg tablets |
(0.15-1 mg/kg/day) |
40 mg/day |
AMPH† (Dextrostat) |
d-AMPH tablet |
4-5 hours |
5 and 10 mg tablets |
(0.15-1 mg/kg/day) |
40 mg/day |
AMPH† (Dexedrine Spansules) |
Two types of beads in a 50:50 mixture short and delayed-absorption of d-AMPH |
8 hours |
5, 10, and 15 mg capsules |
(0.15-1 mg/kg/day) |
40 mg/day |
Mixed salts of AMPH† (Adderall) |
Tablet of d,l-AMPH isomers (75% d-AMPH and 25% l-AMPH) |
4-6 hours |
5, 7.5, 10, 12.5, 15, 20, and 30 mg tablets |
(0.15-1 mg/kg/day) |
40 mg/day |
Mixed salts of AMPH*‡ (Adderall-XR) |
Two types of beads give bimodal delivery (50% immediate-release and 50% delayed-release) of 75:25 racemic mixture d,l-AMPH |
At least 8 hours (but appears to last much longer in certain patients) |
5, 10, 15, 20, 25, and 30 mg capsules; can be sprinkled |
(0.15-1 mg/kg/day) |
30 mg/day in children
Recommended dose is 20 mg/day in adults |
|
| Lisdexamfetamine (Vyvanase)* ‡ |
Tablets of dextroamphetamine and L-lysine |
12 hours |
30, 50, and 70 mg tablets |
|
70 mg/day |
| Atomoxetine*‡ (Strattera) |
Capsule of atomoxetine |
5 hour plasma half-life but CNS effects appear to last much longer |
10, 18, 25, 40, 60, and 80 mg capsules |
1.2 mg/kg/day |
1.4 mg/kg/day or 100 mg |
| Guanfacine ER** (Intuniv) |
Extended-release tablet of guanfacine |
Labelled for once-daily dosing |
1,2,3 & 4 mg tablets |
Up to 4 mg per day |
Up to 4 mg per day |
| Clonidine ER**(Kapvay) |
Extended-release tablet of clonidine |
Labelled for twice-daily dosing |
0.1 mg tablet |
0.1- 0.2 mg twice daily |
Up to 0.4 mg daily |
*Approved to treat ADHD age 6 years and older
†Approved to treat ADHD age 3 years and older.
‡Specifically approved for treatment of ADHD in adults.
** Approved to treat ADHD in youth 6-17 years old as monotherapy or as adjunctive treatment with stimulant
Updated from Prince, J., et al. (2015). Psychopharmacology for adult ADHD. In R. A. Barkley (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). New York: Guilford Press. Copyright by Guilford Press 2015. Reprinted with permission.
Table 4. The Eight Stimulant Delivery Systems |
I think of the first five delivery systems as the 5 Ps – pills, pumps, pellets, patches, and pro-drug. The various brand names of ADHD medicines you will hear about are either one form or another of MPH or AMP and involve one of these delivery systems:
- Pills: These are the original versions of these medicines that have been available for many decades. The first versions of AMP were discovered in the 1930s while the first version of MPH was discovered in the 1950s. In pill form, these medications are absorbed quickly, usually within 15–20 minutes, after being taken by mouth and swallowed. They can reach their peak level in the blood (and so in the brain) in 60–90 minutes usually and may last 3–5 hours in controlling the symptoms of ADHD in most people. That was their problem. If you wanted to control the symptoms of ADHD across the waking day of, say, 14–16 hours for most adults, you had to give these medications 2–4 times per day or more often. The inconvenience that posed to people having to take these drugs is obvious, not to mention the fact that many had to remember to take these drugs so often and frequently forgot to do so. These and other problems with these immediate-release pills led pharmaceutical companies to explore better ways to get the medicines into the body and keep them active there longer. The brand names you are likely to hear about for these pills are Ritalin® (MPH, a mixture of d-MPH and l-MPH), Focalin® (just d-MPH), Dexedrine® (d-AMP), Benzedrine® (l-AMP), and Adderall® (a mixture of the d- and l-AMP forms or salts).
- The Pump: Then came the invention of an ingenious water-pump system for delivering these drugs into the body and keeping them in the bloodstream longer. The brand name for this system is Concerta®, and it contains MPH. It is a capsule-appearing container with a small laser-drilled hole on one of its long ends. Inside there are two chambers. One chamber contains a paste-like sludge of MPH, and the other chamber is empty. There is also powdered MPH coating the outside of the capsule. Now here is the neat part: when you swallow the capsule, the powder goes right to work just as it would in the pill form of MPH described above (i.e., Ritalin). That gives just enough time for the capsule to start to absorb water from your stomach (and later your intestines). The water is absorbed through the wall of the pump in a continuous, even flow into the empty chamber. As that chamber fills up, it presses against the other chamber that contains the MPH paste. That pressure then squeezes the MPH paste out of the hole in the capsule. It is designed to do that continuously for 8–12 hours or more. The final result is that many people, especially children, only need to take one capsule a day, and not the usual 2–3 (or more) they would have to take using the regular pills discussed above.
The capsules come in various-size doses of course, so that physicians can adjust the dose to better suit the individual needs and responses of their ADHD patients. One problem, though, is that some older children and teens, and especially adults, may need a longer course of medication each day than what this provides. To deal with that issue, some physicians use the pills of MPH or AMP toward the end of the day. They do this to get an extra 3–5 hours of treatment with medication after the Concerta may be losing its beneficial control of ADHD symptoms. Even so, you just have to love the human ingenuity that led to the discovery of this delivery system.
- The Pellets:At around the same time as the water-pump method was being invented, chemical (pharmacological) engineers were modifying a method that uses time-release pellets to create a way to keep medicines in the body and bloodstream longer than the pills. This method had been used for years with some cold medicines, like the old Contac brand. But the system had to be modified in various ways for use with MPH and AMP. Now we have time-release pellets for both stimulants. Little beads of the drug are coated in such a way that some dissolve immediately after being swallowed, and others dissolve in 1, 2, 3, or more hours later. This means that the drug can be more gradually activated and absorbed into the bloodstream across 8–12 hours for most people. Here is another ingenious delivery system. It has the added advantage that someone who simply cannot or does not want to swallow the capsule that contains these pellets can open the capsule (pull it apart) and sprinkle it on a teaspoon of applesauce, yogurt, or other food and swallow it that way. It does not change the way the drug will work in the body, typically.
You may have heard of these delivery systems by the brand names of Ritalin LA® (MPH), Focalin XR® (d-MPH), Medadate CD® (MPH), and Adderall XR® (AMP) here in the U.S. Again, there are different sizes (doses) to these capsules to permit a physician to adjust the dose for an individual to their optimum level. Like the water-pump method above, these time-release pellet systems sometimes are supplemented late in the day with a regular or immediate-release pill version of the same drug. That permits even longer symptom control if necessary. Some research exists that shows that this pellet system gives a little better control of ADHD symptoms in the morning than afternoon hours. In contrast, the pump system provides a bit better control in the afternoon than morning hours. Both delivery systems provide good control of ADHD symptoms across the day but not at the same hours of the day. This can be an issue sometimes in deciding which delivery system may be better for someone depending on when they need the greatest control of their ADHD symptoms during the day.
- The Patch:The next invention of a delivery system for the stimulants was FDA-approved just a few years after the pump and pellet. It is a patch with an adhesive coating that is applied directly to the skin, such as on the back of your shoulder or on the buttocks. The patch contains MPH. When applied to the skin, the MPH is absorbed through the skin and gets into the bloodstream by that means. So long as you wear the patch, MPH is being delivered into the body for that many hours during the day. Because the stimulants can cause insomnia or trouble falling asleep, the patch needs to be removed several hours before bedtime to permit the drug left in the body to be broken down and removed without adversely affecting your sleep onset. Another problem is that 15%-20% of people experience a skin rash at the site of the patch and may need to stop using the patch for this reason.
This delivery system used to go by the brand name Daytrana® (MPH). But the patent on the device is up for sale and may be purchased by another company and renamed in the future. As with the drugs above, the patch comes in different doses to better adjust the amount of the drug to the individual.
- The Pro-Drug: In 2008, another delivery system received FDA approval, but only for use with adults with ADHD, and that system goes by the brand name of Vyvanse® (a form of AMP). Here is yet a further example of human inventiveness. One of the problems with the immediate-release pills as well as the pellet systems is that they have the potential to be abused. That is usually done by crushing and inhaling the powder from the pills or the crushed beads from the pellet systems. That powder can also be mixed with water and injected into a vein. Whether snorted through the nose or injected into a vein, the stimulants get into the blood very quickly and so into the brain very rapidly. It is this rapid invasion of the brain by the drug and nearly as rapid decrease in certain brain regions that creates the “rush” or euphoria that people can experience with stimulants delivered in this fashion. This does not occur from the oral ingestion of the drug. This pro-drug was designed so that the drug cannot be activated unless it is in the human stomach or intestines. The drug is designed in such a way that the d-AMP lasts 10–14 hours, typically – greatly reducing any abuse potential while providing for the desired longer course of action from a single dose.
- The Delayed Onset System: In 2019, the latest delivery system was approved, called Jornay PM, which comprises a reformulation of the drug MPH. This drug is taken at night typically between 6:30 and 9:30 p.m., and reliably activates 12 hours later. It is approved for people 6 years of age and older. But it is anticipated that the company will likely come out with a version that uses the drug AMP and seek FDA approval for use of that variant in children and adults with ADHD sometime in the near future. This product was developed because early morning hours can be very difficult for families of children with ADHD even if those children are taking one of the other stimulant delivery systems noted above. That is because it can take up to 60–90 minutes for those medications to reach their therapeutic level – a time period that overlaps with the hours parents and children are getting ready to leave home for school and work. Hence, children with ADHD on those other systems are essentially unmedicated or undermedicated for this crucial and stressful time of the weekday morning. This delivery system solves that problem.
- Liquid Extended Release: There are now liquid versions of the extended-release forms of MPH and AMP that may be helpful when clients profess difficulties swallowing the pills or capsules that are used in these other systems above.
- Dissolvable Gel “Gummy” Systems: Another formulation of MPH uses a gel product like that seen in gummy vitamins and candy. This gel dissolves on contact with saliva in the mouth and is not affected in its pharmacological properties if chewed by the child.
|
References (by major topic)
ADHD as a Disorder of Executive Functioning and Self-Regulation
American Psychiatric Association (1968). The diagnostic and statistical manual for mental disorders (2nd ed.). American Psychiatric Association.
Babinski, D. E. (2024). Sex differences in ADHD: Review and priorities for future research. Current Psychiatry Reports, 26, 151-156.
Barkley, R. A. (1997/2001). ADHD and the Nature of Self-Control (1st &2nd eds). Guilford Press.
Barkley, R. A. (2011). The Barkley Deficits in Executive Functioning Scale Guilford.
Barkley, R. A. (2012/2020 paperback). Executive functions: What they are, how they work, and why they evolved. Guilford Press.
Barkley, R. A. (2012b). The Barkley Deficits in Executive Functioning Scale – Children and Adolescents. Guilford.
Barkley, R. A. (2015). Emotional dysregulation is a core component of ADHD. In R. A. Barkley (Ed.). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 81-115). Guilford Press.
Barkley, R. A. (2019). Neuropsychological testing is not useful for the diagnosis of ADHD. Stop it! (or prove it). The ADHD Report, 27, 1-8.
Barkley, R. A. & Fischer, M. (2010). The unique contribution of emotional impulsiveness to impairment in major life activities in hyperactive children as adults. Journal of the American Academy of Child and Adolescent Psychiatry, 49, 503-513.
