Learning Objectives
This is a beginning to intermediate level
course. After taking this course, mental health professionals will be able to:
- Discuss
the impact of the aging process on mental health.
- Apply
knowledge of family dynamics with the aging parent to the psychological
treatment of family members.
- Assess
the impact of medical illness on the mental health of the elderly client
(e.g., nutritional deficits, pain, use of medications, sleep disturbance).
- Screen
the elderly client for dementia and recognize the different stages of the
illness.
- List
treatment options for depression and anxiety in the elderly and utilize
effective therapeutic techniques.
This course is designed to help mental health practitioners diagnose and treat mental disorders in older adults living in long term care facilities. Practitioners will become aware of difficulties and complexities of the impact of the aging process and the impact of nursing home milieu on mental health. They will also gain knowledge and skills for working within complex psychological dynamics of family and aging parents and loved ones. Information in this course is based on the most recent research, and is evidence-based. However, readers should be aware that the realm of geriatric mental health is rapidly growing and therefore new research appears day to day.
Introduction
This course on aging is intended for all
clinicians wanting to understand the mental health problems of older adults, most who are using professional care.
This course also meets the mandatory requirements for license renewal for
psychologists, LCSWs, and MFTs in California.
Course Outline
- The
Importance of a Course on Aging
- The
Need for Geriatric Mental health Care
- What
is Different about Geriatric Mental Health?
- Why
Long-term Care?
- What
is Long-term Care?
- Mental
Health Services in the Long-term Care Setting
- The
Impact of Aging on Mental Health
- The
Aging Body
- The
Aging Brain
- Cerebrovascular
Integrity
- Personality
- Family
Dynamics
- Social
Dynamics
- The
Impact of Medical Illness on Mental Health
- Nutritional
Deficits
- Pain
- Medications
- Substance
Abuse
- Sexual
Problems
- Sleep
- Delirium
- The
Impact of Memory and Cognitive Decline
- Age
Associated Memory Impairment
- Mild
Cognitive Impairment
- Dementia
- Types
of Dementia
- Reversible
Dementias
- Subcortical
Dementias
- Depression
& Anxiety Disorders
- Extent
of the Problem
- Anxiety
Disorders in Old Age
- Loss
and Grief
- Suicide
- Barriers
to Diagnosis
- Barriers
to Treatment
- Assessing
the Older Mind
- References
The United States is facing the largest change in
demographics in the history of humankind. People over 55 are now the largest segment
of our society, comprising 21 percent of the total population. Those over 65
are now the fastest growing segment of our population. According to the US
Census Bureau, the number of Americans aged 65 and older grew from about 3
million in 1900 to over 35 million in 2000. During that period, the ratio of those
over 65 to the total population jumped from one in twenty-five to one in
eight.
By 2030, the number of people over 65 will reach 85 million. The elderly will outnumber children by 2050 in most of the world. Worldwide, the number of people over 65 is increasing at about 870,000 every month.
What is more important is the finding that
within the over-65 group, the fastest growing segment is those over 100. In the U.S., the number of people over
100 is tripling every five years. By 2025, 1 in 26 Americans can expect to live to age 100, compared to 1 in 500 in 2000.
During this time, the number of older Caucasians will increase by 97 percent, African Americans by 265 percent, and Latino Americans by 530 percent. Ethnicity will be an important variable in treatment some cases.
Two major forces are driving this trend.
As the boomers are growing up, breakthroughs in public health, sanitation, nutrition, and
medicine have led to an unanticipated increase in life expectancy, and an
unprecedented increase in the number of elder Americans.
This change was brought about primarily by
the establishment of clean drinking water and public sanitation systems, along
with the discovery of antibiotics.
In 1900, pneumonia, tuberculosis, and diarrhea/enteritis were the three
leading causes of death. However,
deaths from pneumonia and tuberculosis declined from about 800 per 100,000 in
1900 to only 60 per 100,000 in 1996. As of 2017 according to the CDC, the leading causes of death are heart disease, cancer, accidents (unintentional injuries) chronic lower respiratory diseases, and stroke.
These problems are less life threatening because of advances in treatment options, and life expectancy is predicted to increase even more in the next twenty years. However, due to this rise in lifespan, dementing illness has increased significantly. Before the founding of the Alzheimer’s Association in 1980, the disease was considered rare. Today, news about dementia appears in every newspaper, magazine, and television newscast. Thousands of older people alive today will suffer from dementing illness. Most will have emotional and behavioral problems as a result.
In the coming years, thousands of older
people will need mental health care.
As a healthcare professional, you cannot ignore the impact of this
demographic change. As your
patients and clients age, they will face new challenges.
Unfortunately only 3% of seniors with mental health problems get treatment from mental health professionals. Few get psychotherapy, and most get psychotropics from primary care physicians, often without a physical exam.
Geriatric mental healthcare is based on the premise that older adults have unique psychological needs. Many will have multiple medical
problems that impact their emotional health and obfuscate accurate
diagnoses. The majority will be
taking medications that can cause psychological and behavioral problems. Others will have changes in memory and
cognition that require that interventions and treatments take on a different approach.
Look at:
- Eating
- Using the toilet
- Caring for incontinence
- Bathing
- Dressing
- Bathing
|
|
Although most adults live independently in their home, many are living in long-term care facilities. The majority of
these people (up to 90 percent) in this setting will be suffering from
mental, emotional, or behavioral problems. The number of people
in long-term care facilities is expected to quadruple in the next twenty-five
years. Neither the long-term care
industry nor the health care professionals who serve their clients are prepared
to meet this challenge.
Currently the quality and availability of
mental health care leave much to be desired. Mental health problems are routinely ignored, medicated, or
tolerated, but seldom treated effectively.
There are a number of reasons for this, one
of which is the broad diversity in quality of the facilities. Although many are exemplary in their
care and resident-centered focus, others are atrocious. While the best facilities are dedicated
to maximizing the quality of life of their residents, the worst facilities
focus on the quest to maximize profits and avoid litigation.
It is this stance that has given the news
media an abundance of horror stories, and the industry a bad reputation. One administrator told me, “We have a
serious marketing problem. We are
the only industry where many people would rather be dead than use our
services.”
In order for this attitude to change, there
must be a fundamental reworking of the delivery of services, and this includes
the establishment of high quality mental health care – delivered by you.
Older Adults
- Present with unusual symptom constellation
- May function well with multiple illnesses
- Are taking an average 4.5 medications
- Are reluctant to seek help for mental health problems
|
|
While this might sound like a foolish
question, it isn’t. The long-term
care industry is still struggling to define itself.
Long-term care services are provided by a
range of different entities – including volunteer organizations,
government-funded facilities, and private companies.
Technically, the term “long-term care”
includes everything from home care and assisted living facilities to
residential homes, but the term is most often associated with nursing homes. Three million Americans resided in nursing homes during 2008.
Currently there are about 17,000 nursing homes in the United States. About
three quarters of long-term care facilities are privately owned, for profit
businesses, marketing various levels of care to the infirm elderly. Nonprofit
institutions currently provide care for about 28 percent of institutionalized
elders, while another 6 percent reside in government-funded facilities. As of
2003, over 14 million people were living in long-term care facilities. Ninety
percent of nursing home residents are 65 and above, and 7 in 10 residents are
women. Over half of women and about one-third of men over 65 will spend some
time in a nursing home. The aging population will increase the number of people in nursing homes 300% by 2030.
Long-term care is a range of services and supports one may need to meet personal care needs. Most long-term care is not medical care, but rather assistance with the basic personal tasks of everyday life, sometimes called Activities of Daily Living (ADLs), such as:
“Nursing home”… that name. That’s
another problem. While the terms
“long-term care facility” and “nursing home” are often used interchangeably,
there is a difference.
Nursing homes came into being to treat
people who were recovering from a serious illness or injury. Once they recovered, they went home.
But today the majority of people living in
long-term care facilities will spend the rest of their lives there. Of the people who are admitted to
long-term care, only 20 percent will return to their previous homes. The long-term care facility will be
their permanent dwelling place – their new homes. This is important because a home should be a sanctuary, a
place to feel safe, and a source of nurturance. Despite this, many long-term care facilities bear a closer
resemblance to a hospital than a home.
Most people – including mental health
professionals – have never set foot in a long-term care facility; this is
largely because people avoid them.
As of this writing, I have yet to meet a licensed mental health
professional whose primary career goal was to work in a nursing home.
While many community-dwelling elderly people
have the same degree of physical disability as those in nursing homes, the
decision for placement in a care facility is usually related to the amount of
family and social support, and the presence of a mental disorder.
Currently in many
states, long-term care facilities house the bulk of the elderly mentally
ill. Since the deconstruction of
the state mental health systems, these people have nowhere to go, and end up in
long-term care.
The problem is that many long-term care
facilities do not see themselves as mental hospitals, and are not set
up to deal with the challenges their residents present. Oftentimes staffs have little or no
training in mental health care, and because they are so overwhelmed with the
tasks they are given, pay scant attention to the emotional state of the people
for which they provide care.
Mental health has always been the bastard
child of medicine, but here it is truly an orphan. It is time we changed that, and this is where you fit in.
Mental health problems are rampant in the
impaired elderly population. In
December of 2003, the reported incidence of mental health problems in long-term
care residents was:
| |
Mental Retardation |
2.82 percent |
| |
Depression |
42.79 percent |
| |
Psychiatric Diagnosis |
18.76 percent |
| |
Dementia |
45.35 percent |
| |
Behavior Problems |
30.62 percent |
Source: CMS OSCAR Form 672: F78, F108 - F114
American Health Care Association - Health Services Research and Evaluation
 Older adults
suffer from the same psychological problems as younger adults. While the proportion of mental health
problems is approximately the same for younger adults, older adults are more
vulnerable than younger adults to develop psychological problems resulting from
factors that impact the quality of life such as stress, ill health, loss,
decline in cognitive skills, and changes in living situations.
Older adults
suffer from the same psychological problems as younger adults. While the proportion of mental health
problems is approximately the same for younger adults, older adults are more
vulnerable than younger adults to develop psychological problems resulting from
factors that impact the quality of life such as stress, ill health, loss,
decline in cognitive skills, and changes in living situations.
Although aging affects everyone, its rate
and extent varies from person to person.
Changes in childhood and adolescence are stepwise and predictable, but
advancing age means increased diversity.
In the latter decades of life, people age at very different rates. For this reason, there is no such thing
as a "typical seventy-year-old."
Aging causes changes in all cells, tissues,
and organs, and these changes impair functioning in all of the body’s
regulatory and repair body systems.
With age, cells become less able to divide
and reproduce. Over time, cells
lose their ability to function, or they function abnormally. There is an accumulation of pigments and fats inside the cells. Cell membranes change, impairing the
ability of tissues to get oxygen and nutrients, and to rid the body of carbon
dioxide and waste products. Heart, blood vessels, and capillary walls thicken slightly. Connective tissue becomes increasingly
stiff, which makes organs, blood vessels, and airways less flexible.
A fatty brown pigment called lipofuscin
collects in many tissues; in the skin, it causes “age spots.” Lipofuscin also increases in the hippocampus and cerebellum which may cause cognition and memory problems. (Green tea may lower lipofuscin and lower oxidative stress in the brain.)
Aging organs gradually lose function. Up to a point, this loss goes
unnoticed, because people seldom use organs at full capability. This means that in day-to-day life, a
person may function normally, but when placed under stress, demands on the
system exceed capacity. When
demand exceeds capacity, organ failure occurs. Loss of reserve also makes it harder for the body to
maintain homeostasis and restore equilibrium. This means prolonged reactions to stress and longer recovery
times from illness.
The immune system may decline, causing changes in interleukins which can alter mental status for months after an illness. H. Pylori infection is associated with mood swings. Therefore infection in the gums can cause mood problems.
Kidneys lose about 6 percent of capacity
every decade after 20. This means
reduced capacity to detoxify the body and eliminate waste. This can affect medication dosages
also, and toxic buildups are common in this population.
About 20 percent of women and 8 percent of
men over 65 will experience urinary incontinence. This has a great impact on their sense of control, and also
leads to anxiety, embarrassment, and social isolation.
The most significant changes occur in the
heart and lungs. With age, the
heart loses elasticity, which reduces capacity. Thickening of the aorta decreases delivery of blood to the
muscles. Lungs lose function also. The average 65-year-old today has about
40 percent of the aerobic capacity he had at 30. The combination of decreased heart and lung functions means
loss of vital capacity, and impairs the person’s feelings of stamina and
well-being. This loss also
contributes to the sense of “being old,” and has a great impact on the person’s
identity and sense of self. Fortunately,
these changes can be minimized by an exercise program. A person’s willingness or reluctance to
participate in such a program can tell you a lot about their mood, coping
skills, and lust for life.
Some of the Causes of Brain Aging
- Debris accumulates inside and outside of cells.
- Repair mechanisms slow down.
- Deteriorating cells release chemicals, which harm other, healthy
cells.
- Lifestyle and environmental factors kill brain cells.
- Blood flow decreases
- The immune system changes brain function
|
|
Studies show that brain cells begin to die
at an early age. Brain weight
actually peaks at 20-25 years and steadily declines thereafter. In healthy people, the brain loses 5 to
10 percent of its weight between the ages of 20 and 90.
Researchers say age-related changes in the brain in four distinct periods of life. About 20 to 30 percent of central
nervous system cells are lost from age 25 to 80. For some unknown reason, this cell loss is greater in men
than it is in women of the same age.
After age 40, the hippocampus – the part of
the brain that allows us to store new memories – loses about 5 percent of its
cells every ten years. As a result
of this cell loss, the average healthy eighty-year-old has about two-thirds of
the hippocampal cells that he had when he was born. Although cell loss is significant, there are fortunately, so
many cells in these brain areas that the normal loss of cells does not
significantly impair brain function.
The greatest loss of neurons occurs in the
superior temporal gyrus, a part of the brain that moderates hearing, taste, and
smell, and in the anterior central gyrus, which controls movement. The smallest amount of loss occurs is
in the posterior central gyrus, which controls peripheral sensation.
As nerve cells are lost, glial cells (cells
that support and nourish brain cells) increase in number, size, water content,
and weight. Ventricles (the hollow
chambers in the brain that contain spinal fluid), increase in size. Myelin (the insulation around the brain
cells) thins. Inter- and
intracellular deposits of lipofuscin and heavy metals such as aluminum,
cadmium, and iron increase.
Microtubules (the scaffolding that supports the cell) decrease in
number, and the neurofibrillary tangles symptomatic of Alzheimer's, composed of
deformed microtubules, proliferate.
Neurotransmitters decrease up to 50 percent
in some areas. This occurs
especially in the substantianigra and basal ganglia (areas where dopamine is
found) often resulting in Parkinsonian-like symptoms. Dopamine also regulates pleasure and reward, and its loss
can cause apathy and disinterest – common symptoms in the elderly, very often
mistaken for depression.
The vascular system is the most potent predictor of brain health. Many have high blood pressure, but often have no symptoms. About 85% of people who die from coronary artery disease or stroke are over 65.
Researchers are now saying that high blood pressure at sleep-time is an independent predictor of cardiovascular and cerebrovascular disease. They also have found that people who sleep five hours or less a night are more prone to higher risk of developing high blood pressure. Therefore asking about sleep should be useful. Men with erectile dysfunction often have concurrent vascular problems.
The brain undergoes multiple changes with age. High blood pressure can cause damage to the brain. With age, the brain’s blood supply decreases. Because of this, there is a 20 percent decrease in blood flow from 30 to 70 years of age. As vessels thicken, they impair the transport of nutrients and oxygen. Capillaries die. In spite of its high prevalence of vascular diseases, only 10 to 20% over 65 will be clinically diagnosed.
In any part of the brain, thickening and
stiffening of the arteries and arterioles will result in disturbances of blood
supply, resulting in impaired brain function. The most common causes of this are hypertension, diabetes,
cigarette smoking, and hyperlipidemia (elevated levels of fats in the
bloodstream that include cholesterol and triglycerides).
Blockage of cerebral arteries by plaques or
from emboli (floating bits of fat and cholesterol in the bloodstream) can also
block blood flow and cause small strokes (often called infarcts). The most common causes of this are
atherosclerosis and cardiac arrhythmias, both found in many older people.
Unfortunately many older adults were long-term smokers, and therefore will be suffering from both vascular and lung
problems, both of which impair brain function.
Recent research done in Europe by Alewijn Ott involving more than 9,000 elderly people noted that older smokers lose
cognitive abilities five times faster than nonsmokers do. Furthermore, the more a person smoked,
the higher the rate of decline they experienced.
Although impaired blood flow is damaging to
all parts of the brain, the most vulnerable areas are the basal ganglia and
subcortical white matter. In
contrast to the cortex, which has a double vascular supply, the subcortical
white matter and basal ganglia have but a single, minimally-branching
supply. Therefore, any damage in
this blood supply means that the basal ganglia or white matter will become
ischemic, and cells will experience demyelination, and die. These are parts of the brain
responsible for movement, coordination, and volition.
Be aware that many older adults are taking statin drugs (cholesterol-lowering drugs). These drugs are known to cause mood disorders and significant cognitive problems. In the elderly, lowering cholesterol is related to all-cause mortality elder adults, even when adjusted for other health status or indicators of frailty. Statins are also associated with an increased risk of rheumatoid arthritis, which can cause agitation and depression.
Personality
Personality appears to remain relatively stable throughout the lifespan, but age often changes behavior, cognition, and emotion.
For example, in a 2002 study of aging, researchers Helson, Kwan, John, & Jones stated that, in healthy adults, the trait of neuroticism (a tendency to be in a negative) and extraversion (people how like to talk to others) decline, while the traits of agreeableness and conscientiousness increase. They found evidence that personality does change during adulthood.
Another study by Field and Millsap reported that neuroticism decreased
until age 69 and remained stable until age 83, while agreeableness increased
and extroversion declined until age 83.
Elders who score high in neuroticism and low in extroversion have poorer
perceived health, and are more likely to suffer from anxiety and depression as
result.
In 1964, Bernice Neugarten, et al. conducted a
10-year longitudinal study of aging and personality suggesting that, in healthy elders, change in coping styles,
life satisfaction, and goal-oriented behavior remained stable from ages 40-80. However, there was a shift from what
they labeled Active Mastery (e.g. risk-taking) to Passive Mastery (greater accommodation, and seeing environments as threatening). With advancing age, subjects reported a
greater preoccupation with inner feelings, experiences, and cognitive
processes, and avoidance of external influences on belief structures (i.e. more
set in their ways).
Researchers Mroczek and Almeida
(2004) at Fordham University found that aging resulted in a stronger association between daily stress and
negative feelings. The higher a
person scored in the trait of neuroticism, the stronger the reaction the person
experienced. They concluded that
there was a heightened reactivity to stressors in older adulthood, perhaps due
to kindling effects, most likely caused by changes in the aging brain (see
above).
While the evidence suggests that personality
traits are relatively stable, so are personality disorders. This means that older people retain
their maladaptive traits as well as their healthy traits. The interface of aging and personality
disorders often results in exacerbation of pathologies because of the person’s
greater need for help, medical attention, and support. Unfortunately, older people with
personality disorders are often described as “grumpy old people” and do not get
the help they need.
The presence of a personality disorder is a
common reason for referral to a long-term care facility. For this reason, many people in
long-term care may be volatile, difficult people who are also struggling with
medical problems and cognitive changes.
This presents a challenge for staff and administrators, many of whom
know nothing about personality disorders and therefore may actually exacerbate
problems. There is a great need
for mental health professionals to provide intervention and education in this
treatment setting.
Researchers say that a patient-centered paradigm is the best way to help the elderly. Such a paradigm means getting to know the person and understanding his or her needs, also doing a complete workup looking at needs, pain, fear, and loneliness.
About fifty million Americans provide care to an older relative or friend. Caregiver and family therapy is probably the most
overlooked resource for the older population. At the time of this writing, we are just beginning to
acknowledge the immense need for this type of intervention in dealing with
family stress, caregiver burnout, and dealing with very complicated family
constellations.
Because of the increase in lifespan, the
average adult today will experience triple the amount of years spent with
living parents than in 1900. This
means more support from parents, but also more responsibility in caring for
them. The “sandwich generation”
has emerged. Many elders will
eventually come to live with their children.
The most common cause of family discord is
when a parent becomes too ill to live independently and begins to depend on
children for assistance. According
to researcher Victor G. Cicirelli at Purdue University, this causes filial
anxiety – the anticipation of significant responsibilities often causes
friction and conflict between the parent and child. As parents lose the role of power, retaliation and
resentment often arise. Old wounds
are revisited and old issues reappear.
Friction between siblings is ignited. Old family rivalries and power
struggles are reinstated. Adult
children of the elderly often become conflicted between control and
responsibility. Children argue
over who will accept responsibility for the ailing parent. Once the decision is made, the chosen
sibling may get constant criticism about the way she is handling things.
Eventually most adult children of elders
achieve filial maturity, that is, they have accepted the responsibility
of being depended upon by their parents, but in families where the parent-child
relationships have been stormy, trouble will brew. Loss of power in which a resented parent reanimates old
wounds is a frequent cause of elder abuse.
After rivalries and conflicts have been
resolved and caregiving commences, caregiver burnout often occurs. When a caregiver becomes emotionally
and physically drained due to the caregiving role, irritability, fatigue, and
depression set in. At this point,
many caregivers become ambivalent about their role. This may manifest itself as argumentativeness and
belligerence, followed by bouts of guilt.
Families often become destabilized and volatile without being
consciously aware of the source of their discord.
Because of extended life spans and the need
for companionship, many elderly people remarry, while others cohabit because of
the financial consequences of marriage.
As a result, family constellations become
very complex; with multiple marriages come new children, nieces and nephews,
stepchildren, and many sets of grandchildren. Boundaries and loyalties are fuzzy and confused, and many
conflicts arise.
While working with younger people may not
involve family sessions, interactions with family members are an important part
of every care plan in this population.
At best, the family can be a valuable resource. They can provide historical information
and furnish data on what types of care giving have been most successful in the
past. They also provide a powerful
source of comfort and support for the resident.
But at other times, families may present
problems. In many cases, the
family members have become accustomed to being the primary caregivers, and are
over-involved with the patient.
Although they mean well, they may disagree with caregiving, and
sometimes actually interfere with treatment.
According to researchers J. Paul Teusnik and Susan Mahler, families of elderly
patients with progressive cognitive decline undergo a step-wise process in attempting
to cope with the disorder. Teusnik and Mahler feel that families coping with
debilitating disease exhibit similar reactions to families coping with death.
Because of this, caregivers should provide the families with information and
education about this process so that they can see that what they are feeling
is normal. With support and guidance, a family can successfully work through
its reactions and be able to mourn the loss of their loved one, make the necessary
decisions for her care, and reestablish a new family equilibrium.
Denial
At first, family members may notice memory
and behavioral problems in their loved one, but explain them away by saying
that they are just from “stress,” or part of getting old. In spite of the evidence, they insist
that there is nothing wrong with their loved one. This reaction is sometimes the result of the family's lack
of education about aging, but it is also a wish on the part of family members
to deny what they are seeing.
Denial is a way of defending against the
pain of loss. In addition, the
frequent family fights about how to handle the loved one’s illness may actually
be a way for the family to postpone dealing with its grief. In these cases, denial makes any
objective assessment, decision-making, and treatment-planning difficult.
Families who exhibit excessive denial must
be helped through education and, at times, through outright confrontation in order
to recognize the extent of the disability of the family member. Although this may lead to further
anger, it is only when denial is overcome that the family will be able to make
sound decisions and realistic plans for treatment.
Over-involvement
Denial is often followed by intense
over-involvement of family members with the patient in an attempt to deal with
the illness.
As the deterioration of the afflicted family
member becomes more obvious, family members may take over daily tasks and
responsibilities in an effort to compensate for the deficits.
At this point, a role reversal takes
place. Frequently the family
member must almost become a parent to his or her own parent. This can be one of the most difficult
adjustments that a family member must face. In addition, he often must assume the patient's former
family role, which may include taking over legal and financial
responsibilities. This task can be
difficult and stressful.
Occasionally, family fights break out about who is to take on this responsibility. Sibling rivalry reemerges.
In many cases, a child must take on this role even if the patient’s spouse
is still living. Tasks and responsibilities that were done by one spouse for
many decades are sometimes incomprehensible to the non-ailing partner. For example,
some wives have never written a check or paid a bill, and, in combination
with the stress of dealing with illness in their spouse, find the task overwhelming.
When involvement with a parent becomes an
obsession, family members sacrifice their personal lives and become consumed
with the caregiving task. Even
when they recognize that they are in over their heads, they may be reluctant to
seek professional help, thinking that to do so is to betray their parent.
In fact, some families raise sons or
daughters to believe that they must care for their parents regardless of how
disruptive it may be to their own lives.
The children feel that to not do so will result in ostracism and
ridicule by their family, and their community. This belief often stretches them to the breaking point.
In these cases, the person must be helped to
understand what is within his
power to do, and what is beyond his limits.
Professional caregivers should be able to
recognize the difference between a normal reaction and over-involvement within
the family and its culture.
Families must be helped to see that their over-involvement is actually a
hindrance rather than a help in providing top-quality caregiving.
When doing this, family members should be
provided with solid evidence of what problems the over-involvement is causing
for the patient, the staff, and for the rest of the family.
Anger
Eventually, over-involved family members
react in anger, feeling unable to shoulder the tremendous burden of caring for
their loved one.
Anger among family members develops for many
reasons. In addition to the burden
of caring for a disabled spouse or parent, they cannot tolerate the bizarre and
socially inappropriate behavior the loved one is exhibiting. Anger also can erupt from the feeling
of having been abandoned by a still-living, but now helpless, parent or spouse.
Regardless of its source, this anger is
often projected or displaced onto the very people who are trying to help the
family deal with their overwhelming sense of helplessness – the caregiving
professionals.
Mental health professionals must be able to
recognize this, and help the family confront and deal with its anger. When families fail to see that they are
projecting their own painful feelings on caregivers, they often accuse staff of
neglecting the patient and causing the deterioration that, in reality,
naturally occurs with this illness.
Since the normal reaction to being accused
of neglect is defensiveness or anger, either of which will further alienate the
families, caregivers must be able to handle this anger effectively.
Guilt
As anger lessens, guilt may become more
obvious. Feelings of guilt can be
a normal reaction to recognizing the feelings of anger. Guilt may also come from unexpressed-as-unacceptable
wishes that the suffering loved one die.