Barkley, R. A. & Murphy, K. R. (2011). Deficient emotional self-regulation in adults with ADHD: The relative contributions of emotional impulsiveness and ADHD symptoms to adaptive impairments in major life activities. Journal of ADHD and Related Disorders, 1(4), 5-28.
Brown, T. E. (2013). A new understanding of ADHD in children and adults: Executive function impairments. Routledge.
Brown, T. E. (2017). Outside the box: Rethinking ADD/ADHD in children and adults: A practical guide. American Psychiatric Association.
Castellanos, X., Sonuga-Barke, E., Milham, M., & Tannock, R. (2006). Characterizing cognition in ADHD: Beyond executive dysfunction. Trends in Cognitive Science, 10, 117-123.
Chacko, A., Merrill, B. M., Kofler, M. J., & Fabiano, G. A. (2024). Improving the efficacy and effectiveness of evidence-based psychosocial treatments for ADHD in children and adolescents. Translational Psychiatry, 14, 244.
Dawkins, R. (1982). The extended phenotype: the long reach of the gene. New York: Oxford University Press.
Douglas, V. I. (1980). Higher mental processes in hyperactive children: Implications for training. In R. Knights & D. Bakker (Eds.), Treatment of hyperactive and learning disordered children (pp. 65-92). University Park Press.
Douglas, V. I. (1988). Cognitive deficits in children with attention deficit disorder with hyperactivity. In L. Bloomingdale & J. Swanson (Eds.), Attention deficit disorder: Criteria, cognition, and intervention (pp. 65-82). Pergamon Press.
DuPaul, G. J., Evans, S. W., Cleminshaw-Mahan, C. L., & Fu, Q. (2024). School-based interventions for adolescents with ADHD: Predictors of effects on academic, behavioral, and social functioning. Behavior Therapy, 55(4), 680-697.
Faraone, S. V., Bellgrove, M. A., Brikell, I., Cortese, S., Hartman, C. A., Hollis, C., Newcorn, J. H., Philipsen, A., Polanczyk, G. V., Rubia, K., Sibley, M. H., & Buitelaar, J. K. (2024). Attention deficit/hyperactivity disorder. Nature Reviews: Disease Primers, 10(Article 11), 1-21. doi.org/10.1038/s41572-024-00495-0
Frazier, T. W., Demareem H. A., & Youngstrom, E. A. (2004). Meta-analysis of intellectual and neuropsychological test performance in attention-deficit/hyperactivity disorder. Neuropsychology, 18, 543-555.
Fuster, J. (1997). The Prefrontal Cortex. Raven Press.
Gallagher, R., & Wahba, S. (2024). Advances in the psychosocial treatment of ADHD in children and teens. Psychiatric Annals, 54(3), e88-e93.
Gross, J. J. (2007). Handbook of emotion regulation (pp. 3-24). Guilford Press.
Harlow, J. M. (1848). Passage of an iron rod through the head. Boston Medical and Surgical Journal, 39, 389-393.
Harlow, J. M. (1868). Recovery from the passage of an iron rod through the head. Publications of the Massachusetts Medical Society, Boston, 2, 237-346.
Hervey, A. S., Epstein, J. N., & Curry, J. F. (2004). Neuropsychology of adults with attention-deficit/hyperactivity disorder: A meta-analytic review. Neuropsychology, 18, 495-503.
Koziol, L. F. (2014). The myth of executive functioning: Missing elements in conceptualization, evaluation, and assessment. Springer.
Lalonde, M. A., Briese, R., Paris, A., & Kozy, B. J.(2025). Approaches to treating children with ADHD and common comorbidities. Journal of Pediatric health Care, January 10, 2025.
Marguet-Doleac, J., Biotteau, M., & Chaix, Y. (2023). Behavioral parent training for school-aged children with ADHD: A systematic review of randomized control trials. Journal of Attention Disorders, 28(3), 377-393.
Nigg, J. T., & Casey, B. (2005). An integrative theory of attention-deficit/hyperactivity disorder based on the cognitive and affective neurosciences. Development and Psychology, 17, 785-806.
Makris, N., Biederman, J., Monuteaux, M. C. & Seidman, L. J. (2009). Towards conceptualizing a neural systems-based anatomy of attention-deficit/hyperactivity disorder. Developmental Neurosciience, 31, 36-49.
McCrae, K., Ochsner, K. N. & Gross, J. J. (2011). The reason in passion. In K. Vohs and R. Baumeister (Eds.), Handbook of Self-Regulation (2nd ed.). Guilford Press.
O’Nions, E., El Baou, C., John, A., Lewer, D., Mandy, W., McKechnie, D. G. J., Petersen, I., & Stott, J. (2025). Life expectancy and years of life lost for adults diagnosed with ADHD in the UK: Matched cohort study. British Journal of Psychiatry. Doi: 10.1192/bjp.2024.199
Pievsky, M. A., & McGrath, R. E. (2017). The neurocognitive profile of attention deficit/hyperactivity disorder: A review of meta-analyses. Archives of Clinical Neuropsychology, 33, 143-157.
Popper, K. & Eccles, J. (1977). The self and its brain. London, England: Springer-Verlag.
Ramsay, J. R. & Rostain, A. L. (2014). Cognitive behavioral therapy for adult ADHD: An integrative psychosocial and medical approach. Routledge.
Ryckaert, C., Kuntsi, J., & Asherson, P. (2018). Emotional dysregulation and ADHD. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 103-117). London: Oxford University Press.
Shaw, P., Stringaris, A., Nigg, J., & Leibenluft, E. (2014). Emotion dysregulation in attention deficit hyperactivity disorder. American Journal of Psychiatry, 171(3), 276-293.
Solanto, M. (2013). Cognitive behavioral therapy for adult ADHD: Targeting executive dysfunction. Guilford Press.
Sagvolden, T., Johansen, E. B., Aase, H., & Russell, V. A. (2005). A dynamic developmental theory of attention-deficit/hyperactivity disorder (ADHD) predominantly hyperactive-impulsive and combined subtypes. Behavioral and Brain Sciences, 28, 397-408.
Solanto, M. V. (2015). Executive function deficits in adults with ADHD. In Barkley, R. A. (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 256-266). Guilford Publications.
Stuss, D. T. & Alexander, M. (2000). Executive functions and the frontal lobes: A conceptual view. Psychological Research, 63, 289-298.
Stuss, D. T. & Benson, D. F. (1986). The frontal lobes. Raven. Press.
Toplak, M. E., West, R. F., & Stanovich, K. E. (2013). Practitioner review: Do performance- based measures and ratings of executive function assess the same construct? Journal of Child Psychology and Psychiatry, 54, 131-143.
Weyandt, L. L. & Gudmundsdottir, B. G. (2015). Developmental and neuropsychological deficits in children with ADHD. In Barkley, R. A. (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 116-139.). Guilford Publications.
Willcutt, E. G. (2015). Theories of ADHD. In Barkley, R. A. (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 391-404). Guilford Publications.
Zylowska, L. & Mitchell, J. (2020). Mindfulness Based Practices for Adult ADHD. Guilford Publications.
Principles for Diagnosing ADHD
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
Barkley, R. A. (2011). Barkley Functional Impairment Scale. Guilford Press.
Barkley, R. A. (2012). Barkley Functional Impairment Scale – Children and Adolescents. Guilford Press.
Barkley, R. A. (2015) (ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). Guilford Press.
Barkley, R. A. (2015). History. In Attention Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment (4th ed.). Guilford Publications.
Barkley, R. A. (2015). Emotional dysregulation is a core component of ADHD. In R. A. Barkley (ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.)(pp. 81-115). Guilford Press.
Barkley, R. A. (2015). Executive functioning and self-regulation viewed as an extended phenotype: Implications of the theory for ADHD and its treatment. In R. A. Barkley (ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.)(pp. 405-434). Guilford Press.
Barkley, R. A. (2015). Concentration deficit disorder (Sluggish Cognitive Tempo). In R. A. Barkley (ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 435-454). Guilford Press.
Barkley, R. A. (2015). Health and related impairments in children and adults with ADHD. (pp. 267-313). And educational, occupational, dating and marital, and financial impairments. (pp. 314-342). In R. A. Barkley (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) Guilford Press.
Barkley, R. A., & Peters, H. (2012). The earliest reference to ADHD in the medical literature? Melchior Adam Weikard’s description in 1775 of “Attention Deficit” (Mangel der Aufmerksamkeit, attentio volubilis). Journal of Attention Disorders, 16, 623-630.
Barkley, R. A., Murphy, K. R., & Fischer, M. (2008). ADHD in adults: What the science says. Guilford Press.
Becker, S. P. & Barkley, R. A. (2018). Sluggish cognitive tempo. in Banaschewski, T., Coghill, D., & Zuddas, A. (2018). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 150-153). London: Oxford University Press.
Becker, S. P., Willcutt, E. G., Leopold, D. R., Fredrick, J. W., Smith, Z. R., Jacoson, L. A., Burns, G. L., Mayes, S. D., Waschbusch, D. A., Froehlich, T. E., McBurnett, K., Servera, M., & Barkley, R. A. (2022). Report of a work group on sluggish cognitive tempo: Key research directions and a consensus change in terminology to Cognitive Disengagement Hypoactivity Syndrome (CDHS). Journal of the American Academy of Child and Adolescent Psychiatry. Epub ahead of print.
Beery, M. S., Sweeney, M. M., Dolan, S. B., Johnson, P. S., Pennybaker, S. J., Rosch, K. S., & Johnson, M. W. (2020). Attention-deficit/hyperactivity disorder symptoms are associated with greater delay discounting of condom-protected sex and money. Archives of Sexual behavior. Epub ahead of print. doi: 10.1007/s10508-020-01698-8
Blue Cross Blue Shield Assoc. recorded rates of diagnosis USA Today, 4-8-2019
Faraone, S. C., Asherson, P., Banaschewski, T., Biederman, J., Buitelaar, J. K., Ramos-Quiroga, J. A., Rohde, L. A., Sonuga-Barke, E. J. S., Tannock, R., & Franke, B. (2015). Attention-deficit/hyperactivity disorder. Nature Reviews (Disease Primers), 1, 1-23.
Hechtman, L. (2016)(Ed.), Attention Deficit Hyperactivity Disorder: Adult Outcome and Its Predictors (pp. 63-104). New York: Oxford University Press.
Knouse, L. E. & Barkley, R. A. (2020). What’s in a (symptom example)? Exploring the Impact of DSM-5’s parenthetical additions on self-reporting of adult ADHD symptoms. Poster presentation at the annual meeting of APSARD, the American Professional Society for ADHD and Related Disorders. Washington, DC.
Polanczyk, G. V. (2018). Epidemiology. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 131-135). London: Oxford University Press.
Roberts, W., Milich, R., & Barkley, R. A. (2015). Primary symptoms, diagnostic criteria, subtyping, and prevalence of ADHD. In R. A. Barkley (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.)(pp. 51-80). Guilford Press.
Rohde, A., Kieling, C., & Salum, G. A. (2018). Current diagnostic criteria: DSM, ICD, and future perspectives. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 139-146). London: Oxford University Press.
Wakefield, J. C. (1999). Evolutionary versus prototype analyses of the concept of disorder. Journal of Abnormal Psychology, 108, 374-399.
Weikard, M. A. (1775). Drittes Hauptstück Mangel der Aufmerksamkeit Attentio volubilis in Der Philosophische Artzt (pp. 114-119). Frankfurt, Germany: Zmenter Band.
Willcutt, E. G. (2012). The prevalence of DSM-IV Attention-Deficit/Hyperactivity Disorder: A meta-Analysis Review. Neurotherapeutics, 9, 490-499.
Major Domains of Impairments
Adamou, M. (2018). Adult ADHD and employment. In Banaschewski, T., Coghill, D., & Zuddas, A. (2018). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 170-177). London: Oxford University Press.
Barkley, R. A. (2011). Barkley Functional Impairment Scale. Guilford Press.
Barkley, R. A. (2012). Barkley Functional Impairment Scale – Children and Adolescents. Guilford Press.
Barkley, R. A. (2012). Distinguishing sluggish cognitive tempo from attention-deficit/hyperactivity disorder in adults. Journal of Abnormal Psychology. 121(4), 978-990.
Barkley, R. A. (2013). Distinguishing sluggish cognitive tempo from ADHD in children and adolescents: Executive functioning, impairment, and comorbidity. Journal of Clinical Child and Adolescent Psychology, 42, 161-173.
Barkley, R. A. (2015). Educational, occupational, dating, and marital, and financial impairments in adults with ADHD. In R. A. Barkley (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 314-342.). Guilford Press.
Barkley, R. A. (2016). Managing ADHD in School. Eau Claire, WI: Premier Educational Seminars Inc.
Barkley, R. A. (2020). Taking Charge of Adult ADHD (3rd ed.). Guilford Press.
Barkley, R. A., Murphy, K. R., & Fischer, M. (2008). ADHD in adults: What the science says. Guilford Press.
DuPaul, G. J., & Stoner, G. (2014). ADHD in the schools: Assessment and intervention strategies (3rd ed.). Guilford Publications.
DuPaul, G. J. & Langberg, J. M. (2015). Educational impairments in children with ADHD. In Barkley, R. A. (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 169-190.). Guilford Publications.
Evans S. W., Van der Oord, S., & Rogers, E. E. (2020). Academic functioning and interventions for adolescents with ADHD. In. Becker, S. P. (Ed.), ADHD in adolescents: Development, assessment, and treatment (pp. 148-169). Guilford Publications.
Garner, A. A. (2020). Driving in adolescents with ADHD and the road to intervention. In. Becker, S. P. (Ed.), ADHD in adolescents: Development, assessment, and treatment (pp. 255-277). Guilford Publications.
Gordon, C. T., Fabiano, G. A., Hulme, K. F., Sodano, S. M., Adragna, M., Lim, R., Stanford, S., Janikowski, L., Bufalo, B., Rodriguez, Z., & Swiatek, D. (2020). Efficacy of lisdexamfetamine for promoting occupational success in adolescents and young adults with attention-deficit/hyperactivity disorder. Experimental and Clinical Psychopharmacology. Epub ahead of print. doi: 10.1037/pha0000365.
Gordon, M., & Keiser, S. (Eds.). (1998). Accommodations in higher education under the Americans with Disabilities Act (ADA): A no-nonsense guide for clinicians, educators, administrators, and lawyers. Guilford Press.
Hechtman, L. (2020). Attention deficit hyperactivity disorder: Adult outcome and its predictors. New York: Oxford University Press.
Johnston, C., & Chronis-Tuscano, A. (2015). Families and ADHD. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 191-209). Guilford Press.
Klein, K. R., & Sarkis, S. M. (2009). ADD and your money: A guide to personal finance for adults with attention-deficit disorder. New Harbinger.
Langberg, J. M. (2011). Homework, organization, and planning skills (HOPS) interventions. Bethesda, MD: National Association of School Psychologists.
Lewandowski, L. J., & Lovett, B. (2015). Testing accommodations for students with disabilities: Research-based practice. American Psychological Association.
McQuade, J. D. (2020). Peer functioning in adolescents with ADHD. In. Becker, S. P. (Ed.), ADHD in adolescents: Development, assessment, and treatment (pp. 128-147). Guilford Publications.
McQuade, J. D. & Hoza, B. (2015). Peer relationships of children with ADHD. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 210-222). Guilford Press.
Mikami, A.Y. (2015). Social skills training for youth with ADHD. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 569-595). Guilford Press.
Nadeau, K. G. (2007). Survival guide for college students with ADD or LD (2nd ed.). Magination Press.
Nadeau, K. G. (2015). The ADHD guide to career success (2nd ed.). Routledge.
Orlov, M. (2010). The ADHD effect on marriage: Understand and rebuild your relationship in six steps. Specialty Press.
Orlov, M. & Kohlenberg, N. (2014). The couples guide to thriving with ADHD. Specialty Press.
Pera, G. (2008). Is it you, me, or adult ADHD? 1201 Alarm Press.
Pera, G. (2015). Counseling couples affected by adult ADHD. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 795-825). Guilford Press.
Pera, G. (2016). Adult ADHD-focused couple therapy. Routledge.
Robin, A. R. & Payson, E. (2002). The impact of ADHD on marriage. The ADHD Report, 10(3), 9-11, 14.
Sibley, M. H. (2016). Parent-teen therapy for executive function deficits and ADHD: Building skills and motivation. Guilford Publications.
Tuckman, A. (2020). ADHD after dark: Better sex life, and better relationships. Routledge.
Weiner, J. (2020). The ripple effect of adolescent ADHD: Family relationships. In. Becker, S. P. (Ed.), ADHD in adolescents: Development, assessment, and treatment (pp. 101-127). Guilford Publications.
Assessment
Achenbach, T. M. (2014). The Achenbach System of Empirically Based Assessment (ASEBA). [Includes the Child Behavior Checklist] Author.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
Barkley, R. A. (2011). Barkley Adult ADHD Rating Scale-IV. Guilford Press.
Barkley, R. A. (2012a). Barkley Functional Impairment Scale – Children and Adolescents. Guilford Press.
Barkley, R. A. (2012b). Barkley Deficits in Executive Functioning Scale – Children and Adolescents. Guilford Press.
Barkley, R. A. (2013). Defiant children: A clinician’s manual for parent training (3rd ed.). Guilford Press.
Barkley, R. A. (2015). Attention-Deficit Hyperactivity Disorder: A handbook for diagnosis and treatment (4th ed.). Guilford Press.
Barkley, R. A. (2018). Barkley Sluggish Cognitive Tempo Scale – Children and Adolescents. Guilford Publications.
Barkley, R. A. (2019). Neuropsychological testing is not useful for the diagnosis of ADHD. Stop it! (or prove it). The ADHD Report, 27, 1-8.
Chronis-Tuscano, A., O’Brien, K. A., Johnston, C., Jones, H. A., Clarke, T. L., Raggi, V. L., Rooney, M. E., Diaz, Y., Pian, J., & Seymour, K. E. (2011). The relation between maternal ADHD symptoms & improvement in child behavior following brief behavioral parent training is mediated by change in negative parenting. Journal of Abnormal Child Psychology, 39, 1047-1057.
Chronis-Tuscano, A., Raggi, V. L., Clarke, T. L., Rooney, M. E., Diaz, Y., & Pian, J. (2008). Associations between maternal attention-deficit/hyperactivity disorder symptoms and parenting. Journal of Abnormal Child Psychology. 36, 1237-1250.
Chronis-Tuscano, A., Seymour, K. E., Stein, M. A., Jones, H. A., Jiles, C. D., Rooney, M. E., Conlon, C. J., Efron, L. A., Wagner, S. A., Pian, J., & Robb, A. S. (2008). Efficacy of osmotic-release oral system (OROS) methylphenidate for mothers with attention-deficit/hyperactivity disorder (ADHD): preliminary report of effects on ADHD symptoms and parenting. Journal of Clinical Psychiatry, 69, 1-10.
Danckaerts, M., & Coghill, D. (2018). Children and adolescents: Assessment in everyday clinical practice. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 297-306). London: Oxford University Press.
Derogatis, L. R. (1994). Manual for the Symptom Checklist 90—Revised (SCL-90-R). Indianapolis, IN: Pearson Assessments.
DuPaul, JG. J., Anastopoulos, A. D., & Kipperman, K. (2020). Assessing and diagnosing ADHD in adolescence. In S. P. Becker (Ed.), ADHD in adolescence (pp. 281-305). Guilford Publications.
DuPaul, G. J., Power, T. J., Anastopoulos, A. D., & Reid, R. (2016). The ADHD Rating Scale – 5: Checklists, norms, and clinical interpretation. Guilford Publications.
DuPaul, G. J., & Stoner, G. (2014). ADHD in the schools: Assessment and intervention strategies (3rd ed.). Guilford.
Gioia, G. A., Isquith, P. K., Guy, S. C., & Kenworthy, L. (2015). BRIEF-2: Behavior Rating Inventory of Executive Function – Professional Manual (2nd ed.). Psychological Assessment Resources, Inc.
Goldstein, S., & Naglieri, J. (2016). The Comprehensive Executive functioning Rating Scale. Multi-Health Systems.
Knouse, L. E. & Barkley, R. A. (2020). What’s in a (symptom example)? Exploring the Impact of DSM-5’s parenthetical additions on self-reporting of adult ADHD symptoms. Poster presentation at the annual meeting of APSARD, the American Professional Society for ADHD and Related Disorders. Washington, DC.
Mash, E. J., & Barkley, R. A. (Eds.). (2010). Assessment of Childhood Disorders (3rd ed.). Guilford Publications.
Mash, E. J., & Barkley, R. A. (Eds.). (2014). Child Psychopathology (3rd ed.). Guilford.
Pliszka, S. (2009). Treating ADHD and Comorbid Disorders. Guilford press.
Prinstein, M., Youngstrom, E. A., Mash, E. J. & Barkley, R. A. (Eds.) (2020) Treatment of childhood disorders. (pp.661-703). Guilford Publications.
Reynolds, C., & Kamphaus, R. (2015). Behavioral Assessment System for Children- 3. Pearson Assessments.
Shelton, T. L., Barkley, R. A., Crosswait, C., Moorehouse, M., Fletcher, K., Barrett S., Jenkins, L., & Metevia, L. (1998). Psychiatric and psychological morbidity as a function of adaptive disability in preschool children with aggressive and hyperactive-impulsive-inattentive behavior. Journal of Abnormal Child Psychology, 26, 475-494.
Sleator, E. K., & Ullmann, R. K. (1981). Can the physician diagnose hyperactivity in the office? Pediatrics, 67, 13–17.
Wahler, R. G. (1980). The insular mother: Her problems in parent–child treatment. Journal of Applied Behavior Analysis, 13, 207–219.
Parent Counseling and Behavior Management Training
Allan, C., & Chacko, A. (2018). Adverse events in behavioral parent training for children with ADHD: An under-appreciated phenomenon. The ADHD Report, 28(1), 4-8.
Antshel, K. M., & Olszewski, A. K. (2014). Cognitive behavioral therapy for adolescents with ADHD. Child and Adolescent Psychiatric Clinics of North America, 23, 825-842.
Arnold, E. A., Herbert, S. D., & Stowe, R. M. (2015). Parenting hyperactive preschoolers: Clinician guide. Oxford University Press.
Barkley, R.A. (2013). Defiant Children: A Clinician’s Manual for Assessment and Parent Training (3rd ed.). Guilford Publications.
Barkley, R. A. (2018a). Focus on the side effects of psychosocial treatments for children and teens with ADHD: A special issue. The ADHD Report, 26(1), 1-4.
Barkley, R. A. (2018b). Adverse events associated with behavior management training for families experiencing parent-ADHD teen conflict. The ADHD Report, 26(2), 1-6.
Barkley, R. A. (2020). Taking charge of ADHD: The complete authoritative guide for parents (5th ed.). Guilford Publications.