Family members may feel guilty for believing
they waited too long before seeking professional help – and by doing so
contributed to the suffering.
Guilt can also come from the need to make medical and financial decisions
that are objected to by the elderly person.
Guilt may also be the reawakening of old
feelings – feelings that they were not attentive enough to their parent or
spouse in earlier times – or for abrasive and cruel comments from times passed.
Family members often mix their guilt with a
dash of failure. They have tried
their best to care for their loved one, but the task was more than they could
bear. It is vital to keep this in
mind when dealing with family members.
You cannot truly understand their pain until you have walked in their
shoes. In these cases, support
groups can be a great resource for families that have been struggling with an
ailing elder.
Unfortunately, this guilt sometimes becomes
translated into a need to dictate orders to the staff and caregivers. They confuse interference with
involvement. One such case
involved Jim Stevens and his father.
Jim
Stevens brought his father to the nursing home because caring for his dad was
disrupting his job to the degree that he was at risk of being fired.
He
told the administrator that he wanted to be notified of any and every problem
his father was experiencing. He
made it clear that no treatment of any kind was to be administered to his
father without his approval.
In
reality, Mr. Stevens was very difficult to reach. He seldom returned phone calls, and sometimes could not be
reached at all. This resulted in
impeding any semblance of quality care.
The
administrator invited Mr. Stevens to a meeting and said, “Mr. Stevens, I know
you care for your father a great deal.
I know you worry about him.
And we are all impressed with your concern and your involvement. It is true that you want the absolute
best for your dad, isn’t it?”
“Of
course,” he replied.
“Well
the absolute best care we can give requires immediate intervention at
times. If we have to wait, your
father may suffer unnecessarily.
You wouldn’t want to stand in the way of helping him, would you?”
“No. Of course not,” he said.
“Then
I guess we both agree that when we cannot reach you, we should do what we feel
is in your father’s best interest, right?”
“I
suppose so,” he said.
“Great,”
She said, “then I would like you to sign this agreement stating that if we
cannot reach you within an hour, we can do what is best for him.”
In this interchange, several things
happened:
- The
administrator validated Mr. Steven’s feelings and concerns.
- He
got him to agree that the best care was the most important issue.
- He
got him to agree, in writing, that they could proceed with
treatment if they could not reach him. This assured that there would be no misunderstanding.
Mental health professionals can most
effectively deal with the family members’ guilt by discovering its cause, and
taking corrective steps to alleviate it.
One component of this can be simply to
educate the family about the illness itself, thereby providing reassurance that
the family has not harmed the patient.
More extensive counseling may be needed to help the family make
difficult but necessary decisions, some of which may be objected to by the
patient.
Acceptance
Acceptance comes only when a family is able
to truly understand the disease or disability that is affecting the loved
one. Once the family members have
worked through the bulk of their anger and guilt, and have recognized that
their loved one is no longer the person they once knew, they can accept the
loss.
In cases of dementia, acceptance can be
especially difficult. This
disease's insidious onset and long, slow progress give one false hope that
things will remain as they are. In
addition, the patient's relatively normal appearance during the early stages of
the illness makes the problems seem less serious than they really are.
Here’s an example of these problems in a
case described by Teusnik and Mahler:
Mrs.
K, a profoundly demented 76-year-old Jewish widow, was transferred from a
long-term care facility to the Cornell Medical Center for an evaluation of
agitated behavior including constant pacing, verbal abusiveness, and at times,
combativeness.
Although
Mrs. K had exhibited symptoms of Alzheimer's disease for approximately one and
a half years, she had worked in her family's garment manufacturing business
until one year before her transfer to the Center.
In
the transfer summary, the nursing home complained of difficulty with the
patient's 50-year-old son, who was running his mother's business.
During
the initial phase of his mother's hospitalization in our facility, Mr. K was
unable to accept his mother's progressive deterioration and was insistent that
certain signs, such as intact long-term memory, were proof that she was less
impaired than he had been told. He
believed that his mother's wandering stemmed from her boredom at not having
work to do and from the lack of staff engaging her in activity.
Mr.
K visited his mother nightly and brought her dress patterns to cut. When she was unable to perform the
tasks he expected of her, he displaced his disappointment and anger onto the
nursing staff in a hostile, abusive, and accusatory fashion, thus engendering
staff defensiveness and resistance to empathizing with his pain. Mr. K was critical of all aspects of
his mother's treatment and expected the hospital to find a miracle cure for her
illness.
Engaging
Mr. K in family therapy was difficult since he saw both the doctor and social
worker as his adversaries. He was
seen in weekly sessions, where he was encouraged to talk about his frustration
at our inability to make his mother well.
At
the same time, we educated him about Alzheimer's disease – its manifestations,
course, and treatment.
Mr.
K eventually revealed his concerns that the illness was hereditary or
contagious, and his feelings of helplessness in caring for his mother. He had attempted to have her live with
his family before placing her in a nursing home, but he and the family were
unable to control her wandering and disruption of family life.
As
Mr. K began to discuss his family history and his feelings about his mother, it
became clear that he had a conflict-ridden, ambivalent relationship with her.
Mrs.
K had worked long hours in the family's business since Mr. K was a young child
and had left his care to an older sibling. Mr. K had felt neglected and abandoned, and had developed
angry feelings toward his mother.
Having
to put his mother into a nursing home reawakened these repressed feelings of
anger and abandonment, and aroused concerns that he was now abandoning
her. He was still unable to see
his mother as anything other than the strong, capable, working woman he had
known in the past, and although he was capable of running the family business,
he was experiencing self-doubts.
In addition, he was furious at his sibling, who lived out-of-town and
was not involved with his mother's care.
Mr.
K's reminiscences about his mother helped him to realize the source of his
angry feelings and he became less critical of the staff.
His
lessened anger enabled him to understand the symptoms of Alzheimer's disease,
to more realistically assess his mother's illness, and to mourn her loss.
When
Mrs. K was discharged from our facility, we talked with the social worker in
the long-term care facility where Mrs. K would return, so that we could apprise
her of Mr. K's conflicts and encourage her to provide him with continued
support.
In other cases, family members have become
estranged from the patient, and don’t wish to have any involvement at all. In these cases, unresolved feelings of
anger, frustration, helplessness, grief, and fear interfere with healthy family
interaction. Once again, family
therapy and family support groups can be very useful.
Unfortunately, in some cases, the family
members have been not only neglectful, but also abusive. In a survey done in 1988, researchers
Pfiffer and Finklehor discovered that between 3 and 4 percent of elders experienced
abuse by family members. In the
majority of cases, the abuser was the patient’s spouse. They also discovered that only one in
fourteen cases was ever reported.
Social support plays an important part in
the potential for abuse. Elderly
people who are isolated from all but their caregivers are four times as likely
to suffer abuse as those who have social support. Men are more likely to be abused than women because elderly
men seldom live alone.
Regardless of who they are, how they act,
and what they have done, family members must always be treated with respect,
deference, and consideration. Like
the residents, families must be considered to be customers.
Family Visits in Long-term Care
One frequent problem that long-term care
residents have is loneliness. Many
elders have no families, while those that have families complain that they
don’t visit enough. Although this
is often true, in some cases these complaints arise because the resident simply
doesn’t remember the visits.
Unfortunately, family visits can be a source
of trouble. Negative interactions
with family can irritate and agitate patients. For this reason, therapists should encourage families to
keep the climate of the visit positive.
Explain to them that fighting and friction during a visit can cause
behavioral problems for several days.
Family visits can also be an opportunity for
residents to complain about the facility and the quality of care. Although some of these complaints may
be valid, in many cases the person complains of poor care either because they
cannot remember many of the things that are done for them, or because they get
pleasure out of stirring up trouble.
Mrs.
Whitkin’s daughter would visit twice a week. She would arrive at ten o’clock, and spend an hour with her
mother. During these visits, Mrs.
Whitkin would complain incessantly about not being fed, not being cared for,
and being generally neglected.
We
suggested to her daughter that she come to the facility unannounced at
different times during the day and stand where her mother could not see her, so
that she could observe the things we did for her mother. In this way, she was able to see that
we were in fact doing the things that Mrs. Whitkin claimed we did not do. The daughter then realized that much of
what we were doing was simply forgotten.
Working with Families
Because families play such an important role
in the mental and physical health of their older loved ones they are an
important part of treatment.
Therefore, treatment planning includes spending time with the resident’s
family.
Get to know them, and learn about their
expectations, attitudes, and concerns.
They are not only a source of historical information, but also are
emotionally involved and impact the life of the person being treated.
Involve the family in the care plan whenever
possible. Even minimal
participation gives them a feeling of power and participation, and increases
treatment compliance a great deal.
Encourage them to join a family support
group, and put them in touch with community resources such as the Alzheimer’s
Association and the National Family Caregivers Association.
Listen to, acknowledge, and validate the
feelings and concerns family members are having. If they are not forthcoming with these feelings, offer
information on what kind of feelings are typical and ask them if they are
experiencing any of them. For example,
you might say, “It’s common for families to feel frightened, depressed,
defeated, or guilty about the decision to seek professional help. It would not be unusual for you to be
feeling any or all of these things.”
Family members sometimes express their
concern and anxiety as anger. When
this happens, it is very important that you do not internalize a family
member’s anger. This simply means
that you don’t take their anger personally. Instead, validate their anger and offer solutions. Be responsive, not reactive. Instead of getting angry, say, “I can
hear that you are very upset. I
understand. Let’s see what we can
do to solve the problem.”
Tell family members about the resident’s
current condition. Carefully
explain the symptoms and problems that the resident is experiencing. Explaining problems and unusual
behaviors helps the family understand and cope with what they are seeing. Explain how the resident’s current
condition creates specific needs, and show how these needs can best be met.
Video and Audio
Today’s phones, pads, and other devices are very useful in long term care. These devices allow the patient to talk to and see their friends and families. Most of these devices have audio and video recording of the visits are very useful. While it is not as gratifying as a real visit, most people enjoy them again and again. These devises can also be used for music, movies, books, and magazines.
Social Dynamics
Symptoms of Relocation Stress Syndrome
- loneliness
- depression
- anger
- apprehension
- anxiety
- sleep disturbance
- changes in eating habits
- increased dependency
- insecurity
- lack of trust
- excessive need for reassurance
|
|
As mentioned above, adult children tend to
minimize the impairments and disabilities of their parents and overestimate
their ability to care for them.
They are often in denial about the severity of a parent’s illness and
have an unrealistic view of their coping skills. Eventually, caregiver burnout takes its toll, and with it
comes the realization that a higher level of care is needed.
Although most families make heroic efforts
to care for their ailing elderly, many eventually are forced to consider moving
the person into a professional care facility.
The decision to admit a parent, a spouse, or
any family member to a health care facility is difficult and painful. It is usually made when all other
alternatives have been exhausted.
It is seldom made without guilt, remorse, hurt, and anger.
The move from home to a retirement home,
assisted living, board and care, or skilled nursing facility is a very
difficult transition for both resident and family.
To family members, it means the loss of much
of what has become familiar. They
must adjust to living without the loved one. They must grapple with the reality that they are not
equipped to give adequate care.
They must lick their wounds and learn their limitations.
To the person entering the professional care
facility, it means dealing with multiple losses. She loses her home, her privacy, and her independence. Friends, treasured objects, lifestyle,
and much of what she knew are gone forever. This overwhelming sense of multiple losses is usually
accompanied by anxiety, depression, and disorientation.
This sense of multiple loss, especially when
combined with cognitive and memory problems, usually causes new residents to
have extreme difficulty adjusting to their new environment – in short, they
don’t know where they are or where their personal belongings have gone, and
they get scared.
Although leaving home and entering a care
facility is traumatic, relocation from one facility to another also takes its
toll on the physical and psychological health of elders. In fact, older people face an elevated
mortality risk whenever they are relocated. Studies of the effect of transferring people show that there
is an elevated mortality risk – between 1.99 and 3.76 times greater – than
those who are not transferred.
In 1992, after years of observing and
documenting this problem, health care experts officially named this phenomenon Relocation
Stress Syndrome. The United
States Administration on Aging calls this problem Transfer Trauma, and
notes that relocation is associated with depression, increased irritability,
serious illness, and elevated mortality risk.
After a move, the fear and grief that the
person experiences are often expressed as anger and agitation. While fear disables a person, anger is
empowering. To a person who has
lost most of her personal power and position, anger and resistance may be the
only way to feel her impact on the world.
Therefore it’s not uncommon the see recently relocated people labeled as
agitated, combative, and resisting care – when they are actually feeling
powerless and helpless.
Understanding the origin of this fear,
anger, and resistance allows caregivers to reach beyond the anger and gently
touch the pain. A kind word and an
understanding attitude can make this difficult transition much more bearable.
The stress of moving to a care facility was
carefully examined by Coffman in 1983.
He pointed out that it wasn’t the move itself, but the person’s
perception of the quality of care and the social support they would receive at
the facility that was most traumatic.
In other words, it was not the change itself but the emotions that
surrounded that change that made the event difficult.
With age, social circles decline. Most institutionalized aged people have
no spouse, no close relatives, and the majority of them have no visitors. A new term – elder orphans – has been coined to fit this
population. Up to 60 percent of
people in long-term care have no family.
Because of this, they may have no contact with the outside world. This type of social isolation results
in rapid deterioration of physical and mental health.
Another social dynamic that is often
overlooked is the impact of cultural differences. For intervention and treatment to be effective, the
practitioner must take into account the norms, values, lifestyles, diets, and
diseases of various ethnic groups and the impact that they can have on elderly
people. Although much work has
been done in the field of cross-cultural psychology, little has been done in
elderly ethnic populations.
Cultural differences affect willingness to seek treatment, compliance
with treatment, and the ways that families treat their elder members. For instance, researchers find that African
Americans, Native Americans, and Hispanics place a great deal of importance on
self-sufficiency, pride, and independence.
Probably the biggest difference between
treating emotional and behavioral problems in younger people and in the elderly
is that most elderly people are also suffering from multiple medical
problems. Psychological
problems in this population are often indicators of physical illness. In fact, more than half of all older
psychiatric patients have an undetected physical illness.
Symptoms of Constipation
Behavioral Symptoms:
- Fatigue
- Lethargy
- Irritability
- Restlessness
- Quarrelsome
- Intolerant
- Lack of Endurance
Physical symptoms:
- Shoulder Pain
- Generalized Pain
- Fever
- Headache
- Vomiting
- Nutrient Malabsorption
- Malodorous Stool
- Poor Digestion
- Faulty Metabolism
|
|
Older people who have a previous history of
mental illness are more likely to suffer from mental problems in later
life. Barring that, medical
illness is the strongest predictor of mental illness in the elderly. High medical users are more likely to
suffer from depression, anxiety, and adjustment disorders.
Medical illness also predicts cognitive decline. In a 2003 study by Backman,
et al. looking at how age, social status, education, and substance use
affected mental status, only the number of diseases resulting in hospital
admission during the follow-up period predicted an accelerated
decline in mental status.
A troubling finding in geriatric mental
health assessment is that almost 80 percent of physical illnesses are
missed by psychiatrists during the initial assessment. This happens in part because mental
health practitioners are trained to look at symptoms as signs of
psychopathology, not medical illness.
The other reason for this oversight is that only about 10 percent of
psychiatrists specialize in geriatrics. The three top unrecognized conditions are constipation, urinary infection, and hypothyroidism.
The reality is that medical problems can
cause serious behavioral and emotional disorders, and these factors should
always be considered before any diagnosis or behavioral intervention is
attempted.
Medical disorders may also present
themselves as confusion or functional decline. These things may be mistaken for normal aging, while they
are, in fact, masking a serious problem.
It is important to be aware that while there are many people who have medical causes for
mental illness, almost everyone has strong emotional responses to
physical illness. Disease burden significantly increases levels of stress,
anxiety, and depression.
For example, people undergoing dialysis face
multiple challenges. First, they
must cope with the loss of function of their kidneys. This is a devastating loss, which is
often accompanied by a great deal of anxiety, depression, and grieving. Second, dialysis means adopting an
entirely new lifestyle – one in which several days a week are devoted to
treatment. Third, a majority of
people in dialysis feel exhausted after the procedure, and cannot do anything
strenuous the rest of the day.
Fourth, they must accept strict dietary restrictions to maintain their
health.
Dialysis patients also have a high incidence
of sleep apnea, which causes cognitive problems and exacerbates fatigue.
Dialysis patients are at risk for thiamine deficiency, which may mimic symptoms
of dementia. In rare cases, dialysis can result in a toxic buildup of aluminum
in the brain, which results in dementia-like symptoms (sometimes called dialysis
dementia). This occurs over time in areas where the water supply contains
high levels of aluminum. Although this is a fairly well known phenomenon, it
is often overlooked or missed. Untreated, it is often fatal.
The incidence of depression is very high among dialysis patients,
and a depression screening should be routine in this population. About one in
ten people undergoing dialysis choose to end their lives by discontinuing treatment.
Post-Surgical Problems
Elderly people often undergo surgery, and
although most of these surgeries go well, it is not uncommon to see drastic
behavioral changes after their return from the hospital. The trauma of surgery itself always
causes a significant amount of stress.
The most common problems associated with surgery are:
- Adjustment
disorder
- Post-surgical
depression
- Post-surgical
psychosis
- Biochemical
and metabolic imbalances (for example, blood pressure changes after
amputation)
About 30 percent of older adults will
experience irreversible problems with memory and cognition after a major
surgery. Problems with memory and
thinking after surgery occur because of several factors.
Caloric demand, the amount of energy
consumed by the body, often increases as the body tries to heal itself. If nutrition isn’t adequate, the brain
is most often the first organ to suffer.
Sometimes tiny clots are thrown during and
after the surgery, which may result in minor strokes and, consequently,
impaired brain function.
Older people may also fail to metabolize the
anesthetic properly. The effects
of anesthetic can often linger for weeks after surgery, and can disrupt the
person’s ability to function. In
addition, being anesthetized for hours may causes anoxia (oxygen
starvation) which can lead to diffuse brain damage, causing memory and
behavioral problems.
Problems Associated With Amputation
- Pain
- Phantom Pain
- Balance
- Gait
- Blood Pressure Changes
- Grief
- Body Image Disturbance
- Neuropathy
- Depression
- Cognitive Impairment
|
|
Body Image Problems
Unfortunately, many elderly residents
undergo the loss of a body part, limb, or the loss of the function of a
limb. Losing a limb is a traumatic
and devastating experience. As
well as altering the person’s ability to function normally in the world, the
loss changes a person’s body image and sense of self. They no longer feel normal; often, they do not feel accepted.
These feelings are made worse by the
reactions that others have to the injury.
Many people find amputations frightening, and avoid looking at a person
with a missing limb. In their
efforts to cope with their fear of rejection, the person may become withdrawn
or lash out at others, feeling that by rejecting others, they can save
themselves from being rejected.
During this time, the person may be difficult
to work with – they may be uncooperative, unpleasant, and abusive. It is important to keep this in mind
when working with a person who has lost a limb.
It is normal for a person to go through a
period of grieving for their missing limb, yet they are often reluctant to
discuss their feelings with others.
Addressing the issue head-on is often the best way to open the avenue to
communication. A statement such as,
“Last year I was working with someone who lost her leg. She told me it was a very difficult
time for her. I wonder if you
might be feeling that way, too.”
Other problems accompany amputations. Blood pressure may be altered. Balance and gait may be affected, and
phantom-limb pain may cause discomfort and anxiety. About one-third of women have phantom breast sensations
after a mastectomy. There is research describing successful treatment with acupuncture for phantom-limb pain.
Post-Stroke Depression
At Eastern Cognitive Disorders Clinic, cognitive neurologist Amy Brodtmann has found that each year around fifteen million people worldwide have a stroke . Of these, at least five million die, a third remain disabled, and the remainder make a good recovery.
Yet depression is a common consequence of stroke. It is particularly true if the stroke has resulted in permanent disability. The patient often loses much of his independence, and often suffers from body image difficulties previously discussed.
If the person has lost the ability to speak,
things are even worse. Loss of the
ability to communicate is a devastating loss, and often results in complete
withdrawal.
It is very useful in these cases to get a
complete speech and language assessment.
An augmented communication screening is
an assessment that determines a person’s ability to use a computer, iPads and other devices that contain programmed speech. When people are able to use this device
their world changes.
Dehydration
Several years ago, I was called in to see
80-year-old women named Madeline.
She had recently become confused, disoriented, and was beginning to show
some signs of dementia. In the
course of the interview, it was discovered that she was drinking very few
fluids. When fluids were
increased, the symptoms went away within three days.
A
great many elderly people do not drink enough water. In some cases, this is because they have lost their sense of
thirst. But after asking dozens of
people why they don’t drink water, the answer I get the most is, “Because it
makes me pee.”
And they are right. The decreased fluid intake reduces
their need to urinate.
Incontinence is often a source of shame and inconvenience, and not
drinking reduces the problem.
Unfortunately, it also causes fluid and electrolyte imbalance in the
brain, and can cause dementia-like symptoms. Very often, correcting incontinence problems eliminates dehydration,
and thus eliminates behavioral problems.
Head Trauma
Being knocked unconscious can cause a closed
head injury. About one third of all injury-related deaths in the USA are associated with a traumatic brain injury. This condition is
caused by the bruising or tearing of delicate brain tissue. The brain is a jelly-like substance
that is suspended in a bath of spinal fluid. It is protected by rubbery membranes called the meninges. Minor bumps on the head do not usually
cause any damage. But getting hit
hard enough to cause a loss of consciousness can cause serious injury to the
brain’s delicate tissues. Evidence
suggests that at any time during the lifespan, losing consciousness for more
than one hour triples a person’s risk for dementia.
A concussion is a temporary loss of
consciousness occurring after a blow to the head. The impact of the blow causes the semi-liquid brain tissue
to slosh about inside the skull, causing it to bruise. Like any bruise, the injured tissue
then swells. When the brain
becomes bruised and swollen, brain function can be disrupted for weeks after
the injury. This can cause loss of
memory, and sometimes results in permanent brain damage.
In younger people, most concussions are
caused by traffic accidents, but in the elderly they can also occur from falls,
or from being hit on the head by any object.
Immediately after a concussion, the victim
may experience confusion, memory loss, vomiting, and blurred vision. The longer the person is unconscious,
the more severe the symptoms tend to be.
About one-third of the people who experience
a concussion will exhibit post concussion syndrome. This condition includes chronic memory
loss, dizziness, and changes in behavior that can last over a year. Because most knocks on the head are
soon forgotten, the person usually does not connect the symptoms with the
accident.
Repeated concussions, such as those
experienced by boxers, can cause permanent brain damage, including a condition
called punch-drunk syndrome. One study revealed that 87 percent of former boxers showed evidence of
brain damage. We also know that a
significant number of those suffering from dementia have a history of head
injury.
Elderly people often bump their heads and
later forget that the incidents happened.
In a younger person, these bumps may be unimportant, but the brains of
elderly people are sometimes smaller, and slosh about inside the skull more
easily. The decreased amount of
neurons in the elderly brain makes minor damage more serious. Even small bumps on the head in the
elderly, such as a knock on the head from a cabinet door, can cause subdural hematoma (bleeding inside the
lining of the brain). Any
bump on the head should be checked thoroughly.
As soon as possible after a person has
experienced a loss of consciousness, she should see a doctor to rule out skull
fracture, brain injury, or subdural
hematoma. Subdural bleeding
is a serious condition that requires immediate medical attention. Weeks after a head injury, the person
may experience headaches, dizziness, changes in behavior, drowsiness, and
memory loss.
Dizziness
A common concern for people over 60 is falling. Balance and dizziness are common causes, however, it’s been my experience that
most people don’t really mean that they are dizzy. A great many people
who complain of dizziness are suffering from Parkinsonian difficulties;
that is, if they lose their balance, they cannot regain it, and they may fall.
Others use the word dizzy to describe muscle weakness or damage that results
in unsteadiness, and causes the person to fall or bump into things.
Some people are actually experiencing the results
of orthostatic hypotension, a sudden drop in blood pressure upon
standing. This means that
when they stand up too quickly, they feel faint. This drop in blood pressure can be caused by medications or
chronic low blood volume. Low
blood pressure can also be a sign of internal blood loss, which is a serious
condition. Still others are dizzy
because of vestibular disorders – malfunctions in the balance apparatus
in the ear that result in a feeling that the room is spinning around. Also known as vertigo, this can
cause nausea and panic attacks.
This can be caused by ear infections or damage to the balance organs
themselves.
Dehydration
Thirst is the sensation caused by dehydration. The third part of the brain, the brainstem, connects the brain to the spinal cord which controls hunger and thirst. The sense of thirst is mediated by sensors called baroreceptors. They are located in the aortic arch and carotid sinus, and are stimulated by reduced fluid intake.
The continuing loss of fluid through the skin and lungs and in the urine and feces requires that fluids need to be replenished throughout the day. As people age, baroreceptors decrease, and the sense of thirst becomes impaired. When older adults (aged 65 to 74) and young adults (aged 21 to 30) were given salty water to make them thirsty, the elders drank half as much water as the younger subjects.
Older people are often reluctant to drink water because of incontinence. High water content foods like popsicles and gelatin improves hydration.
Mold can increase thirst and cause frequent urination
Psychotherapy is very useful in improving the quality of life of older adults. However, the most overlooked and undervalued causes
of behavioral and emotional problems are inadequate or poorly balanced
nutrition and the nutritional deficits that come with aging. Therefore, a nutrition assessment should be done before any intervention.
As people age, they often have deficits in
their senses of vision, smell, and taste, decreasing their enjoyment of
food. Elderly people also have a
tendency to narrow the scope of what they will eat, and therefore may become
deficient in certain vitamins and minerals. Often, because of financial difficulties, they consume less
protein and increase the consumption of refined carbohydrates, which can
destabilize blood sugar.
Volatility of blood sugar significantly increases the risk of dementia.
In some long-term care environments, meals
leave something to be desired.
Not only is food of poor quality, but dietary preferences are usually
ignored. In one facility where I
worked, 70 percent of the residents were Hispanic, but despite their
complaints, no ethnic food was offered.
Being forced to eat food the person does not enjoy, and having no choice
in what a person eats, results in non-compliant eating and inadequate
nutrition.
Older people may also lose their sense of
hunger. Hunger is physiological but appetite is psychological. It has been found that the
biochemical imbalances that cause anorexia in younger people and changes in the
natural aging of the brain are very similar. Drug withdrawal and depression may also cause geriatric
anorexia.