Barkley, R. A. (2021). 12 Principles for Raising a Child with ADHD. Guilford Publications.
Barkley R.A., Guevremont D.C., Anastopoulos A.D., & Fletcher, K. E. (1992). A comparison of three family therapy programs for treating family conflicts in adolescents with attention-deficit hyperactivity disorder. Journal of Consulting and Clinical Psychology, 60, 450–62.
Barkley, R.A., Robin, A. R., & Edwards, G. (2013). Defiant Teens: A Clinician’s Manual for Family Training (2nd ed.), Guilford Publications.
Becker, W. (1971). Parents are teachers. Research Press.
Bourchtein, E., & Langberg, J. M. (2018). Adverse events associated with implementing behavioral treatment with adolescents with ADHD. The ADHD Report, 28(2), 19-22.
Chacko, A., Allan, C. C., Uderman, J., Cornwell, M., Anderson, L., & Chimiklis, A. (2015). Training parents of youth with ADHD. In R. A.
Barkley (Ed.). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.)(pp. 513-536). Guilford Publications.
Chacko, A., Wymbs, B.T., Arnold, F.W., Pelham, W.E., Swanger-Gagne, M., Girio, E.L., Pirvics, L., Herbst, L., Guzzo, J.L., Phillips, C., & O’Connor, B. (2009). Enhancing traditional behavioral parent training for single-mothers of children with ADHD. Journal of Clinical Child and Adolescent Psychology, 38, 206-218.
Chacko, A., Wymbs, B.T., Chimiklis, A., Wymbs, F.A., & Pelham, W.E. (2012). Evaluating a comprehensive strategy to improve engagement to group-based behavioral parent training for high-risk families of children with ADHD. Journal of Abnormal Child Psychology, 40, 1351-1362.
Chronis, A.M., Chacko, A., Fabiano, G.A., Wymbs, B.T., & Pelham, W.E. (2004). Enhancements to the behavioral parent training paradigm for families of children with ADHD: Review and future directions. Clinical Child and Family Psychology Review, 7, 1-27.
Chronis, A. M., Lahey, B. B., Pelham, W. E., Williams, S. H., Baumann, B. L., Kipp, H., Jones, H. A., & Rathouz, P. J. (2007). Maternal depression and early positive parenting predict future conduct problems in young children with attention-deficit/hyperactivity disorder. Developmental Psychology, 43, 70–82.
Chronis-Tuscano, A., Clarke, T., O’Brien, K., Raggi, V., Diaz, Y., Mintz, A., Rooney, M., Knight, L., Seymour, K., Thomas, S., Seeley, J., Kosty, D., Lewinsohn, P. (2013). Development and preliminary evaluation of an integrated treatment targeting parenting and depressive symptoms in mothers of children with attention-deficit/hyperactivity disorder. Journal of Consulting Clinical Psychology, PubMed ID: 23477479
Chronis-Tuscano, A.M., & Stein, M. (2012). Pharmacotherapy for parents with attention-deficit hyperactivity disorder (ADHD): Impact on maternal ADHD and parenting. CNS Drugs, 26, 725-732.
Cunningham, C. E., Bremner, R., & Secord, M. (2006). COPE: The Community Parent Education Program: A School-Based Family Systems Oriented Workshop for Parents of Children with Disruptive Behavior Disorders. COPE Works
Daley, D., & Van der Oord, S. (2018). Behavioural interventions for preschool ADHD. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 333-339). London: Oxford University Press.
Davis, N. O., & Mitchell, J. T. (2020). Mindfulness meditation training for adolescents with ADHD. In. S. P. Becker (Ed.), ADHD in adolescents: development, assessment, and treatment (pp. 369-390). Guilford Publications.
Dopfner, M., & Van den Oord, S. (2018). Cognitive-behavioural treatment in childhood and adolescence. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 340-347). London: Oxford University Press.
Eisenstadt, T.H., Eyberg. S., McNeil. C.B., Newcomb, K., & Funderburk, B. (1993). Parent-child interaction therapy with behavior problem children: relative effectiveness of two stages and overall treatment outcome. Journal of Clinical Child Psychology, 22, 42-51.
Forgatch, M. & Patterson, G. (1989). Parents and adolescents living together: Part II, family problem solving. Castalia.
Garland, A. F., Hawley, K. M., Brookman-Frazee, L. I., & Hurlburt, M. (2008). Identifying common elements of evidence-based psychosocial treatments for children’s disruptive behavior problems. Journal of the American Academy of Child and Adolescent Psychiatry, 47, 505–514
Greene, R. W., & Ablon, J. S. (2006). Treating explosive kids: The collaborative problem-solving approach. Guilford Publications.
Guyer, B. P. (2000). ADHD: Achieving success in school and in life. Allyn & Bacon.
Ingoldsby, E. (2010). Review of interventions to improve family engagement and retention in parent and child mental health programs. Journal of Child and Family Studies, 19, 629-645.
Iseman, J. S., Silverman, S. M., & Jeweler, S. (2010). 101 school success tools for students with ADHD. Waco, TX: Prufrock Press. Kazdin, A. (2005). Parent management training: Treatment for oppositional, aggressive, amnd antisocial behavior in children and adolescents. New York, NY: Oxford University Press.
Langberg, J. M. (2011). Homework, organization and Planning Skills (HOPS) interventions: A treatment manual. National Association of School Psychologists Publications.
Langberg, J. M., Smith, Z. R., & Green, C. D. (2020). Addressing homework problems in adolescents with ADHD. In. S. P. Becker (Ed.), ADHD in adolescents: development, assessment, and treatment (pp. 330-349). Guilford Publications.
Lee, P., Niew, W., Yang, H., Chen, V., & Lin, K. (2012). A meta-analysis of behavioral parent training for children with attention deficit hyperactivity disorder. Research in Developmental Disabilities, 33, 2040-2049.
Lundahl, B., Risser, H.J., & Lovejoy, C. (2006). A meta-analysis of parent training: : Moderators and follow-up effects. Clinical Psychology Review, 26, 86-104.
McNeil, C.B., & Hembree-Kigin (2011). Parent-Child Interaction Therapy (2nd ed.) Springer.
Mikami, A. (2015). Social skills training for youth with ADHD. In R. A. Barkley (Ed.). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th. ed.)(pp. 569-595). Guilford Publications.
Mikami, A. (2018). Side effects of social skills training. The ADHD Report, 28(1), 13-18.
Robin, A. R. (2015). Training families of adolescents with ADHD. In R. A. Barkley (Ed.). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th. ed.)(pp. 537-568). Guilford Publications.
Robin, A. R. & Foster, S. L. (1989). Negotiating parent-adolescent conflict: A behavioral-family systems approach. Guilford Publications.
Sanders, M. (2012). Development, evaluation and multinational dissemination of the Triple P-Positive Parenting Program. Annual Review of Clinical Psychology, 8, 345-379.
Sibley, M. H. (2020). Motivational and executive functioning considerations when treating adolescents with ADHD. In. S. P. Becker (Ed.), ADHD in adolescents: development, assessment, and treatment (pp. 306-329). Guilford Publications.
Sprich, S. E. & Burbridge, J. A. (2020). Cognitive-behavioral therapy for adolescents with ADHD. In. S. P. Becker (Ed.), ADHD in adolescents: development, assessment, and treatment (pp. 350-368). Guilford Publications.
Sprich, S. & Safren, S. (2020). Overcoming ADHD in adolescence: A cognitive behavioral approach – therapist guide. Oxford University Press.
Sprich, S. E., Safren, S. A., Finkelstein, D., Remmert, J. E., & Hammerness, P. (2016). A randomized controlled trial of cognitive behavioral therapy for ADHD in medication-treated adolescents. Journal of Child Psycology and Psychiatry, 57(11), 1218-1226.
Thompson, M. J., Laver-Bradbury, C., Ayers, M., Le Poidevin, E., Mead, S., Dodds, C., Psychogiou, L., Bitsakou, P., Daley, D., Weeks, A., Brotman, L., Abikoff, H., Thompson, P., & Sonuga-Barke, E. J. S. (2009). A small scale randomized controlled trial of the revised New Forest parenting programme for preschoolers with attention-deficit hyperactivity disorder. European Child and Adolescent Psychiatry, 18(10), 605-616.
Webster-Stratton, C. (2006). Incredible Years Parenting Program. Incredible Years.
Stimulant and Nonstimulant Medications for ADHD, and Issues in Choosing Medications
Asherson, P. & Ramos-Quiroga, J. A. (2018). Treatment in adult ADHD. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 426-436). London: Oxford University Press.
Brown, T. E., Chen, J., & Robertson, B. (2020). Relationships between executive function improvement and ADHD symptom improvement with lisdexamfetamine dimesylate in adults with ADHD and executive function deficits: A post hoc analysis. Primary Care Companion for CNS Disorders, 22(3), pii: 19m02559.
Coghill, D., & Danckaerts, M. (2018). Oranizing and delivering treatment for ADHD. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 417-425). London: Oxford University Press.
Connor, D. F. (2015). Stimulant and nonstimulant medications for childhood ADHD. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 666-685). Guilford Publications.
Dittman, R. W., Hage, A., Pedraza, J. D., & Newcorn, J. H. (2018). Non-stimulants in the treatment of ADHD. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 393-401). London: Oxford University Press.
Frodl, F. T. & Skokauskas (2012). Meta-analysis of structural MRI studies in children and adults with attention deficit hyperactivity disorder indicates treatment effects. Acta Psychiatrica Scandinavica, 125, 114-126.
Ivanov, I., Murrough, J. W.., Bansal, R., Hao, X., & Peterson, B. S. (2014). Cerebellar morphology and the effects of stimulant medications in youths with attention deficit-hyperactivity disorder. Neuropsychopharmcology, 39(3), 718-726.
Li, L., Sujan, A. C., Butwicka, A., Chang, Z., Cortese, S., Quinn, P., Viktorin, A., Oberg, A. S., D’Onofrio, B. M., & Larsson, H. (2020). Associations of prescribed ADHD medication in pregnancy with pregnancy-related and offspring outcomes: A systematic review. CNS Drugs. Epub ahead of print. doi: 10.1007/s40263-020-00728-2.
Moreno-Alcazar, A., Ramos-Quiroga, J. A., Radua, J., Salavert, J., Bosch, P. G., Salvador, R., Blanch, J., Casas, M., McKenna, P. J., & Pomarol-Clotet, E. (2016). Brain abnormalities in adults with attention deficit hyperactivity disorder revealed by voxel-based morphometry. Psychiatry Research: Neuro-imaging, 254, 41-47.
Prince, J. B., Wilens, T. E., Spencer, T. J., & Biederman, J. (2015). Pharmacotherapy for ADHD in adults. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 826-865). Guilford Publications.
Shulz, K. P., Fan, J., Bedard, A. C., Clerkin, S. M., Ivanov, I., Tang, C. Y., Halperin, J. M., & Newcorn, J. H. (2012). Common and unique therapeutic mechanisms of stimulant and nonstimulant treatments for attention deficit hyperactivity disorder. Archives of Psychiatry, 69(9), 952-961.
Spencer, T. J., Brown, A., Seidman, L. J., Valera, E. M., Makris, N., Lomedico, A., Faraone, S. V., & Biederman, J. (2013). Effect of psychostimulants on brain structure and function in ADHD: A qualitative review of magnetic resonance imaging-based neuroimaging studies. Journal of Clinical Psychiatry, 74, 902-917.
Weyandt, L., Sweeney, C., & Thompson, L. (2020). The effectiveness of stimulant medication at improving executive functioning in adults with ADHD. The ADHD Report, 28(7), 1-6.
Wilens, Timothy E. and Hammerness, Paul G. (2016) Straight talk about psychiatric medications for kids, (4th ed.,) New York.
Zuddas, A., Banaschewski, T., Coghill, D., & Stein, M. A. (2018). ADHD treatment - psychostimulants. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 379-392). London: Oxford University Press.
School Management of ADHD
Barkley, R. A. (2016). Managing ADHD in school. Premier Educational Seminars, Inc.
Barkley, R. A. (2020). Taking charge of ADHD: The complete authoritative guide for parents (5th ed.). Guilford Publications.
Bowman-Perrott, L., Davis, H., Vannest, K., Williams, L., Greenwood, C., & Parker, R. (2013). Academic benefits of peer tutoring: A meta-analytic review of single-case research. School Psychology Review, 42, 39-55.
Charach, A., Carson, P., Fox, S., Usman Ali, M., Beckett, J., & Guan Lim, C. (2013). Preschool children at high risk for ADHD: A comparative effectiveness review. Pediatrics, 131, e1584-e1604.
Children and Adults with Attention-Deficit/Hyperactivity Disorder. (2006). The new CHADD information and resource guide to AD/HD. Landover, MD: Author.
Cooper, H., Robinson, J.C., Patall, E.A. (2006). Does homework improve academic achievement? A synthesis of research 1987-2003. Review of Educational Research, 76, 1-62.
DuPaul, G.J., Eckert, T.L., & Vilardo, B. (2012). The effects of school-based interventions for attention-deficit hyperactivity disorder: A meta-analysis 1996-2010. School Psychology Review, 41, 387-412.
DuPaul, G. J. & Langberg, J. M. (2015). Educational impairments in children with ADHD. In Barkley, R. A. (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 169-190.). Guilford Publications.
DuPaul, G. J., & Stoner, G. (2014). ADHD in the schools: Assessment and intervention strategies (3rd ed.). Guilford Publications.
Dush, D. M., Hirt, M. L., & Schroeder, H. E. (1989). Self-statement modification in the treatment of child behavior disorders: A meta-analysis. Psychological Bulletin, 106, 97–106.
Erchul, W.P., & Martens, B.K. (2010). School consultation: Conceptual and empirical bases of practice (3rd ed.). Springer.
Evans, S. W., Van der Oord, S., & Rogers, E. E. (2020). Academinc functioning and interventions for adolescents with ADHD. In. S. P. Becker (Ed.), ADHD in adolescents: development, assessment, and treatment (pp. 148-169). Guilford Publications.
Fabiano, G. A., Vujnovic, R. K., Pelham, W. E., Waschbusch, D. A., Massetti, G. M., Pariseau, M. E., Naylor, J., Yu, J., Robins, M., Cronefix, T., Greiner, A. R., & Volker, M. (2010). Enhancing the effectiveness of special education programming for children with attention deficit hyperactivity disorder using a daily report card. School Psychology Review, 39, 219-239.
Fowler, M. C. (2006). CHADD educator’s manual (2nd ed.). CHADD.
Gallagher, R., Abikoff, H. B., & Spira, E. G. (2014). Organizational skills training for children with ADHD: An empirically supported treatment. Guilford Press.
Gallagher, R., Spira, E. G., & Rosenblatt, J. L. (2018). The organized child: An effective program to maximize your kid’s potential—in school and in life Guilford Press.
Greenwood, C. R., Maheady, L., & Delquadri, J. (2002). Classwide peer tutoring programs. In M. R. Shinn, H. M. Walker, & G. Stoner (Eds.), Interventions for academic and behavior problems II: Preventive and remedial approaches (pp. 611–650). National Association of School Psychologists.
McGoey, K. E., & DuPaul, G. J. (2000). Token reinforcement and response cost procedures: Reducing the disruptive behavior of preschool children with ADHD. School Psychology Quarterly, 15, 330–343.
McGoey, K. E., Eckert, T. L., & DuPaul, G. J. (2002). Early intervention for preschool-age children with ADHD: A literature review. Journal of Emotional and Behavioral Disorders, 10, 14–28.
Meltzer, L. (2010). Promoting executive function in the classroom. Guilford Press.
Merrell, C., & Sayal, K. (2018). ADHD and school. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 408-4413). London: Oxford University Press.
Miller, F. G. & Lee, D.L. (2013). Do functional behavioral assessments improve intervention effectiveness for students diagnosed with ADHD? A single-subject meta-analysis. Journal of Behavioral Education 22, 253-282.
Nelson, J.R., Benner, G.J., & Mooney, P. (2008). Instructional practices for students with behavioral disorders: Strategies for reading, writing, and math. Guilford.
Pfiffner, L. (2011). All about ADHD: The complete practical guide for classroom teachers. Teaching Resources.
Pfiffner, L. J., & DuPaul, G. J. (2015). Treatment of ADHD in school settings. In R. A. Barkley (Ed.). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th. ed.)(pp. 596-640). Guilford Publications.
Pfiffner, L. J., & DuPaul, G. J. (2018). Possible adverse side effects of school behavioral interventions. The ADHD Report, 28(1), 10-13.
Pfiffner, L.J., Villodas, M., Kaiser, N., Rooney, M., & McBurnett, K. (2013). Educational outcomes of a collaborative school-home behavioral intervention for ADHD. School Psychology Quarterly, 28, 25-36.
Power, T. J., Karustis, J. L., & Habboushe, D. F. (2001). Homework success for children with ADHD: A family–school intervention program. Guilford Press.
Saline, S., & Markham, L. (2018). What your ADHD child wishes you knew: Working together to empower kids for success in school and life. TarcherPerigee (Penguin Books).
Silverman, S. M., Iseman, J. S., & Jeweler, S. (2009). School success for kids with ADHD. Prufrock Press.
Zirkel, P.A. (2013). ADHD checklist for identification under the IDEA and Section 504/ADA. Education Law Reporter, 293(1), 13-27.
Unproven and Disproven Treatments
Bader, A., & Adesman, A. (2015). Complementary and alternative medicine for ADHD. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 728-738). Guilford Publications.
Buitelaar, J., Rommelse, N., Ly, V., & Rucklidge, J. (2018). Nutritional intervention for ADHD. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 373-378). London: Oxford University Press.
Cortese, S., Ferrin, M., Braindeis, D., Holtman, M., Aggensteiner, P., Daley, D., Santosh, PSimonoff, E., Sevenson, J., Stingaris, A., Sonuga-Barke, E. J. S. and the European ADHD Guidelines Group (2016). Neurofeedback for attention-deficit/hyperactivity disorder: Meta-analysis of clinical and neuropsychological outcomes from randomized controlled trials. Journal of the American Academy of Child and Adolescent Psychiatry, 55, 444-455.
Holtmann, M., Albrecht, B., & Brandeis, D. (2018). Neurofeedback. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 366-372). London: Oxford University Press.
Hurt, E. & Arnold, L. E. (2015). Dietary management of ADHD. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 631-640). Guilford Publications.
McGough, J. J., Sturm, A., Cowen, J., Tung, K., Salgari, G. C., Leuchter, A. F., Cook, I. A., Sugar, C. A., & Loo, S. K. (2019). Double-blind, sham-controlled, pilot study of trigeminal nerve stimulant for attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 58(4), 403-411.
Nigg, J. T. (2017). Getting ahead of ADHD: What next generation science says about treatments that work—and how you can make them work for your child. Guilford Publications.
Nigg, J.T., Lewis, K., Edinger, T., & Falk, M. (2012). Meta-analysis of Attention-Deficit/Hyperactivity Disorder or Attention-Deficit Disorder symptoms, restriction diet, and synthetic food color analysis. Journal of the American Academy of Child and Adolescent Psychiatry, 51, 86-97.
Rapport, M. D., Orban, S. A., Kofler, M. J., Friedman, L. M., & Bolden, J. (2015). Executive function training for children with ADHD. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 641-665). Guilford Publications.
Sonuga-Barke, E.J. S., Brandeis, D., Cortese, S., Daley, D., & Ferrin, M. (2013). European ADHD Guidelines Group Nonpharmacological intervention for ADHD: systematic review and meta-analyses of randomized controlled trials of dietary and psychological treatments. American Journal of Psychiatry, 170, 275-289.
Sonuga-Barke, E. J. S. & Cortese, S. (2018). Cognitive training approaches for ADHD: Can they be made more effective? In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.).
Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 358-365.). London: Oxford University Press.
Principles for Diagnosing ADHD
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
Barkley, R. A. (2011). Barkley Functional Impairment Scale. Guilford Press.
Barkley, R. A. (2012). Barkley Functional Impairment Scale – Children and Adolescents. New York: Guilford Press.
Barkley, R. A. (Ed.) (2015) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). Guilford Press.
Barkley, R. A. (2015). History. In Attention Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment (4th ed.). Guilford Publications.
Barkley, R. A. (2015). Emotional dysregulation is a core component of ADHD. In R. A. Barkley (ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed,)(pp. 81-115). Guilford Press.
Barkley, R. A. (2015). Executive functioning and self-regulation viewed as an extended phenotype: Implications of the theory for ADHD and its treatment. In R. A. Barkley (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed,) pp. 405-434). Guilford Press.
Barkley, R. A. (2015). Concentration deficit disorder (Sluggish Cognitive Tempo). In R. A. Barkley (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed,)(pp. 435-454). Guilford Press.
Barkley, R. A. (2015). Health and related impairments in children and adults with ADHD. (pp. 267-313). And Educational, occupational, dating and marital, and financial impairments. (pp. 314-342). In R. A. Barkley (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed,) Guilford Press.
Barkley, R. A., & Peters, H. (2012). The earliest reference to ADHD in the medical literature? Melchior Adam Weikard’s description in 1775 of “Attention Deficit” (Mangel der Aufmerksamkeit, attentio volubilis). Journal of Attention Disorders, 16, 623-630.
Barkley, R. A., Murphy, K. R., & Fischer, M. (2008). ADHD in adults: What the science says. Guilford Press.
Becker, S. P. & Barkley, R. A. (2018). Sluggish cognitive tempo. in Banaschewski, T., Coghill, D., & Zuddas, A. (2018). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 150-153). London: Oxford University Press.
Becker, S. P., Willcutt, E. G., Leopold, D. R., Fredrick, J. W., Smith, Z. R., Jacoson, L. A., Burns, G. L., Mayes, S. D., Waschbusch, D. A., Froehlich, T. E., McBurnett, K., Servera, M., & Barkley, R. A. (2022). Report of a work group on sluggish cognitive tempo: Key research directions and a consensus change in terminology to Cognitive Disengagement Hypoactivity Syndrome (CDHS). Journal of the American Academy of Child and Adolescent Psychiatry. Epub ahead of print.
Beery, M. S., Sweeney, M. M., Dolan, S. B., Johnson, P. S., Pennybaker, S. J., Rosch, K. S., & Johnson, M. W. (2020). Attention-deficit/hyperactivity disorder symptoms are associated with greater delay discounting of condom-protected sex and money. Archives of Sexual behavior. Epub ahead of print. doi: 10.1007/s10508-020-01698-8
Blue Cross Blue Shield Assoc. recorded rates of diagnosis USA Today, 4-8-2019
Faraone, S. C., Asherson, P., Banaschewski, T., Biederman, J., Buitelaar, J. K., Ramos-Quiroga, J. A. Rohde, L. A., Sonuga-Barke, E. J. S., Tannock, R., & Franke, B. (2015). Attention-deficit/hyperactivity disorder. Nature Reviews (Disease Primers), 1, 1-23.