The consequence of brain changes combined with
unhappiness with menu choices often leads to inadequate intake of calories and
essential nutrients and a condition known as failure to thrive. In Amsterdam, Dr. Jan Berend Deijen has
observed that the level of daily functioning in geriatric nursing home patients
is related to both adequate nutrient intake and body weight.
Studies show that about 15 percent of older
people require professional intervention for failure to thrive. This condition includes a decline in
physical health, weight loss, loss of appetite, and social withdrawal in the
absence of any obvious cause.
Along with the physical decline, there is often depression, anxiety, and
confusion.
Making food more attractive does not have to
be expensive. In one study of food
intake in long-term care, residents were given a menu for each meal, which gave
them two entrée choices. Just
doing this increased caloric intake by 25 percent. In another study, adding natural flavoring to meals
increased intake and enjoyment of meals significantly. More flavor and aroma compensated for
taste and smell deficits that accrue with age.
Sadly, failure to thrive may also be the
result of neglect. I have worked
with families that literally starved their partners to death. A typical case of neglect was described
by Christine Williams-Burgess and Mary Kay Kimball.
Mr.
R arrived in the emergency room
with a questionable new stroke. He
was dehydrated and had lost 50 pounds.
He was unable to walk and was incontinent of urine and stool.
During
assessment, the patient confided that he felt he was a burden to his wife. He was embarrassed regarding his loss
of continence and felt badly that his wife “had to clean him like a baby.”
Mrs.
R thought that Mr. R was doing this on purpose. Thus, she would restrict food and fluids to decrease the
frequency of the episodes of incontinence.
Cases of neglect like this often come to
light when a patient improves rapidly in the hospital, and again deteriorates
when returned home.
Vitamins, Minerals and Other Nutrients
Vitamin Overdose
Vitamins and minerals are important for health. Vitamins minerals and other nutrients are often given to older adults, but overdose of these chemicals may contribute to polypharmacy.
Vitamin D
Low levels of vitamin D in the elderly may cause hip fracture.
Vitamin D is stored in the body; therefore, when taking more than needed, it will build up in the body. This may cause high blood pressure, high fever, irregular heartbeat and stomach pain.
B12 and Folic Acid
Folic acid and B12 levels are
found to be low in a large proportion of residents suffering from various
emotional problems, especially depression and anxiety, but deficits also
contribute to symptoms of disorientation, depression dementia, and psychosis.
Although B12 deficiency is common
in the elderly, measuring levels of B12 in the blood is not always
useful. B12 deficiency
may not become apparent until long after serum levels have been greatly
reduced, and symptoms have begun.
In order for this vitamin to be metabolized, it must be transported
through the small intestine by a chemical called intrinsic factor. Most people over 60 have significantly
low levels of this molecule, and therefore cannot absorb dietary B12. This means that even if they get
enough B12 in their diet, most elders will be deficient. For this reason, B12 deficiency should be assumed to exist in the majority of older people.
The most effective way to get B12 into
the bodies and brains of the elderly is by injection or by sublingual (under
the tongue) tablets, both of which bypass the gastrointestinal system. This should be a routine intervention
in all older patients manifesting psychiatric symptoms; however, in the real
world it is seldom done. Instead,
antipsychotics and antianxiety drugs are administered, which often cause more
problems than they cure. For
example, antipsychotic medication appears to increase the incidence of diabetes
in this population, and diabetes accelerates dementia. Also, antianxiety medications are the
number two cause of falls in the elderly, which are often lethal.
Folate and vitamin B12 can reduce the risk of hip fracture in elderly patients following a stroke.
B12 deficiencies are related to frailty, falls, cognitive impairment, failure to thrive, and enhancing aging anorexia and cachexia (weakness, muscle atrophy, fatigue).
In studies of elderly people with
depression, over 30 percent of subjects were also shown to be deficient in
folic acid. In another study, 67
percent of the residents admitted to a geropsychiatric hospital were deficient. As well as depression, folic acid
deficiency can also cause chronic forgetfulness, insomnia, anxiety, apathy, and
dementia-like symptoms. The
combination of B12 and folic acid reduces levels of homocysteine,
which reduces risk of cardiovascular disease, and raises levels of SAMe, a
natural antidepressant.
Niacin, Biotin, Pantothenic Acid
Both niacin (vitamin B3)
deficiency and biotin deficiency can cause or exacerbate depression, anxiety, and memory problems,
as well as cause emotional instability.
Pantothenic acid (vitamin B5) deficiency can cause
restlessness, irritability, and depression.
Thiamin
Thiamin (vitamin B1) deficiency
is very common among alcoholics, and can lead to a condition called Korsakoff's
psychosis, which causes profound memory loss, as well as depression, apathy,
anxiety, and irritability. B1 deficiency in the brain results in a condition called metabolic acidosis,
which upsets the neurotransmitter balance.
Vitamin C
In a few cases, chronic vitamin C deficiency
has been shown to cause both hypochondriasis (a preoccupation with bodily
symptoms) and depression. In
addition, vitamin C has been shown to interact with many central nervous system
receptors.
Calcium
Excessive milk-drinking, taking high amounts
of calcium supplements, steroid hormone therapy, and hypothyroidism can all
contribute to a condition called hypercalcemia, which may lead to
adverse conditions associated with calcium. Symptoms include fatigue, depression, anxiety, panic
attacks, headaches, paranoia, memory deficits, and insomnia. High intake of calcium also depletes
magnesium.
Magnesium
Diets high in phosphorus (found in
lunchmeats, hot dogs, and soft drinks) deplete magnesium. Thyroid hormones can also deplete
magnesium. The most common group
that experiences magnesium deficits is chronic alcoholics. Depression is related to both
alcoholism and alcohol withdrawal, and magnesium sulfate can often reverse this
type of depression.
Studies show that magnesium deficiency is
found in 25 percent of people with eating disorders such as obesity and
anorexia. Low magnesium levels
have been linked to many problems including loss of appetite, muscle weakness,
and cramps in the feet and legs.
Psychological symptoms include agitation, anxiety, depression,
hallucinations, insomnia, and confusion.
The recommended daily allowance for magnesium is 200 to 300 mg per day.
Potassium
Although the exact mechanism is not known,
excess potassium has long been associated with depression. This is often seen in uremic
patients. A deficiency of potassium
is also associated with depression and is most commonly seen in patients with
frequent vomiting or prolonged diarrhea, and in people receiving diuretics or
steroids.
Sodium
Elderly people with heart problems,
particularly those in cardiac failure, sometimes eliminate sodium from their
diets. Because of this, they may
develop depression. In these
cases, the addition of a minimal amount of sodium corrects the problem.
Metabolic Imbalances
Because of the nutritional deficits that
accompany aging, many people may overload themselves with nutritional
supplements, in the hope that taking mega-doses of certain nutrients will keep
them young and healthy forever. It
is a good idea to ask about the nutritional supplements, herbs, and other
self-medicating behavior the person is engaged in, as this is very common, and
will not be mentioned unless you inquire.
Supplements are not an alternative to proper eating.
Minor illness, such as the flu; dietary
habits; tobacco or alcohol use; and other factors that can affect lab values
are more likely to affect test results among the elderly. But because of the diversity that
accompanies aging, even though lab values outside of these ranges should be
considered as red flags for diagnoses, they do not necessarily indicate an
abnormality, nor do results within these ranges necessarily rule it out.
The experience of pain in the elderly has
been examined in two segments of the population – healthy older people, and
those suffering with medical illness.
The experience of pain is usually a consequence of injury or disease,
conditions that are more prevalent in older people, which makes pain a
significant detractor to quality of life.
Although the elderly are more prone to painful illnesses such as
neuropathy, trigeminal neuralgia, spinal degeneration, arthritis, and a variety
of other degenerative diseases, there is actually little evidence that pain
complaints are more common in the normal aged. Despite this evidence, the fallacy persists that pain is
an inevitable consequence of aging.
However, when it does exist, chronic pain
will often cause impaired activities of daily living, depression, anxiety,
lowered tolerance for frustration, problems with thinking and attention, sleep
disturbances, and irritability
Unfortunately, the belief that all older
people complain about pain can cause caregivers to ignore complaints of pain
and sometimes overlook serious pathology, including life-threatening
illnesses. Pain and suffering
should never be equated with the processes of normal aging, but should be
treated in an older person just as it is in the young.
In reality, elderly people may actually under-report pain because they too expect
pain with aging. In addition, those with communication difficulties or confusion
may be unable to make others aware that they are in pain.
The reporting of pain by someone who is not
actually suffering is called malingering. A true malingerer consciously fakes pain in order to get
medication, or to gain attention from family members or the healthcare staff. But even though many caregivers believe
that lying about pain is common, research shows that in the elderly, feigning
pain is actually very rare.
When a person says he is in pain, caregivers
sometimes feel the need to decide whether they should believe a person who on
other occasions has been untrustworthy.
Although there is no accurate test to detect a malingerer, and in some
cases we may disbelieve a person who claims to be in pain, professional
responsibility dictates that we accept the report of anyone who states that he
is in pain. It is better to treat
a malingerer than to deny treatment to someone who is suffering.
A professional assessment of pain should
never include a clinician’s personal biases, beliefs, values, or feelings about
the person.
Pain is a completely subjective experience –
there simply is no reliable way to objectively observe whether someone is in
pain. Because pain cannot be
observed, proved, or disproved, the only basis for pain assessment is the
patient's subjective report that he is in pain. For this reason, the most useful criterion for definition
is, “pain is whatever a person says it is, and exists whenever he or she says
it does.”
In the 1986 edition of Cancer Pain
Relief, the World Health Organization states unequivocally, “Believe the
patient’s complaints of pain.”
In other words, a report of pain by a patient should be sufficient to
establish pain as a diagnosis.
This means that it is the person reporting the pain, and not the
healthcare team or the family, who is the final authority on the reality of
pain.
Acute pain is useful in that it warns us that the body has
sustained damage. The
distress that accompanies pain causes us to withdraw from the source of the
pain, and teaches us to avoid similar situations in the future. If tissue injury occurs, pain motivates
us to seek help. It also tells us
to remain immobile so that healing can occur.
However, chronic pain, also called unproductive
pain, is not useful in any way.
It only serves to diminish the quality of life. The distress from chronic pain serves
only to make the person suffer.
Chronic pain can sap enjoyment from a day, and eventually hamper one’s
will to live – and it is the most common type of pain found in the
elderly. About one out of five
elders suffers from chronic pain, and in the long-term care population, the
incidence of chronic pain can be as high as 80 percent.
Cicely Saunders, the founder of the hospice
movement, was the first clinician to see that chronic pain was
multidimensional. She felt that
this type of pain was a problem of symbolic meaning. Chronic pain, she felt, can be experienced by the victim as
never-ending, timeless, and meaningless.
This experience often leads to despair, social isolation, and
hopelessness. Hopelessness is the
greatest predictor of suicide in chronic pain patients.
Saunders also believes that pain was not an event,
but a situation in which the patients found themselves. Understanding this experience was
facilitated by listening to the patients’ stories of suffering. She believed that this was often a
portal to other problems which, when addressed, relieved suffering, Her concept
of total pain treatment included exploration of the physical,
psychological, social, emotional, and spiritual elements of the pain.
Treatment of pain included adequate pain
medication combined with the exploration of the person’s experience. This is accomplished by listening to
the person’s narrative about the experience, but also through exploring his or
her worldview, which included artwork portraying the person’s predicament.
Saunders also pointed out a problem that
still exists in treatment of the elderly – that 9 percent of terminally ill
people who die in hospice report pain, while 20 percent of those in long-term
care report pain.
Pain Tolerance
The tolerance of pain is best defined as the duration and intensity of pain that the person is willing to endure. Pain tolerance, pain perception,
and the expression of pain are all unique to the individual. Research shows that there is no such
thing as a general pain tolerance.
Some people just feel more pain than others do.
For this reason, the duration or severity of
pain can’t be predicted. Simply
put, you cannot be the judge of what should be painful to someone, or how long
it should hurt.
Many caregivers believe that the more
experience a person has with pain, the more endurance and the greater tolerance
they will develop. In fact, people
who experience chronic pain usually have a lower tolerance combined with
a higher level of anxiety because they know how severe the pain can be and how
hard it may be to get relief.
Furthermore, a person’s tolerance for pain
varies from one situation to another.
A person’s emotional state and degree of fatigue, and the value or
meaning of the pain for that person all play a part in the tolerance to pain.
Pain Threshold
A person’s pain threshold is the
point at which a stimulus is perceived as painful. Many caregiving professionals mistakenly believe that
everyone perceives pain the same.
In addition, over time, seasoned health-care workers often develop their
own conclusions about the range of expected pain responses for certain
situations. This can cause
problems because a patient who experiences more pain than expected with a
certain treatment, diagnostic procedure, or in a postoperative recovery period
can become labeled as “exaggerating” his pain.
For example, surveys show that most nurses
expect that the most severe pain following surgery will occur in the first 48
hours and then gradually subside.
However, in a recent study of post-surgical patients, 31 percent
reported significant pain after the fourth postoperative day.
Researchers Helme & Gibson have found
that in healthy elders, pain threshold increases with age – with pain thresholds
increasing about 20 percent by the eighties. Older brains seem to be less sensitive to peripheral
input. Gastrointestinal pain
threshold also rises significantly with age, and for this reason, warning signs
of disease such as reflux or ulcers are often ignored.
However, pain threshold studies in the
“older old” (age 80 years and older) show high within-group variance. In other words, the older a person is,
the harder it is to predict his pain threshold. The perception of and reaction to pain in older people may
be determined by other circumstances in their lives, such as stress, anxiety, and depression.
Arthritis is the most common source of pain
in the elderly. Interestingly, in
the oldest old, more people report the disappearance of joint pain than the
onset of symptoms. This does not
seem to be correlated with the severity of their disease. It also appears that the peak of
musculoskeletal pain occurs after middle age. Arthritis and muscle pain does not improve with rest. In fact, rest can make the pain
worse. Furthermore, a person loses
one percent of his muscle mass for each day he remains inactive. Inactivity can lead to disuse
syndrome, and may result in the person losing the ability to walk.
The Causes of Pain
Another common misconception among health
care professionals is the belief that all pain must have an identifiable
physical cause. Because we
like to believe we have control, we believe that if a person has pain, there
must be an observable cause. If we
can’t find the cause, we inaccurately conclude that the person has no “real”
pain. However, all pain is
real, regardless of its cause and regardless of whether it can be diagnosed or
measured.
Lack of a physical diagnosis causes some
people to conclude that a person’s pain is psychogenic or “all in their
head.” However, there is no
evidence that purely psychogenic pain exists, and therefore all reports of pain
should accepted as valid despite a lack of an observable, physical cause.
As a result of this widespread belief that
all pain should be diagnosable, when there is difficulty establishing a cause
for pain, the sufferers themselves may begin to question their own sanity. They may begin to fear they will be
perceived as lying or malingering, and that pain relief will be withheld because
their pain is not real. For this
reason, it is useful to tell your patients that all pain is real, and will be
recognized as such.
All pain includes both a physical and an
emotional component. To have pain
that is purely physical – that is, the experience of pain without distress (a
condition called pain asymbolia) – is very rare. Therefore, feelings of fear and anxiety
are appropriate reactions to pain, and shouldn’t be seen as evidence that the
pain isn’t “real.”
All this being said, the social context in
which the pain is occurring should be considered. Secondary gain from chronic pain – that is, the
rewards one reaps from complaining of pain – includes increased attention from
staff and family. In fact, in some
cases, families and caregivers unwittingly encourage a sick role in a
person, attending to him when he complains, and ignoring him when he does not.
For others, the expression of pain may be an
attempt to cope with loneliness, fear of physical deterioration, or fear of
impending death. Focusing on pain
allows the person to avoid thinking about these unpleasant and frightening
things. In these cases, behavioral
intervention can be helpful.
Pain Behavior
Many health care professionals have been
taught to look for visible physiological and behavioral signs that accompany
pain, and therefore can be used as the basis for objective pain assessment.
With acute pain, physiological signs include
elevated blood pressure, rapid heartbeat, rapid breathing, dilated pupils, and
behaviors such as grimacing, moaning and flailing about.
With chronic pain, however, physical and
behavioral adaptation occurs, resulting in periods where the person may show no
overt signs of pain. As the body
adapts to pain, vital signs normalize after a period of time. This return to equilibrium is necessary
to prevent physical harm and stress on the body, but it does not necessarily
mean the pain has disappeared.
When caregivers follow the acute pain model
to assess pain, there will be times when a patient's behavior and physical
signs do not correlate with the patient's report of pain. Patients may experience even severe
pain without acting as if they are in pain. In other words, lack of pain behavior does not mean lack
of pain.
A recent study shows the effect that behavior
can have on pain assessment. In
the study, nurses were told to rate the pain of two patients recovering from
identical surgical procedures.
Although the surgeries were identical, one of the patients smiled, while
the other grimaced. Even though
their behavior was different, the patients both reported that they had exactly
the same amount of pain.
Interestingly, in both cases, many of
the nurses underestimated the amount of pain the patents reported, but the
estimates were even lower for the smiling patient. This indicated that the nurses had relied on their
expectations of the patient’s pain and his behavior and appearance rather than
on the person’s actual report of his level of pain.
Attitudes about Pain
In America, we have an unrealistic and stoic
attitude about pain. Most of us
feel that people should be able to cope with pain, and that to ask for help is
a sign of weakness. This causes
many caregivers to underestimate the severity of pain in those who report it,
and to adopt the attitude that the person should “just learn to live with it.”
This attitude also causes many people in
pain to refuse medication that could help them because they don’t want to
appear to be “weak.” I have had
many people tell me they don’t complain about pain because they want to be a
“good patient,” or they feel that a stoic response to pain or exhaustion
somehow makes them a better person
As a clinical psychologist, I have never
been a strong proponent of medication, but I think we are very wrong-headed and
ignorant about pain treatment in this country. Too many people suffer needlessly because of our negative
attitudes about pain medication.
In addition, many physicians are reluctant
to prescribe pain medication out of fear of repercussions from federal
agencies, which also have this unrealistic attitude about medicating pain. A doctor who doles out pain medication
liberally is often red-flagged, and called on the carpet for his or her
“excessive” prescribing habits.
This must change.
Another barrier to medicating pain is the
unrealistic fear of addiction.
Despite an abundance of evidence that narcotic drugs do not cause
addiction in pain patients, many health care professionals persist in believing
that addiction is a problem.
A survey of 1,781 nurses done in 1989 showed that 31 percent of them thought
pain-killing drugs should not be given because of potential addiction. Because
of this mistaken belief, many health care professionals continue to refuse these
drugs to those who need them. Others minimize the amount of pain medication
a person can receive, making the therapy useless. These attitudes are archaic
and harmful.
Effectively eliminating pain can do wonders
for a person’s quality of life.
The priority for patients should always be comfort, not courage.
It has also been found that many chronic
pain patients, including cancer patients, refuse to take opiate-based pain
medication because they believe that they would develop tolerance to the drugs,
and therefore the drugs would become ineffective. In reality, opioid drugs have no “analgesic ceiling” – that
is, the level of these drugs can be increased to effective levels.
Finally, many health care workers
underestimate the severity of the person’s pain, and overestimate the
effectiveness of the medication they are giving. If a person who has received pain medication a few hours
before claims that they are still in pain, they are often told, “I’m sorry, you
just got a pain pill. You’ll have
to wait two more hours.”
This is equivalent to telling the patient that you think they are lying.
Pain and Depression
In the elderly, pain and depression may be
closely linked – pain can be exacerbated by coexisting depression, while many
who experience chronic pain often become depressed and anxious.
Studies show that up to 59 percent of
patients requesting treatment for depression also complain of recurring pain,
and conversely, 87 percent of patients coming to chronic pain clinics exhibit
the symptoms of depression.
Even when people deny being depressed, they
may exhibit the symptoms. In fact,
most people are unaware of the symptoms of depression, and do not realize that
depression can worsen pain. Common
symptoms of depression include sleep disturbances, early morning awakening,
psychomotor retardation or agitation, anorexia, and weight loss.
In some cases of unrecognized depression,
complaints of pain may be the person’s way of explaining her loss of interest
in life, her low energy, poor concentration, and guilt. In cases where pain complaints are
accompanied by the symptoms listed above, behavioral interventions can
help. Several studies have shown
that chronic pain can cause cognitive problems. In fact, in one recent study, the central processing speed
(the time it takes to think) in chronic pain patients was significantly slower
than in head injury patients. Pain
interferes with attention, concentration, and endurance, and can preoccupy a
person to the degree that he cannot think clearly.
Interestingly, although cognitive impairment
may be a barrier to pain assessment, it is important to recognize that even
cognitively impaired residents reliably report the presence of pain when they
are asked.
Medications
The elderly spend four times as much on
medications than the rest of the population. People over age 65 comprise 12 percent of the population,
but take 30 percent of all prescribed medications. The average number of drugs prescribed to people over sixty
is fifteen per year. Two-thirds of
this population is taking at least one prescription drug. Thirty-seven percent are taking at
least five drugs, while another 20 percent are taking seven or more medications
at once. The majority are also
taking herbs, vitamins, and supplements.
Medication problems
In his book, The People's Pharmacy, Joe Graeden claims that thousands
of cases of confusion, mood disorders, and memory problems are actually a result
of the toxic effects of over-medication. He calls this problem the “spaced-out
Grandma syndrome.”
Common Side Effects Of Drugs
Depression:
- antibiotics
- ulcer medications
- steroids
- anti-glaucoma eye drops
- cardiovascular drugs
- anti-Parkinson's drugs
- anti-epileptic medications
- Advil
- Naprosyn
- Indocin (for arthritis)
- Antabuse
- Hytrin (for benign prostatic hyperplasia)
Psychosis:
- antibiotics
- urinary tract infection drugs
- analgesics
- aspirin
- Darvon
- cold medicines
- Actifed
- Benadryl
- Albuterol (for asthma)
- cardiovascular medications
- antidepressants
- tranquilizers
- Vincristine (for cancer)
- Sinemet (anti-Parkinson’s)
Dementia:
- Zantac
- Axid
- Pepcid
- cardiovascular drugs
- central nervous system drugs
|
|
This is not a small problem; in fact, it is
estimated that over 200,000 people in this country are currently suffering from
medication-induced mental problems.
Each year, adverse reactions to prescription drugs, drug misuse, and
medication abuse account for thousands of illnesses and deaths in the elderly.
One woman who came to see me was taking
seventeen prescription medications!
These drugs were given to her by several doctors for various ailments
she had suffered over a period of years, but it seemed that no one had ever
asked her if she was taking any other medication. Furthermore, none of the doctors told her when to stop
taking the medication, so she continued to take medicine for ailments that had
disappeared long ago.
Most older adults will take any medication that their
doctor recommends, without question.
The majority do not know the names of the
medicines they are taking, or why they are taking them.
An adverse reaction is an unexpected and
unwanted response to a drug that results in illness, organ failure, or
death. Drug misuse is the
under use, overuse, improper use, or erratic use of a medication. Drug abuse is the use of a drug
for other than its intended purpose.
It’s important to understand that any drug
that has a therapeutic affect can also have an adverse effect on a person. Unfortunately, up to 90 percent of
people over 65 will suffer side effects from medication at some time in their
lives.
Drugs act differently in older people. They are more prone to idiosyncratic
and paradoxical reactions. The
loss of brain cells and the lower amounts of neurotransmitters in the older
brain can amplify the effects of many medications, and doses that are safe for
younger people are often toxic in the aged.
Older bodies take much longer to metabolize
and excrete certain drugs.
Decreased liver and kidney functions increase the risk of drug
toxicity. In short, all medications
should be given with care and be closely monitored. In many cases, dosages need to be decreased.
SSRIs or SNRIs given in high doses to older patients may cause an increase in fragility fractures.
For these reasons, any symptom in an elderly
patient should be considered to be a drug side effect until proven otherwise.
The medical community has not done an
effective job in tackling this problem.
Almost 65 percent of elders are not told by their doctors about
precautions in using medications, and 67 percent are not told anything about
possible side effects.
In many cases, the prescribing physician did
not know about the potential adverse effects of the medication, and was not
aware of the interactive effects it could have with other medications the
patient was taking.
Over a third of elderly people make serious
mistakes in taking their medication – either forgetting to take it or
forgetting that they have taken it, and therefore overdosing.
Even worse, about 12 percent of people
taking prescription drugs are using medications that were actually prescribed
for someone else. They
accidentally take medicine that is not their own because they can’t read the
label, or because they got it from a friend who said it “worked for him.”
Although most people do not realize it, many
over-the-counter medications can also significantly interfere with memory,
mood, and thinking. Even so, few
if any of these medications indicate cognitive impairment as a side
effect. Doctors don’t often
explain to their patients that the drug they are prescribing may have an effect
on their memory or thinking.
In addition to experiencing problems with
drugs, many people resort to alternative medicines, vitamins, herbs, and other
over-the-counter remedies to help them with their various maladies. This becomes problematic because most
people don’t let anyone know what they are taking.
Always ask the person to tell you about everything they are taking. Ask them
about prescription drugs, non-prescription drugs, vitamins, herbs, nutrients,
and other alternative remedies. Ask them about any allergic reactions or adverse
symptoms they have experienced in the past. If you don’t ask, you will
not be told.
Medication Misuse
Misuse is using a drug improperly, which may include overuse, use for the wrong
reason, or using a medication when it is no longer needed. Commonly misused prescription drugs
include sedative-hypnotics (sleeping pills), anti-anxiety agents (such as
Valium and Xanax), and analgesics (such as Oxicodone). When misuse rather than abuse is
suspected, drug education groups and clear instructions about the use of the
medication are usually effective interventions. When a person is abusing a drug, however, things get more
complicated.
The elderly not only use prescription drugs
three times as frequently as the general population but also have the poorest
rates of compliance with directions for taking medications. For these reasons, abuse of
prescription drugs may actually be the most common type of drug abuse.
Because of changes in metabolism, and kidney
and liver function, older people should be prescribed lower doses of
medications. Despite this, data
from the Veterans Affairs Hospital System suggest that elderly patients
routinely are prescribed inappropriately high doses of benzodiazepines, and
that the drugs may continue to be prescribed for longer periods than in younger
adults, which results in overdosing, inducing altered consciousness, and
increasing the risk of dependence.