Hechtman, L. (Ed.) (2016), Attention Deficit Hyperactivity Disorder: Adult Outcome and Its Predictors (pp. 63-104). New York: Oxford University Press.
Knouse, L. E. & Barkley, R. A. (2020). What’s in a (symptom example)? Exploring the Impact of DSM-5’s parenthetical additions on self-reporting of adult ADHD symptoms. Poster presentation at the annual meeting of APSARD, the American Professional Society for ADHD and Related Disorders. Washington, DC.
Polanczyk, G. V. (2018). Epidemiology. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 131-135). London: Oxford University Press.
Roberts, W., Milich, R., & Barkley, R. A. (2015). Primary symptoms, diagnostic criteria, subtyping, and prevalence of ADHD. In R. A. Barkley (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 51-80). Guilford Press.
Rohde, A., Kieling, C., & Salum, G. A. (2018). Current diagnostic criteria: DSM, ICD, and future perspectives. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 139-146). London: Oxford University Press.
Wakefield, J. C. (1999). Evolutionary versus prototype analyses of the concept of disorder. Journal of Abnormal Psychology, 108, 374-399.
Weikard, M. A. (1775). Drittes Hauptstück Mangel der Aufmerksamkeit Attentio volubilis in Der Philosophische Artzt (pp. 114-119). Frankfurt, Germany: Zmenter Band.
Willcutt, E. G. (2012). The prevalence of DSM-IV Attention-Deficit/Hyperactivity Disorder: A meta-Analysis Review. Neurotherapeutics, 9, 490-499.
Major Domains of Impairments
Adamou, M. (2018). Adult ADHD and employment. In Banaschewski, T., Coghill, D., & Zuddas, A. (2018). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 170-177). London: Oxford University Press.
Barkley, R. A. (2011). Barkley Functional Impairment Scale. Guilford Press.
Barkley, R. A. (2012). Barkley Functional Impairment Scale – Children and Adolescents. New York: Guilford Press.
Barkley, R. A. (2012). Distinguishing sluggish cognitive tempo from attention-deficit/hyperactivity disorder in adults. Journal of Abnormal Psychology. 121(4), 978-990.
Barkley, R. A. (2013). Distinguishing sluggish cognitive tempo from ADHD in children and adolescents: Executive functioning, impairment, and comorbidity. Journal of Clinical Child and Adolescent Psychology, 42, 161-173.
Barkley, R. A. (2015). Educational, occupational, dating, and marital, and financial impairments in adults with ADHD. In R. A. Barkley (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.)(pp. 314-342.). Guilford Press.
Barkley, R. A. (2016). Managing ADHD in School. Premier Educational Seminars Inc.
Barkley, R. A. (2020). Taking Charge of Adult ADHD (3rd ed.). Guilford Press.
Barkley, R. A., Murphy, K. R., & Fischer, M. (2008). ADHD in adults: What the science says. Guilford Press.
DuPaul, G. J., & Stoner, G. (2014). ADHD in the schools: Assessment and intervention strategies (3rd ed.). Guilford Publications.
DuPaul, G. J. & Langberg, J. M. (2015). Educational impairments in children with ADHD. In Barkley, R. A. (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 169-190.). Guilford Publications.
Evans S. W.,Van der Oord, S., & Rogers, E. E. (2020). Academic functioning and interventions for adolescents with ADHD. In. Becker, S. P. (Ed.), ADHD in adolescents: Development, assessment, and treatment (pp. 148-169). Guilford Publications.
Garner, A. A. (2020). Driving in adolescents with ADHD and the road to intervention. In. Becker, S. P. (Ed.), ADHD in adolescents: Development, assessment, and treatment (pp. 255-277). Guilford Publications.
Gordon, C. T., Fabiano, G. A., Hulme, K. F., Sodano, S. M., Adragna, M., Lim, R., Stanford, S., Janikowski, L., Bufalo, B., Rodriguez, Z., & Swiatek, D. (2020). Efficacy of lisdexamfetamine for promoting occupational success in adolescents and young adults with attention-deficit/hyperactivity disorder. Experimental and Clinical Psychopharmacology. Epub ahead of print. doi: 10.1037/pha0000365.
Gordon, M., & Keiser, S. (Eds.). (1998). Accommodations in higher education under the Americans with Disabilities Act (ADA): A no-nonsense guide for clinicians, educators, administrators, and lawyers. Guilford Press.
Hechtman, L. (2020). Attention deficit hyperactivity disorder: Adult outcome and its predictors. New York: Oxford University Press. Johnston, C., & Chronis-Tuscano, A. (2015). Families and ADHD. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 191-209). Guilford Press.
Klein, K. R., & Sarkis, S. M. (2009). ADD and your money: A guide to personal finance for adults with attention-deficit disorder. New Harbinger.
Langberg, J. M. (2011). Homework, organization, and planning skills (HOPS) interventions. National Association of School Psychologists.
Lewandowski, L. J., & Lovett, B. (2015). Testing accommodations for students with disabilities: Research-based practice. American Psychological Association.
McQuade, J. D. (2020). Peer functioning in adolescents with ADHD. In. Becker, S. P. (Ed.), ADHD in adolescents: Development, assessment, and treatment (pp. 128-147). Guilford Publications.
McQuade, J. D. & Hoza, B. (2015). Peer relationships of children with ADHD. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 210-222). Guilford Press.
Mikami, A.Y. (2015). Social skills training for youth with ADHD. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 569-595). Guilford Press.
Nadeau, K. G. (2007). Survival guide for college students with ADD or LD (2nd ed.). Magination Press.
Nadeau, K. G. (2015). The ADHD guide to career success (2nd ed.). Routledge.
Orlov, M. (2010). The ADHD effect on marriage: Understand and rebuild your relationship in six steps. Specialty Press.
Orlov, M. & Kohlenberg, N. (2014). The couples guide to thriving with ADHD. Specialty Press.
Pera, G. (2008). Is it you, me, or adult ADHD? 1201 Alarm Press.
Pera, G. (2015). Counseling couples affected by adult ADHD. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 795-825). Guilford Press.
Pera, G. (2016). Adult ADHD-focused couple therapy. Routledge.
Robin, A. R. & Payson, E. (2002). The impact of ADHD on marriage. The ADHD Report, 10(3), 9-11, 14.
Sibley, M. H. (2016). Parent-teen therapy for executive function deficits and ADHD: Building skills and motivation. Guilford Publications.
Tuckman, A. (2020). ADHD after dark: Better sex life, and better relationships. Routledge.
Weiner, J. (2020). The ripple effect of adolescent ADHD: Family relationshis. In. Becker, S. P. (Ed.), ADHD in adolescents: Development, assessment, and treatment (pp. 101-127). Guilford Publications.
Assessment
Achenbach, T. M. (2014). The Achenbach System of Empirically Based Assessment (ASEBA). [Includes the Child Behavior Checklist] Burlington, VT: Author.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). Washington, DC: Author.
Barkley, R. A. (2011). Barkley Adult ADHD Rating Scale-IV. Guilford Press.
Barkley, R. A. (2012a). Barkley Functional Impairment Scale – Children and Adolescents. Guilford Press.
Barkley, R. A. (2012b). Barkley Deficits in Executive Functioning Scale – Children and Adolescents. Guilford Press.
Barkley, R. A. (2013). Defiant children: A clinician’s manual for parent training (3rd ed.). Guilford Press.
Barkley, R. A. (2015). Attention-Deficit Hyperactivity Disorder: A handbook for diagnosis and treatment (4th ed.). Guilford Press.
Barkley, R. A. (2018). Barkley Sluggish Cognitive Tempo Scale – Children and Adolescents. Guilford Publications.
Barkley, R. A. (2019). Neuropsychological testing is not useful for the diagnosis of ADHD. Stop it! (or prove it). The ADHD Report, 27, 1-8.
Chronis-Tuscano, A., O’Brien, K. A., Johnston, C., Jones, H. A., Clarke, T. L., Raggi, V. L., Rooney, M. E., Diaz, Y., Pian, J., & Seymour, K. E. (2011). The relation between maternal ADHD symptoms & improvement in child behavior following brief behavioral parent training is mediated by change in negative parenting. Journal of Abnormal Child Psychology, 39, 1047-1057.
Chronis-Tuscano, A., Raggi, V. L., Clarke, T. L., Rooney, M. E., Diaz, Y., & Pian, J. (2008). Associations between maternal attention-deficit/hyperactivity disorder symptoms and parenting. Journal of Abnormal Child Psychology. 36, 1237-1250.
Chronis-Tuscano, A., Seymour, K. E., Stein, M. A., Jones, H. A., Jiles, C. D., Rooney, M. E., Conlon, C. J., Efron, L. A., Wagner, S. A., Pian, J., & Robb, A. S. (2008). Efficacy of osmotic-release oral system (OROS) methylphenidate for mothers with attention-deficit/hyperactivity disorder (ADHD): preliminary report of effects on ADHD symptoms and parenting. Journal of Clinical Psychiatry, 69, 1-10.
Danckaerts, M., & Coghill, D. (2018). Children and adolescents: Assessment in everyday clinical practice. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 297-306). London: Oxford University Press.
Derogatis, L. R. (1994). Manual for the Symptom Checklist 90—Revised (SCL-90-R). Pearson Assessments.
DuPaul, J. G. J., Anastopoulos, A. D., & Kipperman, K. (2020). Assessing and diagnosing ADHD in adolescence. In S. P. Becker (Ed.), ADHD in adolescence (pp. 281-305). Guilford Publications.
DuPaul, G. J., Power, T. J., Anastopoulos, A. D., & Reid, R. (2016). The ADHD Rating Scale – 5: Checklists, norms, and clinical interpretation. Guilford Publications.
DuPaul, G. J., & Stoner, G. (2014). ADHD in the schools: Assessment and intervention strategies (3rd ed.). Guilford.
Gioia, G. A., Isquith, P. K., Guy, S. C., & Kenworthy, L. (2015). BRIEF-2: Behavior Rating Inventory of Executive Function – Professional Manual (2nd ed.). Psychological Assessment Resources, Inc.
Goldstein, S., & Naglieri, J. (2016). The Comprehensive Executive functioning Rating Scale. Multi-Health Systems.
Knouse, L. E. & Barkley, R. A. (2020). What’s in a (symptom example)? Exploring the Impact of DSM-5’s parenthetical additions on self-reporting of adult ADHD symptoms. Poster presentation at the annual meeting of APSARD, the American Professional Society for ADHD and Related Disorders. Washington, DC.
Mash, E. J., & Barkley, R. A. (Eds.). (2010). Assessment of Childhood Disorders (3rd ed.). Guilford Publications.
Mash, E. J., & Barkley, R. A. (Eds.). (2014). Child Psychopathology (3rd ed.). Guilford.
Pliszka, S. (2009). Treating ADHD and Comorbid Disorders. Guilford press.
Prinstein, M., Youngstrom, E. A., Mash, E. J. & Barkley, R. A. (Eds.) (2020). Treatment of childhood disorders (pp.661-703). Guilford Publications.
Reynolds, C., & Kamphaus, R. (2015). Behavioral Assessment System for Children- 3. Indianapolis, IN: Pearson Assessments.
Shelton, T. L., Barkley, R. A., Crosswait, C., Moorehouse, M., Fletcher, K., Barrett S., Jenkins, L., & Metevia, L. (1998). Psychiatric and psychological morbidity as a function of adaptive disability in preschool children with aggressive and hyperactive-impulsive-inattentive behavior. Journal of Abnormal Child Psychology, 26, 475-494.
Sleator, E. K., & Ullmann, R. K. (1981). Can the physician diagnose hyperactivity in the office? Pediatrics, 67, 13–17.
Wahler, R. G. (1980). The insular mother: Her problems in parent–child treatment. Journal of Applied Behavior Analysis, 13, 207–219.
Parent Counseling and Behavior Management Training
Allan, C., & Chacko, A. (2018). Adverse events in behavioral parent training for children with ADHD: An under-appreciated phenomenon. The ADHD Report, 28(1), 4-8.
Antshel, K. M., & Olszewski, A. K. (2014). Cognitive behavioral therapy for adolescents with ADHD. Child and Adolescent Psychiatric Clinics of North America, 23, 825-842.
Arnold, E. A., Herbert, S. D., & Stowe, R. M. (2015). Parenting hyperactive preschoolers: Clinician guide. New York: Oxford University Press.
Barkley, R.A. (2013). Defiant Children: A Clinician’s Manual for Assessment and Parent Training (3rd ed.), Guilford Publications.
Barkley, R. A. (2018a). Focus on the side effects of psychosocial treatments for children and teens with ADHD: A special issue. The ADHD Report, 26(1), 1-4.
Barkley, R. A. (2018b). Adverse events associated wit behavior management training for families experiencing parent-ADHD teen conflict. The ADHD Report, 26(2), 1-6.
Barkley, R. A. (2020). Taking charge of ADHD: The complete authoritative guide for parents (5th ed.). Guilford Publications.
Barkley, R. A. (2021). 12 Principles for Raising a Child with ADHD. Guilford Publications.
Barkley R.A., Guevremont D.C., Anastopoulos A.D., & Fletcher, K. E. (1992). A comparison of three family therapy programs for treating family conflicts in adolescents with attention-deficit hyperactivity disorder. Journal of Consulting and Clinical Psychology, 60, 450–62.
Barkley, R.A., Robin, A. R., & Edwards, G. (2013). Defiant Teens: A Clinician’s Manual for Family Training (2nd ed.), Guilford Publications.
Becker, W. (1971). Parents are teachers. Research Press.
Bourchtein, E., & Langberg, J. M. (2018). Adverse events associated with implementing behavioral treatment with adolescents with ADHD. The ADHD Report, 28(2), 19-22.
Chacko, A., Allan, C. C., Uderman, J., Cornwell, M., Anderson, L., & Chimiklis, A. (2015). Training parents of youth with ADHD. In R. A. Barkley (Ed.). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th. ed.)(pp. 513-536). New York: Guilford Publications.
Chacko, A., Wymbs, B.T., Arnold, F.W., Pelham, W.E., Swanger-Gagne, M., Girio, E.L., Pirvics, L., Herbst, L., Guzzo, J.L., Phillips, C., & O’Connor, B. (2009). Enhancing traditional behavioral parent training for single-mothers of children with ADHD. Journal of Clinical Child and Adolescent Psychology, 38, 206-218.
Chacko, A., Wymbs, B.T., Chimiklis, A., Wymbs, F.A., & Pelham, W.E. (2012). Evaluating a comprehensive strategy to improve engagement to group-based behavioral parent training for high-risk families of children with ADHD. Journal of Abnormal Child Psychology, 40, 1351-1362.
Chronis, A.M., Chacko, A., Fabiano, G.A., Wymbs, B.T., & Pelham, W.E. (2004). Enhancements to the behavioral parent training paradigm for families of children with ADHD: Review and future directions. Clinical Child and Family Psychology Review, 7, 1-27.
Chronis, A. M., Lahey, B. B., Pelham, W. E., Williams, S. H., Baumann, B. L., Kipp, H., Jones, H. A., & Rathouz, P. J. (2007). Maternal depression and early positive parenting predict future conduct problems in young children with attention-deficit/hyperactivity disorder. Developmental Psychology, 43, 70–82.
Chronis-Tuscano, A., Clarke, T., O’Brien, K., Raggi, V., Diaz, Y., Mintz, A., Rooney, M., Knight, L., Seymour, K., Thomas, S., Seeley, J., Kosty, D., Lewinsohn, P. (2013). Development and preliminary evaluation of an integrated treatment targeting parenting and depressive symptoms in mothers of children with attention-deficit/hyperactivity disorder. Journal of Consulting Clinical Psychology, PubMed ID: 23477479
Chronis-Tuscano, A.M., & Stein, M. (2012). Pharmacotherapy for parents with attention-deficit hyperactivity disorder (ADHD): Impact on maternal ADHD and parenting. CNS Drugs, 26, 725-732.
Cunningham, C. E., Bremner, R., & Secord, M. (2006). COPE: The Community Parent Education Program: A School-Based Family Systems Oriented Workshop for Parents of Children with Disruptive Behavior Disorders. Hamilton, Ontario: COPE Works
Daley, D., & Van der Oord, S. (2018). Behavioural interventions for preschool ADHD. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 333-339). London: Oxford University Press.
Davis, N. O., & Mitchell, J. T. (2020). Mindfulness meditation training for adolescents with ADHD. In. S. P. Becker (Ed.), ADHD in adolescents: Development, assessment, and treatment (pp. 369-390). Guilford Publications.
Dopfner, M., & Van den Oord, S. (2018). Cognitive-behavioural treatment in childhood and adolescence. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 340-347). London: Oxford University Press.
Eisenstadt, T.H., Eyberg. S., McNeil. C.B., Newcomb, K., & Funderburk, B. (1993). Parent-child interaction therapy with behavior problem children: relative effectiveness of two stages and overall treatment outcome. Journal of Clinical Child Psychology, 22, 42-51.
Forgatch, M. & Patterson, G. (1989). Parents and adolescents living together: Part II, family problem solving. Eugene, OR: Castalia.
Garland, A. F., Hawley, K. M., Brookman-Frazee, L. I., & Hurlburt, M. (2008). Identifying common elements of evidence-based psychosocial treatments for children’s disruptive behavior problems. Journal of the American Academy of Child and Adolescent Psychiatry, 47, 505–514
Greene, R. W., & Ablon, J. S. (2006). Treating explosive kids: The collaborative problem-solving approach. Guilford Publications.
Guyer, B. P. (2000). ADHD: Achieving success in school and in life. Allyn & Bacon.
Ingoldsby, E. (2010). Review of interventions to improve family engagement and retention in parent and child mental health programs. Journal of Child and Family Studies, 19, 629-645.
Iseman, J. S., Silverman, S. M., & Jeweler, S. (2010). 101 school success tools for students with ADHD. Prufrock Press.
Kazdin, A. (2005). Parent management training: Treatment for oppositional, aggressive, and antisocial behavior in children and adolescents. New York, NY: Oxford University Press.
Langberg, J. M. (2011). Homework, organization and Planning Skills (HOPS) interventions: A treatment manual. National Association of School Psychologists Publications.
Langberg, J. M., Smith, Z. R., & Green, C. D. (2020). Addressing homework problems in adolescents with ADHD. In. S. P. Becker (Ed.), ADHD in adolescents: development, assessment, and treatment (pp. 330-349). Guilford Publications.
Lee, P., Niew, W., Yang, H., Chen, V., & Lin, K. (2012). A meta-analysis of behavioral parent training for children with attention deficit hyperactivity disorder. Research in Developmental Disabilities, 33, 2040-2049.
Lundahl, B., Risser, H.J., & Lovejoy, C. (2006). A meta-analysis of parent training: : Moderators and follow-up effects. Clinical Psychology Review, 26, 86-104.
McNeil, C.B., & Hembree-Kigin (2011). Parent-Child Interaction Therapy (2nd ed.) Springer.
Mikami, A. (2015). Social skills training for youth with ADHD. In R. A. Barkley (Ed.). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th. ed.)(pp. 569-595). Guilford Publications.
Mikami, A. (2018). Side effects of social skills training. The ADHD Report, 28(1), 13-18.
Robin, A. R. (2015). Training families of adolescents with ADHD. In R. A. Barkley (Ed.). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th. ed.) (pp. 537-568). Guilford Publications.
Robin, A. R. & Foster, S. L. (1989). Negotiating parent-adolescent conflict: A behavioral-family systems approach. Guilford Publications.
Sanders, M. (2012). Development, evaluation and multinational dissemination of the Triple P-Positive Parenting Program. Annual Review of Clinical Psychology, 8, 345-379.
Sibley, M. H. (2020). Motivational and executive functioning considerations when treating adolescents with ADHD. In. S. P. Becker (Ed.), ADHD in adolescents: development, assessment, and treatment (pp. 306-329). Guilford Publications.
Sprich, S. E. & Burbridge, J. A. (2020). Cognitive-behavioral therapy for adolescents with ADHD. In. S. P. Becker (Ed.), ADHD in adolescents: development, assessment, and treatment (pp. 350-368). Guilford Publications.
Sprich, S. & Safren, S. (2020). Overcoming ADHD in adolescence: A cognitive behavioral approach – therapist guide. New York: Oxford University Press.
Sprich, S. E., Safren, S. A., Finkelstein, D., Remmert, J. E., & Hammerness, P. (2016). A randomized controlled trial of cognitive behavioral therapy for ADHD in medication-treated adolescents. Journal of Child Psycology and Psychiatry, 57(11), 1218-1226.
Thompson, M. J., Laver-Bradbury, C., Ayers, M., Le Poidevin, E., Mead, S., Dodds, C. Psychogiou, L., Bitsakou, P., Daley, D., Weeks, A., Brotman, L., Abikoff, H., Thompson, P., & Sonuga-Barke, E. J. S (2009). A small scale randomized controlled trial of the revised New Forest parenting programme for preschoolers with attention-deficit hyperactivity disorder. European Child and Adolescent Psychiatry, 18(10), 605-616.
Webster-Stratton, C. (2006). Incredible Years Parenting Program. Incredible Years.
Stimulant and Nonstimulant Medications for ADHD, and Issues in Choosing Medications
Asherson, P. & Ramos-Quiroga, J. A. (2018). Treatment in adult ADHD. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 426-436). London: Oxford University Press.
Brown, T. E., Chen, J., & Robertson, B. (2020). Relationships between executive function improvement and ADHD symptom improvement with lisdexamfetamine dimesylate in adults with ADHD and executive function deficits: A post hoc analysis. Primary Care Companion for CNS Disorders, 22(3), pii: 19m02559.
Coghill, D., & Danckaerts, M. (2018). Oranizing and delivering treatment for ADHD. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 417-425). London: Oxford University Press.
Connor, D. F. (2015). Stimulant and nonstimulant medications for childhood ADHD. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 666-685). Guilford Publications.
Dittman, R. W., Hage, A., Pedraza, J. D., & Newcorn, J. H. (2018). Non-stimulants in the treatment of ADHD. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 393-401). London: Oxford University Press.
Frodl, F. T. & Skokauskas (2012). Meta-analysis of structural MRI studies in children and adults with attention deficit hyperactivity disorder indicates treatment effects. Acta Psychiatrica Scandinavica, 125, 114-126.
Ivanov, I., Murrough, J. W.., Bansal, R., Hao, X., & Peterson, B. S. (2014). Cerebellar morphology and the effects of stimulant medications in youths with attention deficit-hyperactivity disorder. Neuropsychopharmcology, 39(3), 718-726.
Li, L., Sujan, A. C., Butwicka, A., Chang, Z., Cortese, S., Quinn, P., Viktorin, A., Oberg, A. S., D’Onofrio, B. M., & Larsson, H. (2020). Associations of prescribed ADHD medication in pregnancy with pregnancy-related and offspring outcomes: A systematic review. CNS Drugs. Epub ahead of print. doi: 10.1007/s40263-020-00728-2.