Because of this, Valium (diazepam), Xanax, and Dalmane (flurazepam) are
some of the most common drugs of abuse in this population.
There is a sex bias problem in prescribing
medications that further exacerbates problems. Studies show that women are more likely than men to be
prescribed narcotics and anti-anxiety drugs – one study touting a 48 percent
higher likelihood. Women are also
two times more likely to become addicted to sedative, hypnotic, or anti-anxiety
medications.
Cognitive impairment often occurs with
benzodiazepine use, manifesting as symptoms that mimic and are often mistaken
for dementia. But worst of all,
elders who take these medications are at increased risk for falls that can
result in hip and thigh fractures (as well as for vehicle accidents). In fact, these medications are the
number two cause of falls in the elderly.
Hip fracture can be lethal in the frail elderly. Of those who do survive, many undergo
hip surgery, which frequently results in significant irreversible decrease of
mental status.
Substance abuse among the elderly is a very
common but often undetected problem.
Older people rarely seek help for drug problems.
Even though the elderly are at highest risk
for drug misuse and abuse, the problem is chronically under-diagnosed. Although it is not well known to the
public, alcohol-related problems in the elderly cause as many deaths as heart
attacks.
Initial research on elder substance abuse suggested
that the prevalence of alcohol abuse and dependence in adults 65 years of age
and older was low – about 2 to 5 percent for men and about one percent for
women. Other studies estimate that
between 2 and 10 percent of individuals over the age of 60 suffer from
alcoholism, and in a survey of elderly patients in Washington State, 9.6
percent were diagnosed with alcohol abuse, while about 5 percent were referred
for prescription drug abuse.
However, since that time researchers have discovered that these numbers are
probably an underestimation because the majority of substance-abusing older
people lie about drug and alcohol use, and deny any problems when asked. In
surveys of drinking habits in the elderly, those who admitted drinking routinely
under-reported the amount of alcohol consumed.
It is easier for the elderly to conceal
their drinking because they don’t work, have few social commitments, and may
avoid social contact without consequence.
Recent research suggests that retirement communities may foster
substance abuse because the communities isolate elders from the general
population, and a person who does not interact with others in the community is
seldom scrutinized. Because people
who live in these communities buy or lease their property after they retire,
the community is made up of strangers.
There are few, if any, long-term friends who would notice changes in
behavior. They are not monitored
and have no obligations or responsibilities, and therefore can stay in their
homes intoxicated for long periods of time with no social consequences.
Chronic alcohol consumption leads to medical
and psychological problems. For
example, excess alcohol consumption is linked to malnutrition, because heavy
drinkers seldom eat a balanced diet.
Chronic consumption of alcohol also decreases the ability of the stomach
to absorb nutrients. Another
alcohol‑related problem is osteomalacia, or thinning of the bones. Over time, drinking results in
cirrhosis of the liver, which is now one of the eight leading causes of death
in older adults.
The most frequent and serious problem with
chronic alcohol use in older adulthood is a decline in cognitive
functioning. Chronic alcohol abuse
may lead to major declines in memory and information processing.
Over many years of alcohol abuse, the
effects of these physical and cognitive changes lead to significant impairment
in most persons who survive past middle age. The same is true for those who begin to drink heavily in
later life.
There is 60 percent correlation between prescription
drug abuse and alcoholism.
Psychosocial factors such as loneliness and depression, and health
factors related to the aging process, such as pain, disability, or chronic
disease, are the major contributors to alcoholism and drug abuse in older people. Combining alcohol and drugs, especially
tranquilizers and sleeping pills, is especially dangerous, as there may be a
cumulative depressant effect on the central nervous system.
Risk factors for alcohol abuse among all
adults include genetic predisposition, being male, limited education, low
income, and a history of psychiatric disorders, especially depression.
Stressors are more important contributors to
late onset alcohol and drug abuse than to early onset abuse. Common stressors that contribute to
alcohol and drug abuse in later adulthood include retirement, relocation,
conflict within the family, financial concerns, physical health problems, and
death of a spouse. Older widowers
have the highest prevalence rates of alcohol abuse among older adults.
The stigma attached to chemical dependency
problems in older persons fosters denial and makes it difficult to determine
the extent of dependency.
Individuals often enable their chemically dependent spouses out of a
sense of duty, thus increasing the likelihood of denial.
The elderly are often viewed as poor
treatment risks because society sees them as physically, mentally, and
economically unstable. However,
successful treatment and recovery are highly possible for this population if
intervention and treatment are positive and get to the root of their
problems. During intervention and
treatment, it is important to build social support networks for the
elderly. Programs that reinforce
skills and focus on reducing isolation decrease the risk of relapse. Involving spouses and other family
members in the treatment process will educate everyone about the effects of
chemical dependency on the older person, and its effects on family
relationships.
A thorough assessment is essential to detect
and correct drug misuse and to diagnose drug abuse. Prior to considering any medication, the person must be
screened for alcohol and drug use, as this will cause medical complications and
put the person in peril. Ask about
an individual or family history of alcohol or other drug abuse.
Contrary to popular belief, sexual behavior
continues throughout the lifespan.
In this culture, the belief that elderly people should be nonsexual is
especially true about older women.
Studies show younger people look unfavorably on aging women as being
physically attractive and sexually active. This set of values does not apply to older men.
The greatest barrier to sexual activity in
the elderly is lack of an available partner. In the 65-74 age group, only 9 percent of men are widowed
but 42 percent of women are. Older
women are also less likely to remarry, while elderly single men often marry
younger women.
In addition, elderly women experience more
losses at widowhood than do elderly men.
Many women tie their identity and self-esteem to marital roles, while
most men tie their identity to their work.
Depressive symptoms are associated with poorer sexual health. Retirement is also a problem Because many men do tie their identity to their work, retirement often brings on depression and adjustment disorders, which can make life difficult for both partners. Another problem is the significant change in time spent together, and the concomitant disruption in lifestyle and routines. Marital conflict often increases, anger and hostility emerge, and, consequently, sexual desire may lessen.
The strongest predictor of the frequency of
sexual activity in the elderly is the level of activity in their younger
years. The marketing of
medications to increase potency has increased the frequency and enjoyment of
sex for thousands of elders, however, it has also increased the risk of stroke
and heart attacks, as the vascular insufficiency that impaired erections may be
indicative of cardiovascular disease.
It is often thought that HIV only affects younger people. Many older people do not realize that they may acquire the virus.
It’s important to note that the rates of HIV
infection are growing rapidly in the population. Currently 10 percent of HIV cases are found in people over
50, and 5 percent of cases are in those over 65. Between 1991 and 1996, the increase of HIV was 97 percent in
men over 50 and 106 percent in women over 50. This may be in part because lack of concern about pregnancy
lessens the perceived need for safe sex.
Older people are rarely checked for
syphilis. Tertiary syphilis can
present as dementia and should always be considered as a cause of cognitive
disarray.
Sleep
Medications That Cause Sleep Problems
- Antibiotics
- Amantadine
- Gastrointestinal drugs
- Inderal
- Drugs containing caffeine
- Drugs containing Ephedrine
|
|
With increasing age comes a change in
sleep. In general, older adults
take longer to fall asleep, have multiple nighttime awakenings, and require
more daytime naps. The most common
sleep complaints in the elderly are difficulty sleeping throughout the night,
waking up earlier than they would prefer, and feeling that they have not gotten
enough rest.
Other common phenomenon is a circadian drift
into becoming a “morning person.”
There is a tendency to go to bed earlier and wake up earlier. Nevertheless, for many, even when they
do go to bed at the same time that they did when they were younger, they will
wake up earlier, thus depriving themselves of adequate sleep.
Loss of hearing and sight can also disrupt
sleep. For example, many blind
people have a free-running biological clock, which causes regular periods of
insomnia and hypersomnia every three weeks, because sunlight does not rest
their biological clock.
Contributors to Sleep Changes
- Less light exposure
- Lower social demands
- No work schedules to structure the day and maintain arousal
- Less physical exercise
|
|
Older people with sleep problems experience
a diminished overall quality of life.
There is also a greater prevalence of depression and anxiety. Older people who have sleep complaints
also show slower reaction times, problems with balance, and impaired
memory. Cognitive function is also
impaired, and sleep problems may be misdiagnosed as dementia.
Aging Changes in Sleep
- Stages I and II increase
- Wake time after sleep onset increases
- REM latency decreases
- Stages III and IV decrease
- Daytime sleepiness and napping increase
- Changes in the central nervous system circadian oscillators
|
|
Insomnia is very prevalent in people
experiencing stressful life events including loss, bereavement, or a move. As these events are common in the
long-term care population, they should always be considered as primary causes
of sleep disturbance.
Other common factors that affect sleep
include noise, uncomfortable temperature, lighting problems, and bedding. Many studies in sleep problems in the
elderly point to these factors, particularly in a long-term care setting, where
people may share a room with others who have different sleep cycles, who snore,
or make noise during the night.
Temperature, light, and bedding preferences are seldom asked about or
attended to, and cause uncomfortable sleep environments.
A common and potentially dangerous sleep
problem in the elderly is sleep apnea. This is caused by an obstruction in the airflow during
sleep. A person suffering from
apnea may actually stop breathing for more than a minute. Most people with sleep apnea snore, and
sleep poorly. During the day, they
are fatigued and listless. This in
itself is troubling, but even more troubling is the mounting evidence that
apnea can cause dementia.
Sleep researcher Sonia
Ancoli-Israel found that among 235 nursing home patients, virtually all with
severe sleep apnea were also severely demented. Seventy percent of the patients had five or more respiratory
disturbances per hour of sleep and 96 percent showed some dementia. Sleep apnea was significantly
correlated with all subscales on the dementia rating scale.
Mild to moderate apnea caused no problems,
but the study showed a strong relationship between dementia and sleep apnea
when the sleep apnea and dementia are severe. It is thought that sleep apnea causes deficits in brain
function, possibly due to global effects rather than any particular cortical or
subcortical structure. If this is
so, treating residents for apnea could significantly reduce dementia symptoms. Fortunately, this condition can usually
be remedied.
Still another concern is the finding that
sleep apnea, or any type of breathing abnormality during sleep, has been shown
to increase the level of agitation in people suffering from dementia.
The continuous positive airway pressure (CPAP) represents the treatment of choice. Although many people do not like the CPAP at first, most find significant improvement in activities of daily living.
Delirium
People who are delirious have problems with focus and sustaining attention, Delirium, also called acute confusional state, is most often caused by acute illness or drug toxicity, and always involves periods of diminished consciousness. It may be caused by fever, organ failure that leads to toxicity, or any acute infection. The most frequent cause of delirium in older people is a urinary tract infection, and this should always be assessed and ruled out when establishing the cause of diminished cognition. The delirious state is usually transient and fluctuates in intensity throughout the day.
Delirium develops over a short period of time, typically hours to days. It is a sign of danger, and if not
treated, often is a warning sign of death. In the majority of cases, the person recovers within a few
weeks. However, in elderly
patients, delirium lasting up to 6 months is not uncommon, especially when
arising because of chronic liver disease, a carcinoma, or endocarditis. This prolonged delirium is sometimes
mistaken for dementia, but the differential diagnosis is the observation of
fluctuating level of consciousness.
A majority of older people will develop
confusion or delirium just by entering a hospital. They may also decompensate when relocated.
The Impact of Memory
and Cognitive Decline
 Findings from
the 2000 Medical Research Council Cognitive Function and Aging Study suggest that the relationship between “normal” brain aging and the dementias is
best represented by a continuum.
In the study, the brains of 209 older people (of which 100
met the clinical criteria for dementia) were examined to distinguish a normal
aging brain from that of one suffering from dementia.
Findings from
the 2000 Medical Research Council Cognitive Function and Aging Study suggest that the relationship between “normal” brain aging and the dementias is
best represented by a continuum.
In the study, the brains of 209 older people (of which 100
met the clinical criteria for dementia) were examined to distinguish a normal
aging brain from that of one suffering from dementia.
Brains of demented and non-demented subjects
overlap in the amount of vascular lesions, plaques (found in all Alzheimer’s
disease patients), and plaque density.
Studies show that no single pathological criterion reliably
distinguished between demented and non-demented groups. While vascular lesions did not provide sufficient explanation for the presence of dementia, they did suggest
that the interaction between Alzheimer’s pathology (plaques and tangles) and vascular insufficiency is the strongest determinant of the onset of
dementia. The concept of a
continuum has been suggested by many researchers, who believe that cognitive
and memory deterioration can be divided into three broad categories:
- Age-associated
memory impairment
- Mild
Cognitive Impairment
- Dementia
Age Associated Memory
Impairment
Age-associated memory impairment (AAMI) is a
gradual decline in encoding new memories and retrieving old ones. People who experience AAMI have
subjective memory complaints disturbing everyday life.
The most common manifestations of AAMI are
benign but bothersome difficulties such as forgetting names, losing belongings,
difficulty recalling a list of multiple items, and problems with tasks that
require multiple actions. There
also may be difficulty remembering telephone numbers and zip codes. If the individual is distracted in some
way, the problem is compounded, making it even harder to remember things such
as what he intended to buy at the store.
AAMI may also manifest itself as subtle deficits in executive functions associated
with frontal lobe function. This may slow thinking, reduce tolerance for frustration,
and cause the person to seek reduced levels of stimulation. The Alzheimer’s Association and the American
Health Care Association are currently studying AAMI to determine whether those
with age-associated memory impairment will eventually develop Alzheimer’s
disease.
Although this research is ongoing, most
researchers now consider age- associated memory impairment to be a benign
condition which is not a predicator of dementia – AAMI seems likely to be a
phenomenon of normal aging rather than a continuum from normal aging to a
pathologic state such as Alzheimer's disease.
A survey sponsored by General Nutrition
Centers revealed very low awareness of AAMI among those who may suffer from the
condition. Although AAMI is a very
real condition, the majority of survey respondents (71 percent) had never heard
of it. Two-thirds of the
respondents insisted they did not suffer from it even though they reported such
typical symptoms as forgetting names, phone numbers, day-to-day tasks, and even
important events.
Researchers do not yet know the exact cause
of age-associated memory impairment.
However, there are things that contribute to memory change and/or
loss. One of the causes is chronic
lack of mental stimulation.
Findings suggest that if a person becomes more mentally active and takes
steps to keep her brain healthy, memory will improve.
Because AAMI and Mild Cognitive Impairment
(MCI) are relatively new concepts, researchers are still attempting to define
and delineate the terms. MCI is
considered to be more serious than age-associated memory impairment, but not as
serious as dementia.
An example of the difference between the two
would be a person with AAMI occasionally forgetting the name of an acquaintance
for a few seconds. In contrast, a
person with MCI would repeatedly struggle to remember the names of close
colleagues, which might begin to interfere with his everyday life.
Other signs of MCI include difficulty in
forming memories of events that just happened. On a recall test, a person may be able to repeat a string of
unrelated words, but then fail to remember even one of them 10 minutes later.
No one knows how many people experience this
condition. While an estimated five
million Americans have Alzheimer’s disease, studies to determine the incidence
of this milder deficiency are only starting.
Unlike AAMI, Mild Cognitive Impairment is
now thought to be a condition that frequently precedes Alzheimer's
Disease. It is defined as a
transitional phase between normal aging and dementia. One study estimates that between 30 and 50 percent of
persons who develop Mild Cognitive Impairment will contract Alzheimer’s disease
within five years.
Individuals confronted with this prediction
may feel as though they are numbers on a roulette wheel, and if theirs comes up
when the spinning stops, they are fated to lose their memories. While acknowledging the importance of
new studies that give physicians a clearer picture of how many new victims of
memory loss to expect, I believe that such announcements create unrealistic
fears because they offer no alternatives.
The truth is that if MCI can be detected, it
may be treatable. Preliminary data
suggests that people with MCI should begin intervention and treatment as soon
as the diagnosis is made.
Currently, the government's National
Institute of Aging is engaged in a multi-university study to test the
effectiveness of drugs (e.g., Aricept™), and natural approaches including
vitamin E, ginkgo biloba and others.
Therefore, while the predicted statistics may be accurate, at least half
of those who develop MCI can not only overcome it, but may also prevent the
onset of Alzheimer’s by using corrective measures.
The word dementia means literally to
lose one’s mind. Dementia is a
syndrome of brain dysfunction characterized by multiple deficits in cognitive
abilities without loss of alertness (a loss of alertness occurs in delirium).
In 1900, there were 3 million people over 65
in the United States. At the time
of this writing, there are about 35 million, and this number is expected to
double by the year 2050. It is
estimated that one percent of people between the ages of 65 and 74 years old,
seven percent of those from 75 to 84 years old, and twenty-five percent of
those over 85 will suffer from severe dementia. Currently about 2 million people in the US suffer from
advanced dementia, while another 5 million suffer mild-to-moderate symptoms. However, these data may be underestimates,
as some researchers feel that more than half of the people suffering from
dementing illness are never diagnosed.
Dementia is caused by brain damage. The parts of the brain that are
most affected are the association areas of the brain, which integrate sensory
information, thought, memory, and purposeful behavior. When extensive damage to these regions
occurs, the person may begin to engage in bizarre behaviors that have no
external link to the environment.
They may also become verbally and physically agitated and abusive.
Dementing illness always includes the loss
of memory and cognition. It
also causes the loss of the ability to make sound judgments, and to maintain an
ongoing sense of being. Very
often, the ability to comprehend and express ideas is also impaired. In addition, there are problems with
social interaction, daily living skills, and thinking.
The word “dementia” is the loss of brain function which occurs with certain diseases. It affects memory, thinking, language, judgment, and behavior.
There are over 60 known disorders that cause
dementia, but Alzheimer's disease, which is also often referred to as Dementia
of the Alzheimer's type (DAT), accounts for over half of all cases. Vascular dementia (previously called multi-infarct
dementia,) accounts for another twenty percent. Fronto-temporal dementias, (including Pick's disease)
account for about 5 percent.
Criteria for the diagnosis of dementing
illness are:
- A
significant decline in cognitive abilities from baseline level
- Deficits
in multiple cognitive realms (memory, thinking, decision-making, and
language)
- A
clear sensorium (sensorium is impaired in delirium)
Reversible Dementias
Although dementia is usually thought of as a chronic, progressive loss of mental function, many people suffer from potentially reversible dementias. The most common cause of reversible dementia is reaction to medication, i.e., prescription, over the counter, or polypharmacy. Other causes are brain tumors, thyroid problems, low testosterone, infections, sepsis, toxins, nutritional deficiencies, metabolic problems, and neurological disorders.
In 2014 PubMed published 1165 research papers on reversible dementias. There is evidence that one out of four older people diagnosed with dementia does not have it. This is often because of sloppy diagnosis, or confusing medical or psychological disorders with dementing illness. It is also important to distinguish the existence of a mental disorder from the symptoms of dementia, because mental disorders often mimic the symptoms of dementia, yet are often treatable. In addition, when a person is suffering from dementia, the existence of other mental disorders may worsen the symptoms. The 2012 ICD-9-CM Diagnosis Code 290.21 is “Senile dementia with depressive features.” The 2015 ICD-10-CM F03.90 is “Unspecified dementia without behavioral disturbance.”
While cortical dementias such as Alzheimer’s
usually cause aphasia (loss of language skills including word retrieval),
apraxia (problems with motor programs), and agnosia (trouble identifying and
naming objects), subcortical dementias most often present with intact language
and visuo-spatial function.
Subcortical dementias include Parkinson's, normal-pressure hydrocephalus
(NPH), multi-infarct dementia, Huntington’s disease, and Binswanger’s disease. Of these dementias, only
normal-pressure hydrocephalus is potentially reversible.
The Stages of Dementia
Early Stage
If you have ever walked into a room and realized you had no idea why you were
there, you have an inkling into how demented people experience their entire
day.
In the early stages of dementia, the loss of
ability to think and remember becomes intermittent and patchy – the afflicted
person may forget who you are on Monday, but have no trouble recognizing you a
day later.
A person in the early stage of Alzheimer's
disease may begin to show a loss of interest in his environment and in his
personal affairs. Word-finding
becomes difficult, usually beginning with the inability to remember names, and
then nouns. He may have difficulty
in attending to important social events, such as holidays or birthday
parties. Social graces,
politeness, and social protocols begin to break down. For example, one of my patients went home in the middle of
his birthday party because he did not remember why he was there, and decided it was time to take a nap.
People in this stage suffer uncertainty and
confusion in initiating actions. A
thought occurs to the person to do something, but a moment after they begin,
they have forgotten what they intended to do. They may pick up an object with clear intent, and find
themselves wandering around with it, not remembering what they meant to do.
At this stage of the illness, people may be
able to live at home with supportive care. But even though they appear to be thinking clearly, they
will usually need assistance in paying bills and managing money. Frequent assistance is especially
important if the person lives alone.
Proper health care, vitamin E, Vitamin B12, non-steroidal anti-inflammatory drugs, and anticholinesterase inhibiting drugs
– along with the reduction of environmental change and stress – can reduce
symptoms, slow the disease process, and prolong independence at this stage.
Although a person in this stage of the
disease may still be able to drive, he may become easily lost, and forget his
way home. Neighbors and friends
can assist by being aware of any change in living habits that warrant increased
vigilance. Relocation, change in
residence, or illness will often be the point at which the patient slips into
the next stage.
Intermediate Stage
As dementia progresses there is a loss of
what health care providers call activities of daily living (ADL). Health care and personal hygiene are
neglected. The person shows
diminished ability to care for personal needs or affairs. There is also a loss of ability to
comprehend, remember, or follow simple directions. As motor programs begin to break down, the person may engage
in meaningless behavior.
There are obvious memory problems in recall,
recognition, and retention. As
memory loss continues, most of the simple tasks of life – like bathing,
brushing teeth, or getting dressed – become confusing and incomprehensible, and
require aid from others. Even
something as simple as putting on a shirt may become overwhelming.
Biological clocks begin to falter, and time
disorientation occurs to the degree that the person may not be able to tell if
it is day or night – the person wakes at midnight and asks for lunch. Appointments are forgotten and personal
possessions are lost or sometimes hoarded and hidden.
Because there are severe deficits in the
ability to think and remember, business affairs must be turned over to a
conservator or family member with power of attorney. At this point, families may still be able to care for the
person, if there is support from its members. If a support network is not in place, most families find the
caregiving overwhelming, and a higher level of care is required. This type of behavior is often the
reason for a referral to a long-term care facility.
Later Stage
As the disease progresses, screaming,
wandering aimlessly, and combative behaviors often appear. The person in the later stage of Alzheimer's disease is no
longer able to find his way from one point to another. He often is disoriented as to time and
place. His ability to recognize
people becomes impaired, and he may mistake a caregiver for a family
member. Fine motor skills, such as
the ability to write or manipulate objects, are lost. The person now needs help with eating, getting dressed, and
toileting.
Speech becomes garbled and incoherent and
nonverbal communication must often be used. A compulsive need to touch everything, to hoard everything,
and to examine all objects with the mouth begins to emerge.
There is sometimes a complete loss of
emotion. Dietary habits change,
ranging from anorexia to binge eating.
The person may exhibit inappropriate sexual behavior. Even with all of these problems, a
person in this phase may still be able to engage in, and enjoy physical
activities such as walking and group activities, and will still enjoy music.
By this time, behavior patterns literally
fall to pieces. Motor sequencing
programs are shattered into fragments.
The person may suddenly get up, stop, look around, touch the wall, and
sit down again without having the slightest idea what she is doing.
In this stage, the person requires 24-hour
care. Placement in a care facility
may become necessary. When this is
done, the lack of familiar surroundings and faces often results in a total loss
of orientation. Personal hygiene
is done entirely by a caregiver.
Sleep becomes severely impaired, and agitation and confusion often occur
upon awakening and before bedtime.
Terminal Stage
In the end stage of this cruel siege, the
individual may lose the ability to walk or stand up, and the ability to
communicate in any meaningful way.
The terminal stage requires total nursing care. The patient is dependent on support for
all physiologic processes. He is
non-responsive and cannot recognize family members or familiar objects. Further deterioration is usually halted
by death from an infection, renal failure, or pneumonia.
Losing a loved one to this disease is a
painful and devastating process.
Family members undergo prolonged anticipatory grief and require frequent
support from the staff and from each other. Some family members may not be able to tolerate seeing the
mindless, ravaged body of a person who no longer recognizes them. Occasionally, to protect themselves
from the pain, they stop visiting the patient. Supporting the family members is vitally important in
preventing abandonment at this time.
Depression and anxiety are the most
prevalent, and also the most misdiagnosed, emotional disorders in the older
population. Together, these
debilitating disorders will impair the quality of life and shorten the lifespan
of millions of adults. In fact,
the World Health Organization ranks depression as the number two cause of
mortality in older people and predicts that by 2020, depression will rank
second only to ischemic heart disease in terms of disability. There is an association between anxiety and suicidal thoughts in older adults.
Extent of the Problem
In healthy adults, depression beginning late
in life is uncommon – less than two percent of the healthy elderly suffer from
late onset depression. Despite the
occasional inconveniences that accompany aging, most older adults actually
experience an increase in life satisfaction.
On the other hand, depression is rampant in
older people who are medically ill.
The greater the severity of the illness, the more likely it is that a
person will become depressed.
For this reason, depression in the elderly
is seen largely among disabled, hospitalized, and long-term care patients.
Depressive symptoms are found in 40 to 50
percent of nursing home and geropsychiatric hospital residents, and in a recent
study of several nursing homes, major depression was found in 25 percent of the
cognitively intact residents and 10 percent of cognitively impaired residents.
The Diagnostic and Statistical Manual of
Mental Disorders (DSM-5) emphasizes emotional symptoms such as sadness and anhedonia
as the quintessential criteria for the diagnosis of depression. However, in the elderly, physical
symptoms may be more prevalent.
In fact, in one study of 1146 patients with
major depression, physical symptoms were the chief or exclusive complaint for
69 percent of those identified.
These symptoms include headache, back pain or nonspecific
musculoskeletal complaints, weight loss, constipation, a bad taste in the
mouth, lack of interest in sex, and insomnia. In addition, physical symptoms that are not usually
associated with depression, including gastrointestinal complaints, are also
common. One study of irritable
bowel syndrome showed markedly higher rates in depressed patients versus
controls.
When emotional symptoms are reported, they
are most likely to be complaints of agitation, anxiety, panic attacks,
irritability, and obsessive concern with bodily functions.
Despite the high prevalence of depression in
the medically ill elderly, sufferers seldom admit to being depressed, and
rarely seek treatment.
Depression’s Impact on Health
Heart disease and stroke are the leading
causes of death and disability among older Americans today. Depression is associated with increased
mortality in patients with ischemic heart disease activation. Although cardiovascular disease is
linked to many factors – such as sedentary lifestyles, hostility, cynicism,
smoking, and alcohol abuse – the presence of depression is the most potent
predictor of mortality.
Studies show that even when the effects of
smoking are controlled, depression remains a significant independent predictor
of mortality among heart patients and stroke survivors. The relationship between depression and
heart disease is reciprocal, with each condition exacerbating the other.
In 1905, German psychiatrist Robert Gaupp
coined the phrase arteriosclerotic depression after observing that many
elderly depressed people also showed hardening of the arteries. Felix Post also suggested that vascular
disease in the brain was a significant factor in the development of depression
in late life.
With the advent of computer tomography (CT
scans) and magnetic resonance imaging (MRIs), it has actually become possible
to evaluate vascular changes in the brain of elderly patients with
depression. These changes are seen
as hyper-intense signals in both the white matter and the gray matter.
In 1988, Dr. Ranga Krishnan found that over
70 percent of patients with late-onset depression (defined as depression with
its onset over age 50), had hyper-intense signals on MRI images that are
indicative of small strokes. The
main locations of the gray matter changes were in the basal ganglia, in the
caudate and putamen, the cingulate gyrus, and in the frontal lobes of the brain
– areas that mediate mood and executive function.
It has long been known that many people with
depression exhibit low levels of serotonin. Recently, it’s been suggested that the link between vascular
disease and depression may be because blood platelets and brain neurons share
the same serotonin transporter protein, and are moderated by the same gene.
Other research suggests that this link has a
genetic component – that is, depression often runs in families. Even in people without heart disease, platelet
activation (the process in which platelets stick to one another and to tissue, forming a plug or clot) is
increased in late-life depression, and is most often found in elderly depressed
subjects with a 5HTTLPR l/l genotype.
Several studies have linked this genotype with mood disorders,
suggesting that there may be a common pathway to blood flow problems in both
the brain and the heart through which depression increases mortality in the
elderly.
Other risk factors for vascular depression
include diabetes, hypertension, and atherosclerosis. Those that had cardiac surgery are also at much higher risk.
There is also a growing body of evidence
that recovery from heart attack and stroke is influenced by depression. Researchers point out that the heart is
not only a pump that delivers blood to all vital organs, but it is also a sense
organ that responds to emotional upset.
Disability and loss of stamina following a
heart attack is often accompanied by a major depression. The emotional impact of this type of
traumatic event brings the person face-to-face with his own mortality, and
often suggests to him that he is much more vulnerable than he once
believed. This revelation is often
accompanied by bouts of hopelessness, anxiety, and depression. This type of reaction can be dangerous
in that it can impede physical rehabilitation compliance with treatment.
Depression in the elderly can be expensive
and lethal. Medical costs are 47
to 51 percent higher in depressed elders compared with non-depressed cohorts,
and depressed elders have a 50 percent higher risk of heart attack than those
free of depression.
Behavior, Memory and Cognition
Depression is also one of the most common
under-diagnosed causes of memory problems. Depression has a profound effect on the ability to think,
reason, and remember. In fact, the
symptoms of depression can be so severe that it is often difficult to tell
whether a person is suffering from depression or dementia. Because of this, several diagnostic
tests have been developed to ferret out the differences between these two
memory-destroying disorders.
It is vitally important that all elderly
people be screened for depression because depression in cognitively intact
individuals can mimic the signs of dementia, while depression in people with
cognitive problems can make their problems worse.
Depressed people
become focused on internal events.
These may be memories about tragic losses, or about real and imagined
transgressions. As just mentioned,
the focus is often on physical symptoms such as body aches and pains. This internal preoccupation prevents
the person from attending to the outside world.
Depression actually slows down the level of
brain activity in the afflicted person, so that memory and thought-processing
are impaired. People suffering
from depression often are said to exhibit poverty of thought, which is
the inability to process thought at all.
Medical Causes of Depression
Depression is often one of the first signs
of thyroid disease. Even subtle
decreases in thyroid hormone can induce depression, and in the elderly,
depression may be the only sign of thyroid dysfunction. For this reason, depressed residents
should be routinely screened for thyroid problems, particularly if they
complain of depression and fatigue.
Like the thyroid gland, dysfunction of the
adrenal gland has been associated with depression, so adrenal function should
also be checked.
Temporal lobe tumors are particularly
inclined to cause depression, and are frequently masked by the psychological
symptoms of headache and paresthesias.
Depression can also be caused by allergies
to environmental toxins. For
example, solvents like those used in paints, furniture-making, carpet-
manufacturing, and boat-building have been reported to cause depression,
confusion, and memory loss in many people.
Although rare, another potential cause is
chronic exposure to heavy metals.
Because elderly people may have an impaired ability to eliminate toxins
from the body, these factors should be ruled out before further intervention.
Chemical Causes of Depression
Although depression is often triggered by a
loss or trauma, or a biochemical imbalance in the brain, it can also be caused
by nutritional deficiencies or excesses; prescription, over-the-counter, and
illegal drugs; alcohol, caffeine, and nicotine; hypoglycemia; and hormonal imbalances. In fact, research suggests that almost
any chronic biochemical imbalance can cause depression.
Many medications, used alone or in
combinations, may cause depressions.
Often, reducing the dosages, elimination of use, or changing certain
combinations will correct the problem.
Here are a few of the most common culprits:
Anti-emetics
Anti-emetic drugs are used to prevent
nausea. But if they are used in
large doses or over a period of time, they may cause depression. If this is the cause, discontinuing the
drug or using a smaller dose usually reverses the symptoms in two weeks.
Sedatives
Unfortunately, sedative drugs are often used
by elderly people to promote sleep and reduce anxiety. Instead, they often lead to addiction,
abuse, and an increased risk of depression and suicide. Because of this problem, some states
now use computer tracking to see if the person is obtaining these medications
from more than one doctor.
Corticosteroids
Steroid drugs, used as anti-inflammatories,
often cause depression, which usually occurs late rather than early in their
use.
Antihypertensives
Blood pressure medications can also cause
depression and subsequent behavioral problems. Even though this is common knowledge, many doctors are
unaware of how often people suffer from drug-induced depression, and fail to
connect depressive symptoms with the medication.
Harvard researcher Dr. Jerry Avorn and his
colleagues looked at how often antidepressants were prescribed to people taking
beta-blockers such as Inderal, Lopressor, and Corgard. Examining the medical records of
143,253 residents, they found that 23 percent (almost one out of four) of those
taking beta-blockers were also taking antidepressants.
This study revealed that doctors often give
patients additional prescriptions to overcome side effects of another
medication without realizing that the problems could actually be solved by
eliminating the first medication.
Bicarbonate
Ingestion of large amounts of bicarbonate
may lead to depressive symptoms.
In addition, the vomiting of gastric acid and respiratory acidosis cause
a rise in the plasma bicarbonate level.
Many patients who have anxiety or hysteric vomiting attacks take
over–the-counter bicarbonate as a relief, which eventually upsets blood
chemistry and pushes them into depression.
Antacids
Systemic antacids such as Tagamet and Zantac
have high side effect profiles in older people. They have been known to cause depression, anxiety, and even
psychosis in some individuals.
Post-Stroke Depression
Although they are usually easy to diagnose,
strokes – with or without physical impairment or disability – often cause
depression. Strokes may be major
or minor, and minor ones may produce as severe a depression as a major stroke.
The most effective treatment for post-stroke
depression is antidepressant drug therapy.
Other contributing factors to depression can
be physical problems such as hearing loss, vision problems, foot problems, and
even dental problems.
I was once called for a consultation for a
patient who had been isolating, refusing to leave her room, and refusing to
participate in groups or mealtime.
Although this woman had a history of depression, during the interview
she told me, “I’m not leaving this room until I get my new dentures. I look so ugly without my teeth.” In this case, a dental
consultation cured the problem.
Psychotic Depression
The term psychotic depression was
quite common prior to the 1940's.
In fact, during that time, as many as two-thirds of hospitalized
depressed patients were diagnosed as psychotically depressed. Today, the term has fallen out of
favor, and less than ten percent of depressed patients are considered
psychotic.
Nevertheless, psychotic depression happens
frequently in the elderly. This
type of depression often mimics dementia, and can include hallucinations,
delusions, and other bizarre symptoms.
It’s important to remember that depression alone can cause psychotic
symptoms. When a person becomes
delusional or begins to hallucinate, depression could be the cause.
About two-thirds of psychotically depressed
people have delusions but no hallucinations, and about one-quarter hallucinate
without delusions. Although
delusions and hallucinations take many forms, patients often claim that their
insides are rotting, and that the devil is speaking to them.
The most common delusion seen in
psychotically depressed people is the delusion of persecution – the
belief that other people are wishing the person harm. Often, the person feels that they deserve to be
punished. Some say that they are
evil and that God is punishing them.
Elderly patients who express intense feelings of guilt and remorse
should always be screened for psychotic symptoms.
The sudden onset of an anxiety disorder is
unusual in elderly people, but many have had a long-standing history of anxiety
disorders. When anxiety does
appear late in life, it’s usually associated with a stressor, is a sign of
medical illness, or may be a medication problem. These factors should always be assessed and ruled out before
a diagnosis is made.
Medical Causes of Anxiety
- Endocrine disorders
- Hypo- and hyperthyroidism
- Pheochromocytoma (an adrenalin secreting tumor)
- Hypoglycemia
- Hypercortisolism
- Stimulants
- Caffeine
- Cocaine
- Amphetamines
- Nicotine
- Withdrawal from sedatives, alcohol, or tranquilizers
- Brain tumors
- Strokes
- Epilepsy
- Pulmonary embolus
- Chronic pulmonary disease
- Aspirin intolerance
- Collagen vascular disease
- Brucellosis (undulant fever, rock fever, and Malta fever)
- B12 deficiency
- Demyelinating disease
- Heavy metal intoxication
- Food allergies
- Balance disorder
|
|
The root of anxiety is a malfunction of our
innate fear response system. Fear
is a normal human emotion. Although no one enjoys the feeling of fear, it has
an important function – to help us avoid danger. For example, it’s normal to be afraid of something we have
never encountered before. Fear
prompts us to proceed with caution when we enter unexplored territory, and only
when we feel that we can handle a situation does the fear disappear.
Fear has another important function – it
promotes social bonding. All
children are naturally afraid to be alone. Because children cannot survive without their parents, fear
saves their life. A child who had
no fear would wander off, and probably die.
Children instinctively run to their parents
whenever they get scared, and the parent's natural tendency is to calm the
child and allay the fear. Over
time, this sequence of events teaches us how to cope. As we hear our mother’s voice say, “It’s all right, nothing
will hurt you now,” over and over, we eventually make these words a part of
ourselves. This process of being
held and internalizing calming messages is called self-soothing.
So, if we spend most of our early years
physically and emotionally attached to our mothers, as we grow and mature and
learn to self-soothe, we are able to tolerate more and more time alone. We also come to realize that many of
the things we fear will never happen – there are no monsters in the closet.
In the elderly, anxiety disorders can occur
because of the failure of one or both of these factors – people with anxiety
disorders are afraid to be alone and/or they have difficulty self-soothing.
There is evidence that this process of
bonding with parents stabilizes the brain circuitry that mediates fear. In animal studies, it has been shown
that animals that are handled and held regularly have a stable HPA axis (the
circuit of the hypothalamus, pituitary and adrenal glands are part of out
fight, flight, or freeze system).
Animals handled in infancy have increased
hippocampal activity throughout their lifespan, and do not show HPA
abnormalities in later life.
Furthermore, their levels of cortisol are permanently lower, and this decreases
the risk of dementia. In studies
of older humans, HPA axis abnormalities are related to anxiety. These subjects have been found to
consume higher levels of dietary fat and sugar – both risk factors for cognitive problems. They also have higher levels of plasma
cortisol and a smaller number of cells in the hippocampus, the part of the
brain that stores memory. These
findings suggest a link between cortisol, anxiety, and increased risk for
dementia
Although social bonding is a primary element
in reducing fear, many elders have lost most of their social contacts – through
death, illness, or relocation.
Loss of social support provokes fear, and pain from the losses they have
suffered makes them reluctant to form new friendships, which leads to isolation
and increased anxiety.
Our alarm circuits prepare us for threats by
increasing heart rate, blood pressure, and muscle tension. When this system becomes activated, we
scan the environment for danger.
Once the danger is identified, we make decisions on how to deal with it,
and our alarm system returns to baseline.
But when the system itself goes awry, a
person may experience a diffuse, global feeling of threat, and will assess the
environment for danger, seeing nothing external that can be identified as a
threat. Because the system is
malfunctioning, the level of arousal does not return to baseline and the person
begins to seek sources for their disease.
An anxious person becomes fixated on
threats. Increased threat
assessment means that the person’s working memory is occupied with danger,
leaving no room for solutions.
Lack of ability to generate solutions leaves a person frozen in
indecision.
For these reasons, many anxious people focus
only on reducing their feelings of anxiety, and not on recognizing and reducing
the causes. Common methods of
reducing anxiety are isolating and substance abuse, which cause more problems
than they cure. Treatment must
therefore focus on reducing threats, increasing coping skills, and helping with
problem-solving.
Anxious people may also have another deficit
– they cannot separate realistic fears from irrational fears. This means spending time perseverating
over things that might happen, and whipping themselves into a frenzy. This type of behavior is more prevalent
in older people who have low life-satisfaction, high levels of neuroticism, and
who have not accomplished what they wished to in life.
Because older people suffer from many
medical problems, including aches, pains, and gastrointestinal disturbances,
they may conclude that these symptoms are the threat, and become preoccupied
with them. This condition is
called hypochondria, and this is one
reason why older people are high medical users. Unfortunately, being labeled a hypochondriac means not being
screened for anxiety, and effective intervention will not occur.
Three Basic Components of Anxiety
Emotional
- Restlessness, agitation, irritability, hypervigilance
Cognitive
- Worry, rumination, cognitive impairment
Somatic
- Muscle tension, aches and pains, sleep problems
|
|
This can manifest itself by the person
becoming overly-dependent on others and engaging in incessant attention
seeking. They may also become
overly-demanding and complaining.
This type of behavior is often charted in care facilities as
attention-seeking, and the diagnosis of anxiety is frequently missed.
Older women are twice as likely to have an
anxiety disorder as older men are, and older adults are more likely to
experience depressive symptoms along with anxiety.
Generalized anxiety disorder is the most
common problem found in the elderly (followed by anxiety due to a general
medical condition), affecting up to one- third of older adults. Often triggered by worry and increased
threat assessment, this type of anxiety is also, in part, reality-based – older people have more to fear.
As well as being more prone to illness or
injury, older people are also frequent victims of crime. Lack of mobility, decreased stamina,
and waning strength contribute to feelings of vulnerability. An older person walking alone is a
target for predators, and many people, rather than exploring ways to stay safe,
become fearful of leaving their home.
Although phobias are less common in this age group, agoraphobia is quite
prevalent.
Stressors such as retirement, disability,
money problems, alienation, widowhood, and loneliness may also increase
anxiety. Any chronic illness
(especially Parkinson’s, chronic obstructive pulmonary disease, and chronic
pain) can contribute to feelings of anxiety.
Unfortunately, because many of these
symptoms are common in older people, they are written off as components of
normal aging rather than symptoms of anxiety. For these reasons, anxiety may be present in many elders,
but interpreted as part of another problem, rather than the existence of a
disorder. Some of these symptoms
could also be interpreted as signs of dementia. Anxiety also presents as a component of depression in the
elderly – 75 percent of general anxiety patients also fit the criteria for
depression.
Panic disorders are rare in the older
population. When panic disorders
do appear, they are usually tied to a stressor such as a loss or an
illness. Unfortunately, many
elders who have experienced a panic attack are given tranquilizing drugs, which
are not effective, are addictive, and greatly increase the risk of falls.
Stages of Grief
- Denial
- Emotionality
- Bargaining
- Depression
- Acceptance
|
|
In an elderly person, it is important to distinguish depression from grief and sadness. Sadness is a transitory state, and very often is the result
of revisiting a painful memory. Temporary bouts of sadness are common in older
people, as most of them have had multiple wounds, regrets, and losses – and
from time-to-time – they revisit them. In these times, refocusing, reframing,
or assistance in working though these events can ameliorate bouts of dejection.
But while sadness may be a fleeting feeling, grief is a process that may last
for months or years.
Grief is the process of mourning a
significant loss. Most elderly
people, especially those in long-term care facilities, have undergone multiple
significant losses, such as the loss of spouse, loss of their home, loss of
friends, and most importantly, the loss of their independence. These losses are monumental and should
be grieved, but seldom are.
Instead, losses are minimized – that is,
caregivers rather than addressing the problem, tell the person to “Cheer
up.” While this is often
said in an effort to comfort the person, it actually discounts and trivializes
the loss. It is also not useful to
tell a grieving person, “I understand how you must feel.” Unless you have actually suffered
a similar loss, you don’t know how they feel.
You can never measure the extent of another
person’s attachment or loss, and no loss is trivial. For example:
Mrs.
Peterson was brought to the hospital because she was losing weight, was
isolating, and was suffering frequent bouts of crying. She had told others that she wanted to
die. It was discovered at the
intake interview that she had recently lost her parakeet – her closest
companion for the last ten years.
No one had recognized the enormity of her loss. In fact, the board-and-care
administrator had stated, “I wish she would quit crying about that stupid
bird.” When this loss was
validated and acknowledged, she was allowed to work it through, and eventually
recovered.
We all recognize that loss has a significant
impact on mood, but what is less attended to is the fact that loss also
disrupts fundamental patterns of living.
For example, Mrs. Johnson, who has recently lost her husband, has spent
forty years with him. During this
time she has developed, and stored, thousands of patterns of behavior. These programs allowed her and Mr.
Johnson to accomplish the tasks of daily living. The patterns ranged from mundane routines such as going
grocery shopping and cleaning the house, to more profound patterns such as
solving problems together, coping with the challenges of life, and interchanges
of intimacy.
The loss of Mr. Johnson is catastrophic, and
requires grieving, but it also means the loss of dozens of patterns of
behavior. Loss of patterns means
immobilization and isolation – two events that can completely disable Mrs.
Johnson. So, while grief work is
the fundamental task of recovery from loss, learning new patterns is essential
for reentry into the world.
Recently a pilot program that addresses this
problem was conducted at the University of Washington School Of Medicine in
Seattle by Dr. Paul Ciechanowski and associates. Called PEARLS (Program to Encourage
Active, Rewarding Lives for Seniors), this was a community outreach
intervention that helped seniors integrate patterns.
Ciechanowski evaluated the effectiveness of
this home-based program in a group of 138 mostly homebound seniors (average age
73) who had been diagnosed with minor depression or dysthymia. Seventy-two percent of the study’s
participants were referred by social agencies, and 28 percent were
self-referred. Seventy-two percent
lived alone, 42 percent belonged to an ethnic minority group, and 36 percent
received antidepressant medications at baseline.
Over a period of 19 weeks, participants in
the program received an average of 6.6 visits from social workers. The substance of the visits was a
combination of problem-solving therapy, and a focus on the patients regularly
becoming physically active and increasing behavior patterns outside of the
home. PEARLS recipients who
completed this program showed a 50 percent improvement in depression scores or
complete remission by the end of 12 months. They also had fewer hospitalizations than the control
group. The improvements in the
participants not only restored their quality of life, but significantly decreased
caregiver burden. Beside the
program’s high degree of success in regard to establishing connections to the world, the most important
element of this program was its cost – $630 per patient.
Grief and Trauma
Another anxiety disorder that is
under-diagnosed in this population is Post-Traumatic Stress Disorder. Older people often face catastrophic
losses, hospitalizations, surgeries, heart attacks, and strokes, all of which
can result in traumatization.
Grief is the negative emotional process
experienced when at least one of a person’s most important relationships is
ended unwillingly, through death, divorce, natural disasters, or
relocation. Unfortunately, most
elderly people have experienced multiple losses. Normally, grief is a time-limited reaction, but sometimes
grief reactions become chronic and interfere with long-term functioning. This type of problem is called pathological
grief.
Grief can have an immediate or delayed
onset. Delayed onset occurs when
the person gets stuck in the stage of denial. Delayed grief reactions, therefore, are somewhat similar to
the symptoms of Post-Traumatic Stress Disorder, and should be considered an
anxiety disorder. Pathological
grief differs from normal grief in the development of anxious
apprehension, phobias, panic, and depression.
Most societies have mourning rituals and
ceremonies that surround the death or loss of a close member of the
family. These rituals create a
context in which all the bereaved relatives and friends can experience their
painful emotions and work through their loss. However, these rituals and ceremonies no longer exist in
much of American culture, and because of this, it's difficult or impossible for
most people to do proper grief work.
Because of the loss of formal ritual, many
people in our culture are actually unaware that they must mourn or grieve. Instead, they try to escape from their
pain and carry on as usual. When
this occurs, the buried feelings may erupt later, disguised in some other form
– often in the form of panic attacks and anxiety symptoms.
The human grief response has its origins
early in mankind's social evolution.
For example, crying is an important survival mechanism. A small child separated from the tribe
could be found by listening to his cries.
The children that cried the most were the ones that were found the
easiest. After thousands of years
of development and evolution, crying when faced with loss has become a
fundamental human instinct.
To help work through loss, traditional
mourning rituals in other cultures encourage loud and sustained crying and the
expression of painful emotions. After
a few days of this, emotional exhaustion is experienced; it then becomes
possible for the bereaved person to complete the emotional and cognitive
aspects of the grieving process
Failure to mourn often results in
suppression of the anger, the fear, and the related emotions in the grief
process. Because these emotions
never get expressed, the levels of arousal in the person remain persistently
high. After the loss, the bereaved
person may carry on with his usual daily activities. However, even though a grieving person may have successfully
suppressed his grief, his body is still experiencing the grief reaction.
Symptoms may not appear until many years
after the loss. When they do
appear, it is frequently on or around the anniversary of the loss. The most common symptoms are panic
attacks and phobias.
On occasion, the loss of one's health can
becomes a substitute for the loss of the person. Instead of grieving, the person becomes preoccupied with
phobias, panic attacks, or illness.
The search for the cure for the illness unconsciously represents a
search for the lost relative.
Feelings of anger and rage are then displaced onto the doctors and
caregivers who fail to find a cure.
Even if it is suggested that the anxiety
disorder is a result of unresolved grief, the patient is very reluctant to
engage in grief work. To make
things even more difficult, the spouse or family members may ridicule the idea
of grief work, claiming it is irrelevant to the problem. If the patient does begin grief work,
family will often interfere with the process and ridicule her for weeping and
crying. If this occurs, the
treatment must be explained thoroughly to family members, and the family must
be involved in the treatment process.
Suicide is currently the seventh leading
cause of death in the United States.
It accounts for over 30,000 deaths each year. Moreover, the suicide rate rises consistently as age
increases – taking one’s own life is presently the ninth leading cause of death
in the elderly. Although older
Americans comprise 13 percent of the population, they account for 18 percent of
all suicides. White males over 65
have the highest suicide rate – twice the rate of the general population, and
six times the rate in women over 65.
Elderly people actually have a lower
incidence of suicide attempts than younger people do, but they are much more
intent on killing themselves, and therefore they have a much higher success
rate. Nonfatal suicidal gestures
are uncommon among the elderly.
Unlike attempts by teens and borderlines, suicide attempts in the
elderly are rarely done for social manipulation – they are the direct intent to
die. Lethal methods tend to be
used, and failure to kill one’s self is most often due to poor planning, rather
than any lack of intent.
The American Association for Marriage and Family Therapists (AAMFT) say older adults make up 12% of the US population, but account for 18% of all suicide deaths. Someone age 65 or over completes suicide
every 90 minutes – that’s 16 deaths a day. Nevertheless, suicide is uncommon in healthy elders. Most people find an increase in life
satisfaction as they age.
However, suicide is high in the elderly
medically ill population. Disease
burden is a predictor of anxiety, depression, and suicide in this population.
Announcing Suicide
One of the myths of suicide is that those
who decide to kill themselves do not seek help before their attempt. Actually, over 60 percent of those who
do commit suicide tell others beforehand.
The typical suicidal person will tell at least three people about his
intent before he attempts it.
Unfortunately, elderly suicidal people
seldom seek help from mental health practitioners. The sufferer will most likely seek medical rather than
psychological help. Studies on
elder suicide show that more than 65 percent of all victims seek medical
attention within three months before their suicides. Seventy-five percent have contacted their primary care
physician within one month before their death, and over one-third have seen a
doctor a week before their demise.
In fact, suicidal people almost always
communicate their intent to kill themselves, and do it several times and in
different ways. Communication may
consist of overt statements of suicide, statements of not wanting to live, or
statements that life is no longer worth living. Less direct methods of communication include making a will
under unusual circumstances, changing insurance policies, giving away valued
objects, or making statements of “putting my affairs in order.”
Having suicidal thoughts is not a normal
phase of life. A suicidal person
has a distorted view of reality, convinced that there are no solutions and that
things will never change. Because
of this, suicide has often been called a permanent solution to a temporary
problem. It is, in fact, a
maladaptive means to escape from anguish.
Risk Factors
Major depression is the most common reason
for suicide – the suicide rate among the depressed being four times higher than
the national average. When the
person is suffering from psychotic depression, the rate is five times higher.
Although there are not many older schizophrenics, any psychotic disorder increases risk for suicide . A person with psychosis who has paranoid thoughtsand is subject to panic states is at very high risk for self-harm. This risk is increased even more if the person hears voices commanding him to kill himself.
Suicide is more common in the divorced and
widowed. Elderly men who lose
their wives are at highest risk.
Oftentimes, the wife was responsible for social activities of the
couple, and her death or departure means an abrupt end of social interaction.
The more closely a person is involved with others,
the lower the probability of suicide.
Therefore, it is important to look at the person’s social support
network when doing a suicide assessment.
If the person has no friends or family, they are at high risk.
There is also a direct relationship between
social status and suicide. In
general, the higher one is on the socioeconomic ladder, the more likely she is
to attempt suicide. For example,
physicians and dentists have a much higher incidence of suicide than the
general population.