Moreno-Alcazar, A., Ramos-Quiroga, J. A., Radua, J., Salavert, J., Bosch, P. G., Salvador, R., Blanch, J., Casas, M., McKenna, P. J., & Pomarol-Clotet, E. (2016). Brain abnormalities in adults with attention deficit hyperactivity disorder revealed by voxel-based morphometry. Psychiatry Research: Neuro-imaging, 254, 41-47.
Prince, J. B., Wilens, T. E., Spencer, T. J., & Biederman, J. (2015). Pharmacotherapy for ADHD in adults. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 826-865). Guilford Publications.
Shulz, K. P., Fan, J., Bedard, A. C., Clerkin, S. M., Ivanov, I., Tang, C. Y., Halperin, J. M., & Newcorn, J. H. (2012). Common and unique therapeutic mechanisms of stimulant and nonstimulant treatments for attention deficit hyperactivity disorder. Archives of Psychiatry, 69(9), 952-961.
Spencer, T. J., Brown, A., Seidman, L. J., Valera, E. M., Makris, N., Lomedico, A., Faraone, S. V., & Biederman, J. (2013). Effect of psychostimulants on brain structure and function in ADHD: A qualitative review of magnetic resonance imaging-based neuroimaging studies. Journal of Clinical Psychiatry, 74, 902-917.
Weyandt, L., Sweeney, C., & Thompson, L. (2020). The effectiveness of stimulant medication at improving executive functioning in adults with ADHD. The ADHD Report, 28(7), 1-6.
Wilens, Timothy E. and Hammerness, Paul G. (2016) Straight Talk about psychiatric medications for kids, (4th ed.), Guilford Press.
Zuddas, A., Banaschewski, T., Coghill, D., & Stein, M. A. (2018). ADHD treatment - psychostimulants. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 379-392). London: Oxford University Press.
School Management of ADHD
Barkley, R. A. (2016). Managing ADHD in school. Premier Educational Seminars, Inc.
Barkley, R. A. (2020). Taking charge of ADHD: The complete authoritative guide for parents (5th ed.). Guilford Publications.
Bowman-Perrott, L., Davis, H., Vannest, K., Williams, L., Greenwood, C., & Parker, R. (2013). Academic benefits of peer tutoring: A meta-analytic review of single-case research. School Psychology Review, 42, 39-55.
Charach, A., Carson, P., Fox, S., Usman Ali, M., Beckett, J., & Guan Lim, C. (2013). Preschool children at high risk for ADHD: A comparative effectiveness review. Pediatrics, 131, e1584-e1604.
Children and Adults with Attention-Deficit/Hyperactivity Disorder. (2006). The new CHADD information and resource guide to AD/HD. Landover, MD: Author.
Cooper, H., Robinson, J.C., Patall, E.A. (2006). Does homework improve academic achievement? A synthesis of research 1987-2003. Review of Educational Research, 76, 1-62.
DuPaul, G.J., Eckert, T.L., & Vilardo, B. (2012). The effects of school-based interventions for attention-deficit hyperactivity disorder: A meta-analysis 1996-2010. School Psychology Review, 41, 387-412.
DuPaul, G. J. & Langberg, J. M. (2015). Educational impairments in children with ADHD. In Barkley, R. A. (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 169-190.). Guilford Publications.
DuPaul, G. J., & Stoner, G. (2014). ADHD in the schools: Assessment and intervention strategies (3rd ed.). Guilford Publications.
Dush, D. M., Hirt, M. L., & Schroeder, H. E. (1989). Self-statement modification in the treatment of child behavior disorders: A meta-analysis. Psychological Bulletin, 106, 97–106.
Erchul, W.P., & Martens, B.K. (2010). School consultation: Conceptual and empirical bases of practice (3rd ed.). Springer.
Evans, S. W., Van der Oord, S., & Rogers, E. E. (2020). Academinc functioning and interventions for adolescents with ADHD. In. S. P. Becker (Ed.), ADHD in adolescents: development, assessment, and treatment (pp. 148-169). Guilford Publications.
Fabiano, G. A., Vujnovic, R. K., Pelham, W. E., Waschbusch, D. A., Massetti, G. M., Pariseau, M. E., Naylor, J., Yu, J., Robins, M., Cronefix, T., Greiner, A. R., & Volker, M. (2010). Enhancing the effectiveness of special education programming for children with attention deficit hyperactivity disorder using a daily report card. School Psychology Review, 39, 219-239.
Fowler, M. C. (2006). CHADD educator’s manual (2nd ed.). CHADD.
Gallagher, R., Abikoff, H. B., & Spira, E. G. (2014). Organizational skills training for children with ADHD: An empirically supported treatment. Guilford Press.
Gallagher, R., Spira, E. G., & Rosenblatt, J. L. (2018). The organized child: An effective program to maximize your kid’s potential—in school and in life. Guilford Press.
Greenwood, C. R., Maheady, L., & Delquadri, J. (2002). Classwide peer tutoring programs. In M. R. Shinn, H. M. Walker, & G. Stoner (Eds.), Interventions for academic and behavior problems II: Preventive and remedial approaches (pp. 611–650). National Association of School Psychologists.
McGoey, K. E., & DuPaul, G. J. (2000). Token reinforcement and response cost procedures: Reducing the disruptive behavior of preschool children with ADHD. School Psychology Quarterly, 15, 330–343.
McGoey, K. E., Eckert, T. L., & DuPaul, G. J. (2002). Early intervention for preschool-age children with ADHD: A literature review. Journal of Emotional and Behavioral Disorders, 10, 14–28.
Meltzer, L. (2010). Promoting executive function in the classroom. Guilford Press.
Merrell, C., & Sayal, K. (2018). ADHD and school. . In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 408-4413). London: Oxford University Press.
Miller, F. G. & Lee, D.L. (2013). Do functional behavioral assessments improve intervention effectiveness for students diagnosed with ADHD? A single-subject meta-analysis. Journal of Behavioral Education 22, 253-282.
Nelson, J.R., Benner, G.J., & Mooney, P. (2008). Instructional practices for students with behavioral disorders: Strategies for reading, writing, and math. New York: Guilford.
Pfiffner, L. (2011). All about ADHD: The complete practical guide for classroom teachers. Teaching Resources.
Pfiffner, L. J., & DuPaul, G. J. (2015). Treatment of ADHD in school settings. In R. A. Barkley (Ed.). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th. ed.)(pp. 596-640). Guilford Publications.
Pfiffner, L. J., & DuPaul, G. J. (2018). Possible adverse side effects of school behavioral interventions. The ADHD Report, 28(1), 10-13.
Pfiffner, L.J., Villodas, M., Kaiser, N., Rooney, M., & McBurnett, K. (2013). Educational outcomes of a collaborative school-home behavioral intervention for ADHD. School Psychology Quarterly, 28, 25-36.
Power, T. J., Karustis, J. L., & Habboushe, D. F. (2001). Homework success for children with ADHD: A family–school intervention program. Guilford Press.
Saline, S., & Markham, L. (2018). What your ADHD child wishes you knew: Working together to empower kids for success in school and life. TarcherPerigee (Penguin Books).
Silverman, S. M., Iseman, J. S., & Jeweler, S. (2009). School success for kids with ADHD. Prufrock Press.
Zirkel, P.A. (2013). ADHD checklist for identification under the IDEA and Section 504/ADA. Education Law Reporter, 293(1), 13-27.
Unproven and Disproven Treatments
Bader, A., & Adesman, A. (2015). Complementary and alternative medicine for ADHD. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 728-738). Guilford Publications.
Buitelaar, J., Rommelse, N., Ly, V., & Rucklidge, J. (2018). Nutritional intervention for ADHD. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 373-378). London: Oxford University Press.
Cortese, S., Ferrin, M., Braindeis, D., Holtman, M., Aggensteiner, P., Daley, D., Santosh, PSimonoff, E., Sevenson, J., Stingaris, A., Sonuga-Barke, E. J. S. and the European ADHD Guidelines Group (2016). Neurofeedback for attention-deficit/hyperactivity disorder: Meta-analysis of clinical and neuropsychological outcomes from randomized controlled trials. Journal of the American Academy of Child and Adolescent Psychiatry, 55, 444-455.
Holtmann, M., Albrecht, B., & Brandeis, D. (2018). Neurofeedback. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 366-372). London: Oxford University Press.
Hurt, E. & Arnold, L. E. (2015). Dietary management of ADHD. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 631-640). Guilford Publications.
McGough, J. J., Sturm, A., Cowen, J., Tung, K., Salgari, G. C., Leuchter, A. F., Cook, I. A., Sugar, C. A., & Loo, S. K. (2019). Double-blind, sham-controlled, pilot study of trigeminal nerve stimulant for attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 58(4), 403-411.
Nigg, J. T. (2017). Getting ahead of ADHD: What next generation science says about treatments that work—and how you can make them work for your child. Guilford Publications.
Nigg, J.T., Lewis, K., Edinger, T., & Falk, M. (2012). Meta-analysis of Attention-Deficit/Hyperactivity Disorder or Attention-Deficit Disorder symptoms, restriction diet, and synthetic food color analysis. Journal of the American Academy of Child and Adolescent Psychiatry, 51, 86-97.
Rapport, M. D., Orban, S. A., Kofler, M. J., Friedman, L. M., & Bolden, J. (2015). Executive function training for children with ADHD. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 641-665). Guilford Publications.
Sonuga-Barke, E.J. S., Brandeis, D., Cortese, S., Daley, D., Ferrin, M., European ADHD Guidelines Group (2013). Nonpharmacological intervention for ADHD: systematic review and meta-analyses of randomized controlled trials of dietary and psychological treatments. American Journal of Psychiatry, 170, 275-289.
Sonuga-Barke, E. J. S. & Cortese, S. (2018). Cognitive training approaches for ADHD: Can they be made more effective? In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 358-365.). London: Oxford University Press.


 ContinuingEdCourses.Net is approved by the American Psychological Association (APA) to sponsor continuing education for psychologists. ContinuingEdCourses.Net maintains responsibility for this program and its content.
ContinuingEdCourses.Net is approved by the American Psychological Association (APA) to sponsor continuing education for psychologists. ContinuingEdCourses.Net maintains responsibility for this program and its content. ContinuingEdCourses.Net, provider #1107, is approved as an ACE provider to offer social work continuing education by the Association of Social Work Boards (ASWB) Approved Continuing Education (ACE) program. Regulatory boards are the final authority on courses accepted for continuing education credit. ACE provider approval period: 3/9/2005-3/9/2027.
ContinuingEdCourses.Net, provider #1107, is approved as an ACE provider to offer social work continuing education by the Association of Social Work Boards (ASWB) Approved Continuing Education (ACE) program. Regulatory boards are the final authority on courses accepted for continuing education credit. ACE provider approval period: 3/9/2005-3/9/2027. ContinuingEdCourses.Net has been approved by NBCC as an Approved Continuing Education Provider, ACEP No. 6323. Programs that do not qualify for NBCC credit are clearly identified. ContinuingEdCourses.Net is solely responsible for all aspects of the programs.
ContinuingEdCourses.Net has been approved by NBCC as an Approved Continuing Education Provider, ACEP No. 6323. Programs that do not qualify for NBCC credit are clearly identified. ContinuingEdCourses.Net is solely responsible for all aspects of the programs. ContinuingEdCourses.Net is recognized by the New York State Education Department's State Board for Psychology (NYSED-PSY) as an approved provider of continuing education for licensed psychologists #PSY-0048.
ContinuingEdCourses.Net is recognized by the New York State Education Department's State Board for Psychology (NYSED-PSY) as an approved provider of continuing education for licensed psychologists #PSY-0048.