Weakening of higher brain functions by
sleeplessness, alcohol, or drugs also strongly contributes to the potential for
self-destruction. In fact, half of
all suicides are associated with alcohol abuse, and the suicide rate among
elderly alcoholics is ten times that of those who do not drink. About 70 percent of successful suicides
in the elderly are committed by persons with a previous diagnosis of
alcoholism, psychosis, or organic brain syndrome.
The incidence of suicide also rises after
surgery, particularly in surgeries that mutilate or change a person’s
appearance; the impact on the person’s body image is often intolerable. This loss must be grieved completely in
order for the person to move ahead.
Suicide by a close family member increases
one's suicide potential significantly.
Guilt, especially over the dead relative, feelings of worthlessness, the
wish for punishment, social withdrawal, and feelings of hopelessness, anxiety,
and agitation are all contributing factors.
However, the most important predictor of suicide
is a previous attempt. Over half
of those who commit suicide have had at least one previous attempt.
Silent suicide is the intent to kill one’s self by nonviolent
means, often through self-starvation and resistance to care. These attempts to end one’s life often
go unrecognized because the depression is not diagnosed, and resistance to care
is seen as a bothersome behavioral problem rather than a suicide attempt. Because of this, resistance to care and
noncompliance with treatment should always be considered as a sign of
depression and suicidal intent.
Since more than half of all suicides occur
in people suffering from mood disorders, one might expect that the
implementation of the more effective SSRIs would decrease the suicide
rate. Yet this has not
happened. Psychological autopsy
studies show that among depressed adults who have killed themselves, less than
one-third of them were taking antidepressants at the time of their death. It is clear that in most cases, the
diagnosis has been missed.
A study funded by the National Institute of
Mental Health (NIMH) and conducted by Dr. Martha Bruce and colleagues at
Cornell University, addressed the problem of missing diagnoses of depression
and suicide in older patients. The
pilot program took place in three major Eastern US cities, and was published
in the March 3, 2004 Journal of the American Medical Association.
Reynolds and colleagues set out to
demonstrate that by educating physicians and improving treatment up to
guideline standards, a social worker, nurse or masters-level psychologist can
significantly improve clinical outcomes.
Called PROSPECT (Prevention of Suicide in
Primary care Elderly: Collaborative Trial), the program placed depression
care managers in ten primary care practices located in Philadelphia,
Pittsburgh and New York City. Each
practice was paired with a similar practice without a depression care manger,
which served as a control.
The care managers screened all patients
visiting the clinics for depression and suicidality. Over two years, about 12 percent of the primary care
patients tested positive for depression and suicidal ideation. From these, 598 (mostly females,
two-thirds with major depression) were recruited into the study.
The care managers offered patients treatment
for their depression including psychotherapy from the care manager and/or a
serotonin selective reuptake inhibitor (SSRI) or another antidepressant, if
clinically warranted. All
treatment was supervised weekly by a psychiatrist. Care managers actively followed the patients, monitoring
their symptoms, drug side effects, and treatment adherence.
The intervention did not lessen symptoms in
patients with minor depression but it did significantly decrease suicidal
thoughts. After eight months, 70
percent of patients with suicidal thoughts were symptom-free compared to
controls. The results of this
study show the importance of assessment of depression and suicidality in a
primary care setting, and that treatment can significantly reduce the risk for
suicide in late life.
Barriers to Diagnosis
Risk Factors for Suicide
- Male over 50
- Single
- Family history
- Previous attempt
- Depression, anxiety, and/or schizophrenia
- Availability of weapons
|
|
As mentioned previously, the majority of
older people who manifest symptoms of depression, anxiety, or suicide are high
medical users, and visit their primary care physician frequently. While there, they may speak of multiple
physical complaints. In these
cases, the diagnosis of depression is often missed.
But even when they display clear signs of
depression, there is a marked tendency for physicians to underestimate the
severity of depressive symptoms, especially in patients who are more
depressed. Studies show that
doctors are most influenced by overt symptoms such as crying and depressed
mood, which are valid – but not reliable – indicators of depression in this
population. Anhedonia, guilt,
suicidal thinking, and hopelessness are more potent indicators, but are seldom
assessed and rarely spontaneously discussed by the patients. Missing these diagnoses not only
precludes the opportunity for treatment, but also puts the patient in
peril. Depression is associated
with treatment refusal and poor treatment compliance even when there is a good
medical prognosis. Those with
anxiety often self-medicate with alcohol and sedatives, which increase the risk
of further medical problems, including falls.
Barriers to
Treatment
In 1999, Dr. Wayne J. Katon at the
University of Washington in Seattle published an important paper addressing the
barriers to effective treatment of mood disorders.
His research revealed that few patients
diagnosed with depression and started on antidepressants received adequate
dosage and duration of antidepressant therapy. In addition, about 40 percent of patients who started on
antidepressants dropped out of treatment within one month.
Examining the results of this research,
Katon concluded that acceptable outcomes in the treatment of depression were
not occurring with traditional medical treatment (which usually consisted of
brief, infrequent visits with a primary care physician). This led Katon to the idea of
collaborative care. This type of
care is done though a health care team, including mental health professionals
and care managers who provide education, patient follow-up, and careful monitoring of outcomes. This type of model is particularly
suited to the older population, who may have problems with travel, treatment
compliance, and an aversion to mental health treatment.
Katon has also pointed out that treatment
failure in this population is highest in elderly women, with only 37 percent of
women showing significant improvement with treatment. Treatment failure was related to patients who had a low level
of social support and low socioeconomic status, and showed high levels of
neuroticism.
Treatment of Depression and Anxiety in
the Elderly
Ask all people being assessed about suicidal
thoughts. Ask if the person has a
plan. A plan and the means to
carry it out are indicators of extremely high risk.
Get a thorough family history about
depression and suicide from the person, family members, and friends, as this
suggests a genetic predisposition.
Studies show that suicide can have a genetic component, and low levels
of serotonin are found in suicidal families. In these cases, SSRIs (such as Prozac) can be of great help.
Suicide is seen as the only solution to what
appears to be an unsolvable problem.
Effective intervention consists of helping the person identify the
problem, and helping him explore constructive solutions.
Ask people with chronic pain about suicidal
thoughts.
Chronic, unremitting pain often leads to the
wish to die. However, when
pressed, most people with chronic pain will agree that what they really want is
to stop suffering. Once this is
established, all efforts should be focused on reducing the pain. A good pain management program can do
wonders in these cases.
Assess their social support network, and the
activities of a typical day. A day
spent with no friends and no joy is a day wasted. Help the person plan a day of enjoyment, and explore ways of
connecting them with others who share similar interests.
If the person undergoing treatment for these
disorders is cognitively intact, cognitive behavioral therapy is
appropriate. The best outcomes in
these cases result from a combination of therapy and antidepressant medication,
keeping in mind that older people may be at more risk of side effects and drug
interaction effects.
Re-integrate pleasant activities into the person’s daily regimen.
Grief is a normal response to loss. Sadness and depression are part of the grieving process, and should not be considered a mental disorder. Once the losses have been listed, explored, and discussed, some must be grieved. Through the loss assessment, you can explore losses that have not been grieved.
Most older people are not familiar with the process of grieving. One of the most effective ways to help them grieve is to explain the normal stages of grief. This normalizes the emotions they are feeling, and allows them to take the time to work through and resolve the grief.
Once a person has done this, have him engage in one of the activities. When he is finished, have him rate how much he actually enjoyed the activity. Depressed people under-rate their capacity for enjoyment. When they realize that they can actually enjoy the things they once did, they become more willing to do them again.
Tie current problems and stressors to the life review, and help him see that the skills and strengths he accumulated can be used to solve his current problems. Once you have found his favorite music, it can be an effective tool to refocus him and brighten his mood.
The following components of treatment are
useful in treating depression and suicidality.
Construct a Loss History
When a older adults appear to be depressed or
anxious, a loss history can be useful. This is a historical survey of the person’s recent and
remote losses. Losses can include
the death of loved ones, but also can be the loss of a job, a pet, loss of a body part, loss of senses, or
social standing. Inquire about
child abuse, trauma, spousal abuse, and elder abuse, all of which may
contribute to problems.
With a comprehensive loss and abuse history,
you will have an outline of the person’s pain and sorrow.
Begin a Life Review
Life review should focus on the person’s
triumphs, successes, and high points in her life. These strength and successes can then be linked to current
concerns, which will increase coping skills.
With a life review, you will have a history
of the person’s strengths.
Help the Person List Their Talents and
Skills
Help the person construct a list of her
positive qualities, talents, and skills.
If she cannot do this, gather information about triumphs.
With a list of positive qualities, you will
have a history of the person’s worth.
Construct a Favorites List
This is a list of all the activities she
used to enjoy. This can be done by
using a favorites questionnaire.
Ask about favorite activities, books, movies, foods, and music.
With this list, you will have a history of
the person’s joy.
Use Music for Recollection
Playing music, especially favorite songs,
can be a powerful trigger for recollection, which is a great help in gathering
data for the categories listed above.
Targeting songs from different times in a person’s lifespan will help
them with the loss history, life review, favorites, and strengths and
abilities. A familiar song can
transport her back to moments in her life she had not thought of for years.
With music, you will have a history of the
person’s heart.
Medications for Anxiety
and Depression
In most cases, there is a medical origin of
depression and anxiety. A thorough
medical workup can reveal suspected causes. Therefore, a referral to a competent physician is the first
step in treatment-planning. Keep
in mind that less than 10 percent of physicians in this country are educated in
geriatric medicine and aware of the medical problems listed above. For this reason, it is useful to
provide them with some research papers delineating the medical causes of mood
disorders. This will help them
target their observations and clinical tests.
Once medical causes have been ruled out, and
psychotherapeutic interventions have not been successful, depressed patients
may improve with antidepressants.
This success rate in older depressed people taking SSRIs is about 65
percent.
Medication for anxiety should be considered
only when all other interventions have failed. Tranquilizers are not recommended for long-term use
in the elderly because of their potential for abuse (they are addictive) and
because they exacerbate cognitive problems. They also have psychomotor effects that lead to falls, which
can be lethal. Despite these
dangers, anti -anxiety drugs are the most common treatment modality
for this population.
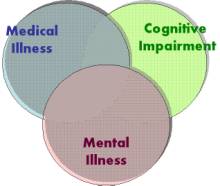 Older adults
present with a vast array of behavioral and psychological symptoms. An assessment of the older adult must
address the realms of mental symptoms, medical problems, and cognitive status
Older adults
present with a vast array of behavioral and psychological symptoms. An assessment of the older adult must
address the realms of mental symptoms, medical problems, and cognitive status
Because of the high likelihood that an older
person will be suffering from multiple physical maladies that could impact
mental status, a comprehensive assessment must include a thorough examination
of all medical symptoms and all medications. Find out when the last physical was done, and get the results. Be aware that physicals may not include gastric assessments and immune deficits – common problems in this population. (See the sections above for the most common medical problems
and their contribution to psychological problems.)
A medical history should be the first step
in any diagnosis. It should
include a history of all illnesses, injuries, and hospitalizations throughout
the person’s lifespan.
Unfortunately, this is often impossible, as medical records are lost and
family members are unavailable.
Often, the only data available is from the person himself, and he may
have forgotten many of his illnesses, injuries, and aliments.
To further complicate things, the signs and symptoms of many diseases are often
less severe, non-specific, or not present in many elders. People suffering from
these disorders may not be able to give you an accurate description of what
they are experiencing. The best you might get form a person is that she feels
tired or she is “not herself.”
In addition, cognitive impairment must be
assessed. The person’s capacity to
think and reason, make informed decisions, and remember what is being
recommended in terms of treatment will determine the method of treatment
rendered. For example, a person
with impaired cognition and memory will not benefit from cognitive therapy, and
a person with memory deficits will not be able to recall what has been
recommended.
If you are working in a long-term care
setting, an assessment can be daunting.
You will often have no access to medical records. There will be no family or friends that
can supply historical information and the person will not remember his medical
history. Occasionally, there will
be a discharge summary available describing the person’s most recent
hospitalization. This helps, but
often contains little history. A
history and physical may also appear in the chart, but often times
it will be illegible.
What you are left with is the person’s
description of his symptoms and concerns, and information from the staff about
observable emotional and behavioral problems. Often the person will claim to have no problems, so you are
left with your own observations and those of the staff.
Once you have gathered this information,
look on the face sheet in the person’s chart. This document will tell you the person’s age and birth
date. Check this with the person’s
recollection of their age and birthday.
Also on this paper will be a list of medical and psychiatric diagnoses.
A typical face sheet might contain something
like this:
Medical Diagnoses: |
Psychiatric Diagnoses: |
GERD |
Schizophrenia |
Diabetes |
Bipolar disorder |
Hypertension |
Delusional disorder |
Anemia |
Dementia |
There is a high probability that some of
these diagnoses are incorrect (especially the diagnoses of dementia – one out
of four is incorrect). They have
been made by different clinicians at various facilities over a long period of
time. Check with staff and other
clinicians to see if these diagnoses are still valid; if they are not, have
them updated.
Next, go to the physician’s orders sheet in
the chart to see what medications the person is currently taking, and if any
medications have recently been added or discontinued. See if behavioral or emotional symptoms coincide with
medication changes.
Check the side effects of all medications to
see if they could be contributing to the presenting problems. Alert those who are participating in
treatment planning that some of the presenting problems may be due to side
effects.
Also, check to see if the medications
coincide with the medical and psychiatric diagnoses. The desired outcome would be that each diagnosis corresponds
to a medication or treatment regimen. However, you may discover that there is no evidence that some
of the diagnoses are being treated.
If so, talk to everyone involved in care-planning about this discrepancy
and take corrective action. You
may also discover that the person is taking medication for which there is no
diagnosis. Take corrective action
here also. Ask the person if they
are also taking any vitamins, herbs, or over-the-counter remedies, as these may
also affect mood and behavior.
If you work in an outpatient setting, ask
your patient or client to bring with them a bag containing all of the
prescription medication, over-the-counter medication, vitamins, herbs, and
supplements he is taking. Make a
list of them and do some homework to see if any of these substances may have
unintended side effects. A
physician trained in geriatric medicine and consultant pharmacists can be invaluable in
this part of an assessment, but in the real world, most of you will be on your
own. [You can find a consultant pharmacist near you at https://www.ascp.com/find-senior-care-pharmacist.]
The next realm to explore is the impact of
medical illness on mental difficulty, which could be causing the problems. Do some homework here also to see if
the medical illnesses could be causing or contributing to the psychological
symptoms you observe.
After this, ask the person to tell you
everything she knows about her diagnoses.
This will give you a feeling for her awareness, judgment, insight, and
capacity to take an active part in her treatment.
The last area to assess is memory and
cognition. Assessment instruments
such as the Mini Mental Status Exam can give you a snapshot of potential
problems. Asking questions about
memory problems, historical data, and current events will give you an idea as
to orientation and awareness.
Formal tests of memory and executive function can also be used, keeping in
mind that, in general, older people do not like to be asked too many questions,
do not like to be tested, and get anxious, frustrated, and irritated when they
do not do well. Also, few of these tests have been normed for people over 80.
For this reason, informal assessment is usually the best choice. Once you have
ruled out medical illness, medication problems, and cognitive impairment as
a cause of the presenting problem, you can make a diagnosis just as you would
in a younger person.
References and
Additional Reading
Centers for Disease Control and Prevention (2017), Leading Causes of Death
https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm
Nursing Homes
Jean A. Talbot, PhD, MPH Andrew F. Coburn, PhD. (2013). Challenges and Opportunities for Improving Mental Health Services in Rural Long-Term Care. Working Paper #50 June Maine Rural Health Research Center.
Cohen CC., Herzig T, Carter EJ. (2014). State focus on health care-associated infection prevention in nursing homes. Am J Infect Control. Apr;42(4):360-5.
American Health Care Association
The Importance of a Course on Aging
Centenarians in the United States http://www.census.gov/
Brownie S, Nancarrow S. (2013). Effects of person-centered care on residents and staff in aged-care facilities: a systematic review. Interv Aging.;8:1-10.
Shura R.Siders RA, (2011). Dannefer D. Culture change in long-term care: participatory action research and the role of the resident. Gerontologist. Apr;51(2):212-25.
Bisla J, Calem M, Begum A, Stewart R. (2011). Have we forgotten about dementia in care homes? The importance of maintaining survey research in this sector.Age Ageing. Jan;40(1):5-6.
Spitzer WJ, Neuman K, Holden G. (2004). The coming of age for assisted living care: new options for senior housing and social work practice. Soc Work Health Care.;38(3):21-45.
Shura R, Siders RA, Dannefer D. (2011). Culture change in long-term care: participatory action research and the role of the resident. Gerontologist. Apr;51(2):212-25.
Seitz D, Purandare N, Conn D. (2010). Prevalence of psychiatric disorders among older adults in long-term care homes: a systematic review. IntPsychogeriatr. Nov;22(7):1025-39.
Kashi, E, Winokur, J (2003). Aging in America; The Years Ahead Powerhouse Books, New York, NY.
Galambos C, Rosen A. (1999). The aging are coming
and they are us. Health Soc Work. Feb;24(1):73-7.
Goulden, J (1976). The Best Years McClelland
& Stewart, NY.
The Impact of Aging on Mental Health
Knight M. (2011). Access to mental health care among older adults. J GerontolNurs. Mar;37(3):16-21.
Snowdon J. (2010). Mental health service delivery in long-term care homes.IntPsychogeriatr. Nov;22(7).
Hayflick L. (2004). The not-so-close relationship
between biological aging and age-associated pathologies in humans. J Gerontol A BiolSci Med Sci. Jun;59(6):B547-50.
Geokas MC, Lakatta EG, Makinodan T, Timiras
PS. (1990). The aging process. Ann Intern Med. Sep 15;113(6):455-66. Review.
Holliday R. (2004). The close relationship between
biological aging and age-associated pathologies in humans. J Gerontol A BiolSci Med Sci. Jun;59(6):B543-6.
Holliday R. (2004). The multiple and irreversible
causes of aging. J Gerontol A BiolSci Med Sci. Jun;59(6):B568-72.
Lakatta EG. (2000). Cardiovascular aging in health.
ClinGeriatr Med. Aug;16(3):419-44.
The Aging Body
Thannickal VJ, Henke CA, Horowitz JC, et al. (2014). Matrix Biology of Idiopathic Pulmonary Fibrosis: A Workshop Report of the National Heart, Lung, and Blood Institute. Am J Pathol. Jun;184(6):1643-1651.
Gilissen EP(1), Staneva-Dobrovski L. (2013). Distinct types of lipofuscin pigment in the hippocampus and cerebellum of aged cheirogaleid primates. Anat Rec (Hoboken). Dec;296(12):1895-906.
Grune T. (2013). Lipofuscin: formation, effects and role of macroautophagy. Redox Biol. Jan 19;1(1): 140-144.
Andrade JP, Assunção M. (2012). Protective effects of chronic green tea consumption on age-related neurodegeneration. Curr Pharm Des.;18(1):4-14.
Xu Y, Zhang JJ, Xiong L, et al. (2010). Green tea polyphenols inhibit cognitive impairment induced by chronic cerebral hypoperfusion via modulating oxidative stress. J Nutr Biochem. Aug;21(8):741-8.
Jung T, Höhn A, Grune T. (2010). Lipofuscin: detection and quantification by microscopic techniques. Methods Mol Biol.594:173-93.
Herzog AR, Diokno AC, Brown MB, Normolle DP,
Brock BM. (1990). Two-year incidence, remission, and change patterns of urinary
incontinence in noninstitutionalized older adults. J Gerontol. Mar;45(2):M67-74
Aging changes in organs - tissue - cells http://adam.about.com/ encyclopedia/ 004012.htm
McArdle, JJ. Anderson, E. (1990). Latent
variable growth models for research on aging In Birren, J. E. Schaie, K. W.,
Handbook of the Psychology of Aging, 21-44. Academic Press, New York.
Whitbourne, SK (1996). The aging individual:
Physical and psychological perspectives. New York: Springer.
Whitbourne, SK (1998). Physical changes in
the aging individual: Clinical implications. In Clinical Geropsychology. I. H.
Nordhus, G. R. VandenBos, S. Berg, & P. Fromholt (Eds.).
The Aging Brain
Watanabe M, Sakai O, Ozonoff A, Kussman S, Jara H. (2013). Age-related apparent diffusion coefficient changes in the normal brain. Radiology. Feb;266(2):575-82.
Backman L, Jones S, Small BJ, Aguero-Torres
H, Fratiglioni L. ( 2003). Rate of cognitive decline in preclinical Alzheimer's
disease: the role of comorbidity. J Gerontol B PsycholSciSoc Sci.
Jul;58(4):P228-36.
Ott A, et al (2004). Effect of smoking on global cognitive function in non-demented
elderly. Neurology. Mar 23;62(6):920-4.
Related Articles and Links
Cardiovasculategrity
Hermida RC, Ayala DE, Ríos MT, Fernández JR, Mojón A, Smolensky MH. (2014). Around-the-clock Ambulatory Blood Pressure Monitoring is Required to Properly Diagnose Resistant Hypertension and Assess Associated Vascular Risk. Curr Hypertens Rep. Jul;16(7):445.
Marques F, Sousa JC, Sousa N, Palha JA.( 2013). Blood-brain-barriers in aging and in Alzheimer's disease. Mol Neurodegener. Oct 22;8:38.
Kalantzi KI, Milionis HJ, Goudevenos IA.(2006). Management of the elderly patient with hyperlipidaemia: recent concerns. Hellenic J Cardiol. Mar-Apr;47(2):93-9.
Shah K, Rogers J, Britigan D, Levy C. (2006). Clinical inquiries. Should we identify and treat hyperlipidemia in the advanced elderly? J FamPract. Apr;55(4):356-7.
Brunero S, Lamont S. (2010). Healthbehaviour beliefs and physical health risk factors for cardiovascular disease in an outpatient sample of consumers with a severe mental illness: a cross-sectional survey. Int J Nurs Stud. Jun;47(6):753-60.
Bailey TL, Rivara CB, Rocher AB, Hof PR.
(2004). The nature and effects of cortical microvascular pathology in aging and
Alzheimer's disease. Neurol Res. Jul;26(5):573-8.
Colcombe SJ, et al (2004). Neurocognitive
aging and cardiovascular fitness: recent findings and future directions. J Mol
Neurosci.;24(1):9-14
Personality
Cooper LD, Balsis S, Oltmanns TF. (2014). Aging: empirical contribution. A longitudinal analysis of personality disorder dimensions and personality traits in a community sample of older adults: perspectives from selves and informants. J Pers Disord. Feb;28(1):151-65.
Błachnio A, Buliński L. (2013). Prejudices and elderly patients' personality -- the problem of quality of care and quality of life in geriatric medicine. Med Sci Monit. Aug 16;19:674-80.
Virginia S.Y. Kwan, Michael Harris Bond, Helen C. Bouche. (2002). The Construct of Individuation: More Complex in Collectivist than in Individualist Cultures Pers Soc Psychol Bull March 28: 300-310,
Karen Hooker1 and Dan P. McAdams. (2003). Personality Reconsidered: A New Agenda for Aging Research. Journal of Gerontology:, Vol. 58B, No. 6, P296–P304
Oltmanns TF, Balsis S. (2011). Personality disorders in later life: questions about the measurement, course, and impact of disorders. Annu Rev Clin Psychol.;7:321-49.
American Heart Association. (2001). Heart and
Stroke Statistical Update. Dallas, Texas: American Heart Association.
Baltes, P.B. (1987). Theoretical
propositions of life-span developmental psychology: On the dynamics between
growth and decline. Developmental Psychology, 23: 611-626.
Caspi, A. (1998). Personality development
across the life course. In W. Damon (Ser. Ed.) & N. Eisenberg (Vol. Ed.),
Handbook of Child Psychology, Vol. 3: Social, Emotional, and Personality
Development. New York: John Wiley & Sons, 311-388.
Caspi, A., & Roberts, B.W. (1999).
Personality continuity and change across the life course. In L.A. Pervin, &
O.P. John (eds.), Handbook of Personality: Theory and Research. New York:
Guilford Press, 300-326.
Daniel K. Mroczek, David M. Almeida l (2004).
The Effect of Daily Stress, Personality, and Age on Daily Negative Affect
Journal of Personality Vol. 72 Issue 2 Page 355
Field, D., & Millsap, R.E. (1991).
Personality in advanced old age: Continuity or change? Journal of Gerontology:
Psychological Sciences, 46: 299-308.
Friedman, H.S., Hawley, P.H., & Tucker,
J.S. (1994). Personality, health, and longevity. Current Directions in
Psychological Science, 3: 37-41.
Helson, R., Kwan, V.S.Y., John, O.P., &
Jones, C. (2002). The growing evidence of personality change in adulthood:
Findings from research with personality inventories. Journal of Research in
Personality, 36: 287-306.
Mroczek DK, Almeida DM. (2004). The effect of
daily stress, personality, and age on daily negative affect. J Pers.
Apr;72(2):355-78.
McCrae, R.R., & Costa, P.T. (1990).
Personality in Adulthood. New York: Guilford Press.
Neugarten, B. L. (1964). Personality in
middle and late life. New York: Atherton Press.
Neugarten, B., Havighurst, R. & Tobin,
S. (1961). The measurement of life satisfaction. Journal of Gerontology, 16,
134-43.
Roberts, B.W., & Delvecchio, W.F.
(2000). The rank-order consistency of personality traits from childhood to old
age: A quantitative review of longitudinal studies. Psychological Bulletin,
126: 3-25.
Social Dynamics
de Rigal J, Des Mazis I, Diridollou S, et al. (2010). The effect of age on skin color and color heterogeneity in four ethnic groups. Skin Res Technol. May;16(2):168-78.
Falk H(1), Wijk H, Persson LO. (2011). Frail older persons' experiences of interinstitutional relocation. Geriatr Nurs. Jul-Aug;32(4):245-56.
Laughlin A, Parsons M, Kosloski KD, Bergman-Evans B. (2007). Predictors of mortality following involuntary interinstitutional relocation. J GerontolNurs. 2007 Sep;33(9):20-6; quiz 28-9.
Capezuti E, Boltz M, Renz S, Hoffman D, Norman RG. (2006). Nursing home involuntary relocation: clinical outcomes and perceptions of residents and families. J Am Med Dir Assoc. Oct;7(8):486-92.
Coffman TL. (1981). Relocation and survival
of institutionalized aged: A re-examination of the evidence. The Gerontologist
21(5):483-500.
Coffman, S. and Coffman, V. (1986). Aging
awareness training for professionals who work with the elderly. Small Group
Behavior, 95-103.
Family Dynamics
Family Caregiver Alliance https://www.caregiver.org/
Zanetti AC, Wiedemann G, Dantas RA, et al. (2013). Cultural adaptation and psychometric properties of the family questionnaire in a Brazilian sample of relatives of schizophrenia outpatients. J Clin Nurs. Jun;22(11-12):1521-30.
Murray PD(1), Lowe JD, Horne HL. (1995). Assessing filial maturity through the use of the Filial Anxiety Scale. J Psychol. Sep;129(5):519-29.
Do EK, Cohen SA(1), Brown MJ. (2014). Socioeconomic and demographic factors modify the association between informal caregiving and health in the Sandwich Generation. BMC Public Health. Apr 15;14(1):362
Kathleen Bogolea, MS. (2013). The Sandwich Generation. Today's Caregiver Magazine April 24.
Roane DM, Teusink JP, Wortham JA. (2002). Home visits in geropsychiatry fellowship training.
Gerontologist. Feb;42(1):109-13.
Cicirelli, V. G. (2000). Filial Anxiety Scale (FAS). In B. F. Perlmutter, J. Touliatis, & G. W. Holden (Eds.), Handbook of family measurement techniques, Vol. 3 Measures (pp. 394-395). Thousand Oaks, CA: Sage.
Cicirelli, V. G. (1991). Sibling
relationships in adulthood. In S. P. Pfeifer & M. B. Sussman (Eds.),
Families: Intergenerational and generational connections (pp. 291-310). New
York: Haworth Press. (Reprinted from Marriage and Family Review, 1991, 16(3/4),
291-310
Murray PD(1), Lowe JD, Horne HL. (1995). Assessing filial maturity through the use of the Filial Anxiety Scale. J Psychol. Sep;129(5):519-29.
Filial anxiety scale [FAS] (1988). Cicirelli
VG. IN: Touliatos J; Perlmutter BF & Straus MA (2001). Handbook of family
measurement techniques. (3 vols.) Thousand Oaks, Calif.: Sage Publications.
V.2, pg.224; v.3, pg.394-394.
Video and Audio, Books, Games
iPads Open New World for Manhattan Nursing Home Residents Berkeley College students
help elders navigate new technology. http://jewishhome.org/manhattan-campus/manhattan-campus-news/ipads-open-new-world-for-manhattan-nursing-home-residents/.
The Impact of Medical Illness on Mental
Health
Zhang G, Ding H, Chen H, et al. (2013). Thiamine nutritional status and depressive symptoms are inversely associated among older Chinese adults. J Nutr. 2013 Jan;143(1):53-8.
Eriksson I, Gustafson Y, Fagerström L, Olofsson B. (2011). Urinary tract infection in very old women is associated with delirium. IntPsychogeriatr. Apr;23(3):496-502.
Backman L, Jones S, Small BJ, Aguero-Torres H, Fratiglioni L. (2003). Rate of cognitive decline in preclinical Alzheimer's disease: the role of comorbidity. J Gerontol B PsycholSciSoc Sci. Jul;58(4):P228-36.
Woo BK, Daly JW, Allen EC, Jeste DV, Sewell DD. (2003). Unrecognized medical disorders in older psychiatric inpatients in a senior behavioral health unit in a university hospital. J Geriatr Psychiatry Neurol. Jun;16(2):121-5.
Deijen JB, de Boer H, van der Veen EA. (1998). Cognitive changes during growth hormone
replacement in adult men. Psychoneuroendocrinology, 23:45-55.
Deijen JB, de Boer H, Blok GJ, van der Veen EA. (1996). Cognitive impairments and mood disturbances
in growth hormone deficient men. Psychoneuroendocrinology, 21:313-322.
Moss R, D'Amico S, Maletta G. (1987). Mental
dysfunction as a sign of organic illness in the elderly. Geriatrics. Dec;42(12):35-42.
Sáez JM. (2012). Possible usefulness of growth hormone/insulin-like growth factor-I axis in Alzheimer's disease treatment. Endocr Metab Immune Disord Drug Targets. Sep;12(3):274-86.
Quik EH. Conemans EB, Valk GD, Kenemans JL, Koppeschaar HP, van Dam PS. (2012). Cognitive performance in older males is associated with growth hormone secretion. Neurobiol Aging. Mar;33(3):582-7.
Burman P, Deijen JB. (1998). Quality of life and cognitive function in
patients with pituitary insufficiency. Psychotherapy and Psychosomatics, 1998
67:154-167.
Body Image
Anderson DL Murray CD, Hurrell R. (2013). Experiences of intimacy among people with bladder exstrophy. Qual Health Res. Dec;23(12):1600-12.
Langer-Most O, Langer N. (2010). Aging and sexuality: how much do gynecologists know and care? J Women Aging. Oct;22(4):283-9.
Fooken I. (1994). Sexuality in the later years the
impact of health and body image in a sample of older women. Patient Education
and Counseling, Jul, 23(3):227 33.
Post-Stroke
National Stroke Association: http://www.stroke.org.
Brodtmann A. van de Port IG. (2013). Fitness, depression, and post-stroke fatigue: worn out or weary? Neurology. Oct 29;81(18):1566-7.
Pohjasvaara T, Leskela M, Vataja R, et al. (2002). Post-stroke depression, executive dysfunction and functional outcome. Eur J Neurol. May;9(3):269-75.
Agrell B, Dehlin O. (2000). Mini mental state
examination in geriatric stroke patients. Validity, differences between
subgroups of patients, and relationships to somatic and mental variables. Aging
(Milano). Dec;12(6):439-44.
Andersen G, Vestergaard K, Ingemann-Nielsen
M, Lauritzen L. (1995). Risk factors for post-stroke depression. ActaPsychiatr Scand.
Sep;92(3):193-8.
Andersen G, Vestergaard K, Riis J, Lauritzen
L. (1994). Incidence of post-stroke depression during the first year in a large
unselected stroke population determined using a valid standardized rating
scale. ActaPsychiatr Scand. Sep;90(3):190-5.
Beckson M, Cummings J.L. (1991). Neuropsychiatric
aspects of stroke. Int J Psychiatry Med. ;21(1):1-15. Review.
Burvill P, Johnson G, Jamrozik K, Anderson
C, Stewart-Wynne E. (1997). Risk factors for post-stroke depression. Int J Geriatr
Psychiatry. Feb;12(2):219-26.
Burvill PW, Johnson GA, Jamrozik KD,
Anderson CS, Stewart-Wynne EG, Chakera TM. (1995). Anxiety disorders after stroke:
results from the Perth Community Stroke Study. Br J Psychiatry.
Mar;166(3):328-32.
Chalmers GL. Post-stroke depression. IntClinPsychopharmacol. (1990). Jul;5Suppl 3:21-31. Review.
Currier MB, Murray GB, Welch CC.
(1992). Electroconvulsive therapy for post-stroke depressed geriatric patients. J
Neuropsychiatry ClinNeurosci. Spring;4(2):140-4.
Fenn D, George K. (1999). Post-stroke mania late in
life involving the left hemisphere. Aust N Z J Psychiatry.
Aug;33(4):598-600.
Ghoge H, Sharma S, Sonawalla S, Parikh R.
(2003). Cerebrovascular diseases and depression. Curr Psychiatry Rep. Jul;5(3):231-8. Review.
de Jong HJ(1), Klungel OH, van Dijk L, Vandebriel RJ, Leufkens HG, van der Laan JW, Cohen Tervaert JW, van Loveren H. (2012). Use of statins is associated with an increased risk of rheumatoid arthritis. Ann Rheum Dis. May;71(5):648-54.
House A, Dennis M, Warlow C, Hawton K,
Molyneux A. (1990). The relationship between intellectual impairment and mood disorder
in the first year after stroke. Psychol Med. Nov;20(4):805-14.
Johnson GA. (1991). Research into psychiatric
disorder after stroke: the need for further studies. Aust N Z J Psychiatry.
Sep;25(3):358-70. Review.
Kalaria RN, Ballard C. (2001). Stroke and cognition.
Curr Atheroscler Rep. Jul;3(4):334-9. Review.
Loong CK, Kenneth NK, Paulin ST. (1995). Post-stroke
depression: outcome following rehabilitation. Aust N Z J Psychiatry.
Dec;29(4):609-14.
Madureira S, Guerreiro M, Ferro JM. (2001). Dementia
and cognitive impairment three months after stroke. Eur J Neurol.
Nov;8(6):621-7.
Morris P. Post-stroke depression and general
hospital psychiatry. (1991). Aust N Z J Psychiatry. Dec;25(4):445-6. No abstract
available.
Morris PL, Robinson RG, Raphael B, Bishop D.
(1991). The relationship between the perception of social support and post-stroke
depression in hospitalized patients. Psychiatry. Aug;54(3):306-16.
Morris PL, Robinson RG, Raphael B. (1993). Emotional
lability after stroke. Aust N Z J Psychiatry. Dec;27(4):601-5.
Pohjasvaara T, Leskela M, Vataja R, Kalska
H, Ylikoski R, Hietanen M, Leppavuori A, Kaste M, Erkinjuntti T. (2002). Post-stroke
depression, executive dysfunction and functional outcome. Eur J Neurol.
May;9(3):269-75.
Starkstein SE, Bryer JB, Berthier ML, Cohen
B, Price TR, Robinson RG. (1991). Depression after stroke: the importance of cerebral
hemisphere asymmetries. J Neuropsychiatry ClinNeurosci.
Summer;3(3):276-85.
Dehydration
Goldberg LR, Heiss CJ, Parsons SD, et al. (2014). Hydration in older adults: The contribution of bioelectrical impedance analysis. Int J Speech Lang Pathol. Jun;16(3):273-81
Dimaria-Ghalili RA, Nicolo M. (2014). Nutrition and hydration in older adults in critical care. Crit Care Nurs Clin North Am. Mar;26(1):31-45.
Bennett JA Dehydration: hazards and
benefits. (2000). GeriatrNursMar-Apr;21(2):84-8.
Bennett, J., et al. (2004). Unrecognized Chronic
Dehydration in older adults: examining prevalence rate and risk factors. Geron.
Nursing Nov Vol30 Number 4: 22-28.
Head Trauma
Greig NH, Tweedie D, Rachmany L. et al. (2014). Incretin mimetics as pharmacologic tools to elucidate and as a new drug strategy to treat traumatic brain injury. Alzheimers Dement. Feb;10(1 Suppl):S62-75.
Brain Injury Association of America: www.biausa.org.
Defense and Veterans Brain Injury Center: http://dvbic.dcoe.mil.
Rimel, R., Giordani, B., Barth, J., Jane, J.
(1982). Moderate head injury: completing the clinical spectrum of brain trauma.
Neurosurgery 11(3):344 51.
Robinson, R. (1984). Chronic subdural
hematoma: surgical management in 133 patients. Journal of Neurosurgery
61(2):263 8.
Tsuboi, K., Maki, Y., Nose, T., Matsuki, T.
(1984). Psychiatric symptoms of patients with chronic subdural hematoma.
Neurological Surgery 12(3 Suppl):275 9.
Dizziness
Piker EG(1), Jacobson GP. (2014). Self-report symptoms differ between younger and older dizzy patients. Otol Neurotol. Jun;35(5):873-9.
Momeyer MA. (2014). Orthostatic Hypotension in Older Adults with Dementia. J Gerontol Nurs. Apr 28:1-8.
Colledge NR; Barr-Hamilton RM; Lewis SJ;
Sellar RJ; Wilson JA. (1996). Evaluation of investigations to diagnose the cause of
dizziness in elderly people: a community based controlled study. BMJ (Clinical
Research Ed.), Sep 28, 313(7060): 788-92.
Grimby A; Rosenhall U. (1995). Health-related
quality of life and dizziness in old age [see comments]. Gerontology, ,
41(5):286-98.
Sloane PD; Hartman M; Mitchell CM.
(1994). Psychological factors associated with chronic dizziness in patients aged 60 and
older. Journal of the American Geriatrics Society, Aug, 42(8): 847 -2.
Sullivan M; Clark MR; Katon WJ; Fischl M;
Russo J; Dobie RA; Voorhees R. (1993). Psychiatric and otologic diagnoses in patients
complaining of dizziness [see comments]. Archives of Internal Medicine,
Jun 28, 153(12):1479-84.
Nutritional Deficits
Castro Vilela ME, Merino Taboada AS, Mesa Lampré MP. (2014). [Vitamin D levels in elderly patients hospitalized with hip fracture.] Med Clin (Barc). Mar 22. [Article in Spanish]
Carter T(1), Nutt J, Simons A. (2014). Bilateral femoral neck insufficiency fractures secondary to vitamin D deficiency and concurrent corticosteroid use--a case report. Arch Osteoporos. Dec;9(1):172.
Ocampo Chaparro JM. (2013). Vitamin B12 deficit and development of geriatric syndromes. Colomb Med (Cali). 2013 Mar 30;44(1):42-5. eCollection.
Viveky N, Toffelmire L, Thorpe L, et al. (2012). Use of vitamin and mineral supplements in long-term care home residents. Appl Physiol Nutr Metab. Feb;37(1):100-5.
Bjelland I, Tell GS, Vollset SE, Refsum H,
UelandPM. (2003). Folate, vitamin B12, homocysteine, and the MTHFR 677C->T
polymorphism in anxiety and depression: the HordalandHomocysteine Study. Arch
Gen Psychiatry. Jun;60(6):618-26.
De Castro JM. (1993). Age-related changes in
spontaneous food intake and hunger in humans. Appetite, Dec, 21(3):255-72.
Deijen JB, Slump E, Wouters-Wesseling W, De
Groot CP, Galle E, Pas H. (2003). Nutritional intake and daily functioning of
psychogeriatric nursing home residents. J Nutr Health Aging.;7(4):242-6.
Deijen, BJ. (1992). Vitamin B-6
supplementation in elderly men: effects on mood, memory, performance, and
mental effort. Psychopharmacology, 109:489-496.
Durlach, J. et al. (1993). Magnesium and
ageing. II. Clinical data: aetiological mechanisms and pathophysiological
consequences of magnesium deficit in the elderly. Magnesium Research 6, 4,
379-394 Review paper
Durlach, J. et al. (1998). Magnesium status
and ageing: an update. Magnesium Research. Mar;11(1):25-42
Freedman ML, Ahronheim JC. (1985). Nutritional needs
of the elderly: debate and recommendations. Geriatrics. Aug;40(8):45-9,
53-4, 57-9 passim.
Frizel D., Coppen A., Marks V. (1969).
Plasma magnesium and calcium in depression. British Journal of Psychiatry 115:
p1375 - 7
Hall R.C.W., Joffe J.R. (1973). Hypomagnesemia:
Physical and psychiatric symptoms. JAMA 224: p 1749 - 51
Pennypacker LC; Allen RH; Kelly JP; Matthews
LM; Grigsby J; Kaye K; Lindenbaum J; Stabler SP. (1992). High prevalence of cobalamin
deficiency in elderly outpatients [see comments]. Journal of the American
Geriatrics Society, Dec, 40(12): 1197 204.
Rayssiguier Y, Durlach J, Gueux E, Rock E,
Mazur A (1993). Magnesium and ageing. I. Experimental data: importance of
oxidative damage. Magnesium Research. Dec;6(4):369-78.
Rolls BJ. (1993). Appetite, hunger, and satiety in
the elderly. Critical Reviews in Food Science and Nutrition, 33(1):39-44.
Schiffman SS; Warwick ZS. (1993). Effect of flavor
enhancement of foods for the elderly on nutritional status: food intake,
biochemical indices, and anthropometric measures. Physiology and Behavior,
Feb, 53(2):395-402.
Sidenvall B; Fjellstrom C; Ek AC. (1996). Cultural
perspectives of meals expressed by patients in geriatric care. International
Journal of Nursing Studies, Apr, 33(2):212-22.
Steele CM; Greenwood C; Ens I; Robertson C;
Seidman-Carlson R. (1997). Mealtime difficulties in a home for the aged: not just
dysphagia. Dysphagia, Winter, 12(1):43-50; discussion 51.
Dysphagia
O'Rourke F, Vickers K, Upton C, Chan D. (2014). Swallowing and oropharyngeal dysphagia. Clin Med. Apr;14(2):196-9.
Mayumi Ikeda, RN. Tatsuto Miki, RN, CN. Masako Atsumi, RN. et al. (2014). Effective elimination of contaminants after oral care in elderly institutionalized individuals. Geriatric Nursing 21 April.
Kanna SV, Bhanu K. (2014). A simple bedside test to assess the swallowing dysfunction in Parkinson's disease. Ann Indian Acad Neurol. Jan;17(1):62-5.
Steele CM; Greenwood C; Ens I; Robertson C; Seidman-Carlson R. (1997). Mealtime difficulties in a home for the aged: not just dysphagia. Dysphagia ,12(1):43-50; discussion 51.
Pain
Fine PG, Davis M, Muir C, Schwind D. (2013). Bridging the gap: pain medicine and palliative care. Pain Med. Sep;14(9):1277-9.
Tseng CC, Chen PY, Lee YC. (2014). Successful treatment of phantom limb pain and phantom limb sensation in the traumatic amputee using scalp acupuncture. Acupunct Med. May 22.
[No authors listed] (2005). Management of chronic pain syndromes: issues and interventions. Pain Med. Jul-Aug;6 Suppl 1:S1-S20; quiz S21-S23.
Ramachandran VS. (1998). Consciousness and body image: lessons from phantom limbs, Capgras syndrome and pain asymbolia. Philos Trans R SocLond B Biol Sci. Nov 29;353(1377):1851-9.
Brink TL, Capri D, DeNeeve V, Janakes C,
Oliveira C. (1979). Hypochondriasis and paranoia: similar delusional systems in an
institutionalized geriatric population. J NervMent Dis. Apr;167(4):224-8.
Clark, D. (1999). "Total pain"
disciplinary power and the body in the work of Cicely Saunders, 1958-1967.
Social Science and Medicine, 49, 727-736.
Gehrman PR, Martin JL, Shochat T, Nolan S,
Corey-Bloom J, Ancoli-Israel S. (2003). Sleep-disordered breathing and agitation in
institutionalized adults with Alzheimer disease. Am J Geriatr Psychiatry.
Jul-Aug;11(4):426-33.
Ott A, et al Effect of smoking on global
cognitive function in non-demented elderly Neurology. (2004). Mar 23;62(6):920-4.
Phillips, D.M. (2000). JCAHO pain management
standards are unveiled. Journal of the American Medical Association
284(4):428-429
Medications
Husson N, Watfa G, et al. (2014). Characteristics of polymedicated (≥ 4) elderly: a survey in a community-dwelling population aged 60 years and over. J Nutr Health Aging. Jan;18(1):87-91.
Moura, C. Bernatsky, S. Abrahamowicz, M. et al. (2014). Antidepressant use and 10-year incident fracture risk: the population-based Canadian Multicentre Osteoporosis Study (CaMoS).
Joe and Terry Graeden The People's Pharmacy (2014).
http://www.peoplespharmacy.com/.
Graeden Joe (1996). The People's Pharmacy, St Martins Press, Revised edition.
Cumming RG; Miller JP; Kelsey JL; Davis P;
Arfken CL; Birge SJ; Peck WA. (1991). Medications and multiple falls in elderly people:
the St Louis OASIS study. Age and Ageing, Nov, 20(6): 455-61.
Simoni-Wastila, L. (2000). The use of abusable
prescription drugs: The role of gender. Journal of Women's Health and
Gender-based Medicine 9(3):289-297.
Wilford, B.B; Finch, J.; Czechowicz, D.J.;
and Warren D. (1994). An overview of prescription drug misuse and abuse: Defining the
problem and seeking solutions. Journal of Law, Medicine, & Ethics 22(3):197-203.
Substance Abuse
Blake V. (2013). Fighting prescription drug abuse with federal and state law. Virtual Mentor. May 1;15(5):443-8.
American Psychiatric Association.
(1990). Benzodiazepine Dependence, Toxicity, and Abuse: A Task Force Report of the
American Psychiatric Association. Washington, DC: American Psychiatric
Association.
CSAT. (2000). Substance Abuse Among Older Adults
(TIP #26): Physicians Guide. DHHS Pub. No. (SMA) 00-3394. SAMHSA.
Johnston, L.D.; O'Malley, P.M.; and Bachman,
J.G. (2000). Monitoring the Future: National Survey Results on Drug Use, 1975-1999, 2
Vols. NIH Pub. No. 00-4803. National Institute on Drug Abuse (NIDA), NIH, DHHS
Joransson, D.E.; Ryan, K.M.; Gilson, A.M.;
and Dahl, J.L. (2000). Trends in medical use and abuse of opioid analgesics. Journal of
the American Medical Association 283(13):1710-1714.
Longo, L.P., and Johnson, B. (2000). Addiction: Part
I. Benzodiazepines-side effects, abuse risk, and alternatives. American Family
Physician 61:2121-2131.
Longo, L.P.; Parran, T.; Johnson, B.; and
Kinsey, W. (2000). Addiction: Part II. Identification and management of the
drug-seeking patient. American Family Physician 61:2401-2408.
National Center on Addiction and Substance
Abuse at Columbia University (CASA). (2000). Missed Opportunity: National Survey of
Primary Care Physicians and Patients on Substance Abuse. New York: CASA.
NIDA NOTES. (2000). Research eases concerns about
use of opioids to relieve pain, NIDA NOTES 15(1):12-13.
Office of Applied Studies. (1997). Substance Use
among Women in the United States. DHHS Pub. No. (SMA) 97-3162. SAMHSA.
Office of Applied Studies. (2000). Year-End 1999
Emergency Department Data from the Drug Abuse Warning Network. DHHS Pub.
No.(SMA) 00-3462. SAMHSA.. http://www.samhsa.gov/.
Drug Abuse Warning Network: National Estimates of Drug-Related Emergency Department Visits (2011). SAMHSA.
Patterson, T.L., and Jeste, D.V. (1999). The
potential impact of the baby-boom generation on substance abuse among elderly
persons. Psychiatric Services 50:1184-1188.
Ryle PR, Thomson AD. (1984). Nutrition and vitamins
in alcoholism. Contemp Issues ClinBiochem. 1:188-224. Review.
Sexual Problems
Wang V, Depp CA, Ceglowski J. et al. (2014). Sexual Health and Function in Later Life: A Population-Based Study of 606 Older Adults with a Partner. Am J Geriatr Psychiatry. Mar 19.
Inelmen EM(1), Sergi G, De Rui M, Manzato E. (2014). Enhancing awareness to mitigate the risk of HIV/AIDS in older adults. Aging Clin Exp Res.
Faria G. (1997). The challenge of health care social
work with gay men and lesbians. Soc Work Health Care. 25(1-2):65-72.
Hobson KG. (1984). The effects of aging on
sexuality. Health Soc Work. Winter;9(1):25-35.
Kobosa-Munro L. (1977). Sexuality in the aging
woman. Health Soc Work. Nov;2(4):70-88.
McGrath FJ, Robinson JS. (1973). The medical social
worker in the coronary care unit. Med J Aust. Dec 22;2(25):1113-6. No
abstract available.
van Lunsen RH, Laan E. (2004). Genital vascular
responsiveness and sexual feelings in midlife women: psychophysiologic, brain,
and genital imaging studies. Menopause. Nov-Dec;11(6):741-8.
Sleep
Gamaldo CE, Shaikh AK, McArthur JC. (2012). The sleep-immunity relationship. Neurol Clin. Nov;30(4):1313-43.
Asghari A, Mohammadi F, Kamrava et al. (2013). Evaluation of quality of life in patients with obstructive sleep apnea. Eur Arch Otorhinolaryngol. Mar;270(3):1131-6.
Mermigkis C, Bouloukaki I, Antoniou KM, et al. (2013). CPAP therapy in patients with idiopathic pulmonary fibrosis and obstructive sleep apnea: does it offer a better quality of life and sleep? Sleep Breath.
Irwin M. (2002). Effects of sleep and sleep loss on immunity and cytokines. Brain Behav Immun. Oct;16(5):503-12. Review.
Irwin, M., Clark, C., Kennedy. B., Christian. Gillin J., Ziegler, M. (2003). Nocturnal catecholamines and immune function in insomniacs, depressed patients, and control subjects. Brain Behav Immun. Oct;17(5):365-72.
Ancoli-Israel S, Klauber MR, Butters N, Parker L, Kripke DF (1990). Dementia in Institutionalized Elderly: Relation to Sleep Apnea. Journal of the American Geriatrics Society; 39(3):258-63.
Chase, M. (1979). Every 90 Minutes a
Brainstorm. Psychology Today Nov.
Folkard, S. (1982). Circadian rhythms and
human memory. Rhythmic Aspects of Human Behavior. F. Brown and R. Graeber, eds.
Erlbaum Associates, Hillsdale NJ, p313 344
Folkard, S., Knauth, P., Monk, T. H. (1976). The
effect of memory load on the circadian variation in performance efficiency
under a rapidly rotating shift system. Ergonomics. Jul;19(4):479-88.
Hoddes, E. (1977). Does Sleep Help You Study?
Psychology Today, April.
Kripke (1982). Ultradian Rhythms in behavior
and physiology. Rhythmic Aspects of Human Behavior, F. Brown and R. Graeber,
eds, Erlbaum Associates, Hillsdale NJ.
Lichstein, M. (1990). Low sleep need causes
confusion. Brain/Mind Bulletin 15(7). Originally in Behavior Therapy 19: 625
632
Monk, T. H., Folkard, S. (1976). Adjusting to the
changes to and from Daylight Saving Time. Nature. Jun 24;261(5562):688-9.
Monk, T. H., Knauth, P., Folkard, S.,
Rutenfranz, J. (1978). Memory based performance measures in studies of shiftwork.
Ergonomics. Oct;21(10):819-26.
Nair NP, Hariharasubramanian N. (1984). Circadian
rhythms and psychiatry. Br J Psychiatry. Nov;145:557-8. No abstract
available.
Nair NP, Hariharasubramanian N, Pilapil C.
(1984). Circadian rhythm of plasma melatonin in endogenous depression. ProgNeuropsychopharmacol Biol Psychiatry. 8(4-6):715-8.
Nair NP, Hariharasubramanian N, Pilapil C,
Isaac I, Thavundayil JX. (1986). Plasma melatonin–an index of brain aging in humans?
Biol Psychiatry. Feb;21(2):141-50.
Nair NP, Hariharasubramanian N, Pilapil C,
Isaac I, Thavundayil JX. (1986). Plasma melatonin rhythm in normal aging and
Alzheimer's Disease J. Neural. Transm. 21, S. 494
Palombo, S. (1978). Dreaming and Memory. Basic
Books, NY.
Prolo, P., Chiappelli, F., Fiorucci, A.,
Dovio, A., Sartori, M. L., Angeli, A. (2002). Psychoneuroimmunology: new avenues of
research for the twenty-first century. Ann N Y Acad Sci. Jun;966:400-8.
Review.
Rasmunsen (1986). Physiological interactions
of the basic rest activity cycle of the brain. 11(4) 389 405.
Roffwarg, H., et al. (1978). The effects of
sustained alterations of waking visual input on dream content. The Mind in
Sleep: Psychology and Psychophysiology. Arkin, Antrobus, and Ellman, eds.
Lawrence Erlbaum. Hillsdale NJ. p295.
Rubin, Z. (1979). Seasonal Rhythms in
Behavior. Dec.
Savard, J., Laroche, L., Simard, S., Ivers,
H., Morin, C. M. (2003). Chronic insomnia and immune functioning. Psychosom Med. Mar-Apr;65(2):211-21.
Delirium
Blazer, Dan (2013). Neurocognitive Disorders in DSM-5 Am J Psychiatry.170:585-587.
Maria Yang, MD (2013). DSM-5: Delirium. December 21.
Edmands MS. (1995). "Murder!" she said: a
case of iatrogenic delirium. Issues in Mental Health Nursing, Mar Apr,
16(2):109 16.
Evans. L. (1987). Sundown syndrome in
institutionalized elderly. Am. Geriat. Soc., 35(5), 101.
Kroeger, L. L. (1991). Critical care nurses'
perceptions of the confused elderly patient, Focus on Critical Care, 18(5).
395.
Levkofl. 5. E.. Evans. O. A., et al. (1992).
Delirium: The occurrence and persistence of symptoms among elderly hospitalized
patients. Arch. Intern. Med. 152:21 33.
Patkar AA; Kunkel EJ. (1997). Treating delirium
among elderly patients. Psychiatric Services, Jan, 48(1):46 8.
Schor. J. D., Levkoll, S. E. el al. (1992).
Risk factors for delirium In hospitalized elderly. JAMA. 267(6), 27.
Yeaw EM; Abbate JH. (1993). Identification of confusion
among the elderly in an acute care setting. Clinical Nurse Specialist,
Jul, 7(4):192 7.
The Impact of Memory and Cognitive Decline
Huntley JD(1), Howard RJ. (2010). Working memory in early Alzheimer's disease: a neuropsychological review.Int J Geriatr Psychiatry. Feb;25(2):121-32.
deJager, C. A., Milwain, E., Badge, M.
(2002). Early detection of isolated memory deficits in the elderly: the need for more
sensitive neuropsychological tests. Psychol Med. Apr;32(3):483-91.
Age Associated Memory Impairment
Gazzaley A(1), Cooney JW, Rissman J, D'Esposito M. (2005). Top-down suppression deficit underlies working memory impairment in normal aging. Nat Neurosci. Oct;8(10):1298-300.
Crook, T., Bartus, R., Ferris, S.,
Whitehouse, P., Cohen, G., Gershon, S. (1986). Age associated memory impairment:
proposed diagnostic criteria and measures of clinical change Report of a
National Institute of Mental Health Workgroup. Developmental Neuropsychology
2(4): 261 276.
Crook, T., Larrabee, G. (1988). Age
associated memory impairment: diagnostic criteria and treatment strategies.
Psychopharmacology Bulletin 24(4): 509 514.
Krzyminski, S. (1995). Age-associated memory
impairment. Psychiatr Pol. May-Jun;29(3):319-31. Review. Polish.
Marwick, C. (1993). What is age associated
memory impairment? JAMA, The Journal of the American Medical Association 269
(1):356.
Youngjohn, J., Crook, T., (1993). Stability
of everyday memory in age associated memory impairment: A longitudinal study.
Neuropsychology v7 (n3):406 416.
Youngjohn, J., Larrabee, G., Crook, T.
(1992). Discriminating age associated memory impairment from Alzheimer's
disease. Psychological Assessment 4 (1):54 59.
Mild Cognitive Impairment
Gates N, Valenzuela M, Sachdev PS, et al. (2014). Psychological well-being in individuals with mild cognitive impairment. Clin Interv Aging. May 8;9:779-92.
Reisberg B, Shulman MB, Torossian C, det al. (2010). Outcome over seven years of healthy adults with and without subjective cognitive impairment. Alzheimers Dement. Jan;6(1):11-24.
Grundman, M., et al. (2004). Mild cognitive
impairment can be distinguished from Alzheimer disease and normal aging for
clinical trials. Arch Neurol. Jan;61(1):59-66.
Jungwirth, S., Fischer, P., Weissgram, S.,
Kirchmeyr, W., Bauer, P., Tragl, K. H. (2004). Subjective memory complaints and
objective memory impairment in the Vienna-Transdanube aging community. J Am
Geriatr Soc. Feb;52(2):263-8.
Neurologic Center of South Florida, Psy. D.,
8940 N. Kendall Drive, Suite 802-E, Miami, FL 33176, USA. rafrv@bellsouth.net
Petersen, R. C., Smith, G. E., Waring, S.
C., Ivnik, R. J., Tangalos, E. G., Kokmen, E. (1999). Mild cognitive impairment:
clinical characterization and outcome. Arch Neurol. Mar;56(3):303-8.
Ritchie, K., Artero, S,. Touchon, J.
(2001). Classification criteria for mild cognitive impairment: a population-based
validation study. Neurology. Jan 9;56(1):37-42.
Rivas-Vazquez, R. A., Mendez, C., Rey, G.
J., Carrazana, E. J. (2004). Mild cognitive impairment: new neuropsychological and
pharmacological target. Arch ClinNeuropsychol. Jan;19(1):11-27.
Rosler, A., Gonnenwein, C., Muller, N.,
Sterzer, P., Kleinschmidt, A., Frolich, L. (2004). The Fuzzy Frontier between
Subjective Memory Complaints and Early Dementia. A Survey of Patient Management
in German Memory Clinics. Dement GeriatrCognDisord. 2004;17(3):222-230. Epub
Jan 20.
Scali, Bruce. (2004). Life Extension for the Brain.
Life Extension Magazine. March.
Dementia
Bernardin F, Maheut-Bosser A, Paille F. (2014). [Cognitive impairment of alcohol-dependent subject]. Rev Prat. Apr;64(4):462-5. [Article in French]
Widmann CN, Heneka MT. (2014). Long-term cerebral consequences of sepsis. Lancet Neurol. Jun;13(6): 630-6.
Juliann Schaeffer. (2014). Music Therapy in Dementia Treatment – Recollection Through Sound. Today’s Geriatric Medicine. Feb;28(2):84-90.
Grigsby J, Kaye K, Robbins LJ. (1995). Behavioral
disturbance and impairment of executive functions among the elderly. Arch
GerontolGeriatr. Sep-Oct;21(2):167-77.
Hanon C, Pinquier C, Gaddour N, Said S,
Mathis D, Pellerin J. (2004). [Diogenes syndrome: a transnosographic approach.] Encephale. Jul-Aug;30(4):315-22. [Article in French]
Leel-Ossy L. (1995). Incidence of Alzheimer's
dementia in homes for the elderly. Arch GerontolGeriatr.
Jul-Aug;21(1):21-6.
Reversible Dementias
Clarfield AM. (2003). The decreasing prevalence of
reversible dementias: an updated meta-analysis. Arch Intern Med. Oct
13;163(18):2219-29.
Freter, S. Bergman, H. Gold, S. Chertkow, H.
and. Clarfield A. M (1998). Prevalence of potentially reversible dementias and
actual reversibility in a memory clinic cohort Canadian Medical Association
Journal, Vol 159, Issue 6 657-662.
Freter, S et al. (1998). Prevalence of potentially
reversible dementias and actual reversibility in a memory clinic cohort .CMAJ; 159:657-62.
Subcortical Dementias
Stefani A, Brusa L, Olivola E, et al. (2012). CSF and clinical hallmarks of subcortical dementias: focus on DLB and PDD. J Neural Transm. Jul;119(7):861-75.
Akiguchi I, Tomimoto H, Wakita H., et al. (2004). Topographical and cytopathological
lesion analysis of the white matter in Binswanger's disease brains. ActaNeuropathol (Berl). Jun;107(6):563-70. Epub 2004 Apr 15.
AntonelliIncalzi R, Marra C, Salvigni BL, et al. (2004). Does cognitive dysfunction conform
to a distinctive pattern in obstructive sleep apnea syndrome? J Sleep Res.
Mar;13(1):79-86.
Bosboom JL, Stoffers D, WoltersECh.
(2004). Cognitive dysfunction and dementia in Parkinson's disease. J Neural Transm.
Oct-Nov;111(10-11):1303-15.
Chen CP. (2004). Transcultural expression of
subcortical vascular disease. J Neurol Sci. Nov 15;226(1-2):45-7.
Gainotti G, Acciarri A, Bizzarro A, et al. (2004). The role of brain
infarcts and hippocampal atrophy in subcortical ischaemic vascular dementia.
Neurol Sci. Oct;25(4):192-7.
Kwak YT. (2004). "Closing-in" phenomenon
in Alzheimer's disease and subcortical vascular dementia. BMC Neurol. Jan
26;4(1):3.
Stolze H, Klebe S, Baecker C, Zechlin C,
Friege L, Pohle S, Deuschl G. (2004). Prevalence of gait disorders in hospitalized
neurological patients. MovDisord. Aug 18; [Epub ahead of print]
Takao M, Ghetti B, Yoshida H, Piccardo P,
Narain Y, Murrell JR, Vidal R, Glazier BS, Jakes R, Tsutsui M, Spillantini MG,
Crowther RA, Goedert M, Koto A. (2004). Early-onset dementia with Lewy bodies. Brain
Pathol. Apr;14(2):137-47.
Usui C, Inoue Y, Kimura M, Kirino E, Nagaoka
S, Abe M, Nagata T, Arai H. (2004). Irreversible subcortical dementia following high
altitude illness. High Alt Med Biol. Spring;5(1):77-81.
van Dijk EJ, Breteler MM, Schmidt R, Berger
K, Nilsson LG, Oudkerk M, Pajak A, Sans S, de Ridder M, Dufouil C, Fuhrer R,
Giampaoli S, Launer LJ, Hofman A. (2004). CASCADE Consortium. The association between
blood pressure, hypertension, and cerebral white matter lesions: cardiovascular
determinants of dementia study. Hypertension. Nov;44(5):625-30. Epub 2004
Oct 04.
Depression
Marina Marcus, M. Taghi Yasamy, Mark van Ommeren, and Dan Chisholm, Shekhar Saxena. (2012). DEPRESSION: A Global Public Health Concern. WHO October
Koopmans RT, Zuidema SU, Leontjevas R, Gerritsen DL. (2010). Comprehensive assessment of depression and behavioral problems in long-term care.IntPsychogeriatr. Nov;22(7):1054-62.
Fournier JC, DeRubeis RJ, Hollon SD, Dimidjian S, Amsterdam JD, Shelton RC, Fawcett J. (2010). Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA. Jan 6;303(1):47-53.
Wolkowitz OM, Reus VI, Mellon SH. (2011). Of sound mind and body: depression, disease, and accelerated aging. Dialogues Clin Neurosci.;13(1):25-39.
Alexopoulos GS; Vrontou C; Kakuma T; Meyers
BS; Young RC; Klausner E; Clarkin J. (1996). Disability in geriatric depression.
American Journal of Psychiatry, Jul, 153(7):877 85.
Anderson B; Zubenko GS; Houck PR; George CJ;
Kupfer DJ. (1995). Complicated grief and bereavement related depression as distinct
disorders: preliminary empirical validation in elderly bereaved spouses.
American Journal of Psychiatry, Jan, 152(1):22 30.
Bell IR; Edman JS; Morrow FD; Marby DW;
Perrone G; Kayne HL; Greenwald M; Cole JO. (1992). Brief communication. Vitamin B1, B2,
and B6 augmentation of tricyclic antidepressant treatment in geriatric
depression with cognitive dysfunction. Journal of the American College of
Nutrition, Apr, 11(2):159 63.
Brodaty H. (1993). Think of depression: atypical presentations in the elderly. Australian
Family Physician, Jul, 22(7):1195 203.
Conn DK; Goldman Z. (1992). Pattern of use of
antidepressants in long term care facilities for the elderly. Journal of
Geriatric Psychiatry and Neurology, Oct Dec, 5(4):228 32.
Devanand DP; Nobler MS; Singer T; Kiersky
JE; Turret N; Roose SP; Sackeim HA. (1994). Is dysthymia a different disorder in the
elderly? American Journal of Psychiatry, Nov, 151(11):1592 9.
Prigerson
HG; Frank E; Kasl SV; Reynolds CF 3rd; Gaupp R, Berrios GE, Pomarol-Clotet E.
(2000). Depressive states in old age. (Classic Text No. 42).History of Psychiatry. Jun; 11 Pt 2(42):213-25.
Glassman AH. (2001). Excess mortality via the
interactions of depression and heart disease. Program and abstracts of the
American Association for Geriatric Psychiatry 14th Annual Meeting; February
23-26; San Francisco, California.
Kennedy GJ, Roose S, Glassman AH. (2001). Heart
disease and depression: reducing the fatal interactions. Program and abstracts
of the American Association for Geriatric Psychiatry 14th Annual Meeting;
February 23-26; San Francisco, California. Abstract ME.
Lee MA; Ganzini L. (1992). Depression in the
elderly: effect on patient attitudes toward life sustaining therapy [see
comments]. Journal of the American Geriatrics Society, Oct, 40(10):983 8.
Markovitz PJ. (1993). Treatment of anxiety in the
elderly. Journal of Clinical Psychiatry, May, 54 Suppl:64-8.
Masand PS, Kaplan DS, Gupta S, et al. (1995).
Major depression and irritable bowel syndrome: is there a relationship? J Clin
Psychiatry.;56:363-367.
Morris PLP, Robinson RG, Andreezewski P, et
al. (1993). Association of depression with 10-year post stroke mortality. Am J
Psychiatry. 150:124-129.
Orengo CA, Fullerton G, Tan R. (2004). Male depression: a review of gender concerns
and testosterone therapy. Geriatrics. Oct;59(10):24-30
Passik SD, Dugan W, McDonald MV, Rosenfeld
B, Theobald DE, Edgerton S. (1998). Oncologists' recognition of depression in
their patients with cancer. J ClinOncol. Apr;16(4):1594-600.
Reynolds CF 3rd. (1995). Recognition and
differentiation of elderly depression in the clinical setting. Geriatrics,
Oct, 50 Suppl 1:S6 15.
Roose S. (2001). Physiological reciprocity of heart
disease, depression, and antidepressants. Program and abstracts of the American
Association for Geriatric Psychiatry 14th Annual Meeting; February 23-26,
San Francisco, California.
Roose SP. (2000). Considerations for the use of
antidepressants in patients with cardiovascular disease. Am Heart J.
140:84-88.
Rothschild AJ. (1996). The diagnosis and treatment
of late life depression. Journal of Clinical Psychiatry, 57 Suppl 5:5 11.
Wayne J. Katon, MD; Elizabeth Lin, MD, MPH;
Joan Russo, PhD; Jürgen Unützer, MD, MPH (2003). Increased Medical Costs of a
Population-Based Sample of Depressed Elderly Patients Arch Gen Psychiatry.
60:897-903.
Whyte EM, Pollock BG, Wagner WR, et al.
(2001). Platelet activation in older depressed subjects. Program and abstracts of the
American Association for Geriatric Psychiatry 14th Annual Meeting; February
23-26; San Francisco, California. Abstract SuQ9.
Anxiety
Arnold EM. (2004). Factors that influence
consideration of hastening death among people with life-threatening illnesses.
Health Soc Work. Feb;29(1):17-26.
Jonson M, Skoog I, Marlow T, Mellqvist Fässberg M, Waern M. (2012). Anxiety symptoms and suicidal feelings in a population sample of 70-year-olds without dementia. Int Psychogeriatr. Nov;24(11):1865-71.
Lauderdale SA, Sheikh JI. (2003). Anxiety disorders in older adults. ClinGeriatr Med. Nov; 19(4):721-41. Review.
Gray, J.A. et al (1985). emotional behavior
and the limbic system Advances in Psychosomatic Medicine. 13:1-25.
Kleban MM, Brody EM. (1972). Prediction of
improvement in mentally impaired aged: personality ratings by social workers. J
Gerontol. Jan;27(1):69-76.
Lupien, S. Meaney, M (1998). Stress,
glucocorticoids, and hippocampal aging in rat and human In Handbook of the
Aging Brain Wang & Snyder, eds, p 19-50.
Marriott P; Smith R. (1993). The elderly
agoraphobic: a hidden problem. Australian Family Physician, Nov, 22(11):2036-7,
2040-1, 2044-5.
Raj BA; Corvea MH; Dagon EM. (1993). The clinical
characteristics of panic disorder in the elderly: a retrospective study.
Journal of Clinical Psychiatry, Apr, 54(4):150-5.
Roberts CS, Cox CE, Shannon VJ, Wells NL. (1994). A
closer look at social support as a moderator of stress in breast cancer. Health
Soc Work. Aug;19(3):157-64.
Roskin M. (1982). Coping with life changes – a
preventive social work approach. Am J Community Psychol. Jun;10(3):331-40.
Simington JA; Laing GP. (1993). Effects of
therapeutic touch on anxiety in the institutionalized elderly. Clinical Nursing
Research, Nov, 2(4): 438- 50.
Tucker GJ. (1994). Introduction. Part I.
Treatment approaches to anxiety, depression, and aggression in the elderly.
Journal of Clinical Psychiatry, Feb, 55 Suppl:3-4.
Loss and Grief
PEARLS http://www.pearlsprogram.org/Our-Program/PEARLS-for-Older-Adults.aspx
Ciechanowski P, Wagner E, Schmaling K. (2004). Community-integrated home-based depression treatment in older adults: a randomized controlled trial. JAMA. Apr 7;291(13):1569-77.
England M. (2004). Association of caregiver planning
with recent experiences of crisis. Int J PsychiatrNurs Res.
Aug;10(1):1111-35.
Grimby A. (1993). Bereavement among elderly people:
grief reactions, post-bereavement hallucinations, and quality of life. ActaPsychiatricaScandinavica, Jan, 87(1):72-80.
Weinberg N. (1995). Does apologizing help? The role
of self-blame and making amends in recovery from bereavement. Health Soc Work.
Nov;20(4):294-9.
Suicide
SAVE http://www.save.org/index.cfm?fuseaction=home.viewPage&page_id=1
American Association for Marriage and Family (AAMFT) Suicide_in_the_Elderly
Prevention of Suicide in Primary Care Elderly: Collaborative Trial (PROSPECT)
Bruce ML, Pearson JL. (1999). Designing an intervention to prevent suicide: PROSPECT (Prevention of Suicide in Primary Care Elderly: Collaborative Trial). Dialogues Clin Neurosci. Sep;1(2):100-12.
Bron B. (1992). [Depression and suicide in the
elderly]. Zeitschrift fur Gerontologie, Jan Feb, 25(1): 43 52.
Bruce ML, et al. (2004). Reducing suicidal ideation
and depressive symptoms in depressed older primary care patients: a randomized
controlled trial. JAMA. Mar 3;291(9):1081-91.
Canetto SS. (1992). Gender and suicide in the
elderly. Suicide and Life Threatening Behavior, Spring, 22(1):80 97.
Canetto SS, Sakinofsky I. (1998). The gender paradox
in suicide. Suicide Life Threat Behav. Spring;28(1):1-23
Casey DA. (1990). Suicide in the elderly. Journal of
the Kentucky Medical Association, Jun, 88(6): 301.
Casey DA. (1991). Suicide in the elderly: a two-year
study of data from death certificates [see comments]. Southern Medical Journal,
Oct, 84(10): 1185 7.
Conwell Y. (1992). Suicide in the elderly [see
comments]. Crisis, 13(1):6 8.
De Leo D; Ormskerk SC. (1991). Suicide in the
elderly: general characteristics. Crisis, Sep, 12(2): 3 17.
Duffy D. (1997). Suicide in later life: how to spot
the risk factors. Nursing Times, Mar 12 18, 93(11): 56 7.
Galanos, AN. (1992). Suicide in the elderly [letter;
comment]. Southern Medical Journal, Mar, 85(3):331.
Harvath TA, Miller LL, Goy E, Jackson A,
Delorit M, Ganzini L. (2004). Voluntary refusal of food and fluids: attitudes of Oregon
hospice nurses and social workers Int J PalliatNurs. May;10(5):236-41;
discussion 242-3.
Heiss HW. (1992). [Restriction or fulfillment.
Ethical topics on suicide and sexuality of the elderly]. Wiener MedizinischeWochenschrift, 142 (23 24): 1 p. following 538.
Hochbaum GM. (1992). Suicide by the elderly [letter;
comment]. American Journal of Public Health, Aug, 82(8):1175.
Horton Deutsch SL; Clark DC; Farran CJ.
(1992). Chronic dyspnea and suicide in elderly men. Hospital and Community Psychiatry,
Dec, 43(12):1198 203.
Humphry D. (1992). Rational suicide among the
elderly. Suicide and Life Threatening Behavior, Spring, 22(1):125 9.
Kerkhof A; de Leo D. (1991). Suicide in the elderly:
a frightful awareness. Crisis, Sep, 12(2):81 7.
Kua EH; Ko SM. (1992). A cross cultural study of
suicide among the elderly in Singapore. British Journal of Psychiatry,
Apr, 160:558 9.
Lester D; Yang B. (1992). Social and economic
correlates of the elderly suicide rate. Suicide and Life Threatening Behavior,
Spring, 22(1):36 47.
Loebel JP; Loebel JS; Dager SR. (1991). Centerwall
BS; Reay DT. Anticipation of nursing home placement may be a precipitant of suicide
among the elderly. Journal of the American Geriatrics Society, Apr,
39(4):407 8.
Lyness JM; Conwell Y; Nelson JC. (1992). Suicide
at-tempts in elderly psychiatric inpatients. Journal of the American Geriatrics
Society, Apr, 40(4): 320 4.
McIntosh JL. (1992). Epidemiology of suicide in the
elderly. Suicide and Life Threatening Behavior, Spring, 22(1):15 35.
Mellick E; Buckwalter KC; Stolley JM.
(1992). Suicide among elderly white men: development of a profile. Journal of
Psychosocial Nursing and Mental Health Services, Feb, 30(2):29 34.
Nieto E; Vieta E; Lazaro L; Gasto C; Cirera
E. (1992). Serious suicide attempts in the elderly. Psychopathology, 25(4):183 8.
Pfaff JJ, Almeida OP (2004). Identifying suicidal
ideation among older adults in a general practice setting. J Affect Disord.
Nov 15;83(1):73-7
Rao AV. (1991). Suicide in the elderly: a report
from India. Crisis, Sep, 12(2):33 9.
Rifai AH; Reynolds CF; Mann JJ. (1992). Biology of
elderly suicide. Suicide and Life Threatening Behavior, Spring, 22(1):48
61.
Schmid H; Manjee K; Shah T. (1994). On the
distinction of suicide ideation versus attempt in elderly psychiatric
inpatients. Gerontologist, Jun, 34(3): 332 9.
Skoog I; Aevarsson O; Beskow J; Larsson L;
Palsson S; Waern M; Landahl S; Ostling S. (1996). Suicidal feelings in a population
sample of non-demented 85 year olds. American Journal of Psychiatry, Aug,
153(8):1015 20.
Sverre JM. Trends in suicide mortality among
the elderly in Norway. (1966, 1986). Epidemiology, 1991 Jul, 2(4):252 6.
Tatai K; Tatai K. (1991). Suicide in the elderly: a
report from Japan. Crisis, Sep, 12(2):40 3.
Barriers to Diagnosis
Barton C, Miller B, Yaffe K. (2003). Evaluation of
the diagnosis and management of cognitive impairment in long-term care.
Alzheimer Dis Assoc Disord. Apr-Jun;17(2):72-6.
Carlson LE, Angen M, Cullum J, Goodey E,
Koopmans J, Lamont L, MacRae JH, Martin M, Pelletier G, Robinson J, Simpson JS,
Speca M, Tillotson L, Bultz BD. (2004). High levels of untreated distress and fatigue
in cancer patients. Br J Cancer. Jun 14;90(12):2297-304.
Seedat S, Stein DJ, Berk M, Wilson Z.
(2002). Barriers to treatment among members of a mental health advocacy group in South
Africa. Soc Psychiatry PsychiatrEpidemiol. Oct;37(10):483-7.
Simon GE, Fleck M, Lucas R, Bushnell DM;
LIDO Group. (2004). Prevalence and predictors of depression treatment in an
international primary care study. Am J Psychiatry. Sep;161(9):1626-34.
Barriers to Treatment
Katon W, et al. (1999). Stepped collaborative care
for primary care patients with persistent symptoms of depression: a randomized
trial. Arch Gen Psychiatry. Dec;56(12):1109-15.
Unutzer J. (2002). Diagnosis and treatment of older
adults with depression in primary care. Biol Psychiatry. Aug
1;52(3):285-92. Review.
Assessing the Older Mind
Butler R. (2004). Evaluating an education project in
mental health of older people. Nurs Times. Aug 31-Sep 6;100(35):38-40.
Rosenthal RA, Kavic SM. Assessment and
management of the geriatric patient. (2004). Crit Care Med. Apr;32(4
Suppl):S92-105. Review.
Van Citters AD, Bartels SJ. (2004). A systematic review of the effectiveness of community-based mental health outreach services for older adults .Psychiatr Serv. Nov;55(11):1237-49.
Gillies D. (1999). Elderly trauma: they are different. AustCrit Care. Mar;12(1):24-30. Review.
Sinoff G, Ore L. (1997). The Barthel activities of
daily living index: self-reporting versus actual performance in the old-old
(> or = 75 years). J Am Geriatr Soc. Jul;45(7):832-6.
Links of Interest
For data on the status of the long-term care industry go to the American Health
Care Association
For information on long term care issues http://www.rwjf.org/
For information on magnesium, aging, and metal health, visit The Magnesium
Web Site http://www.mgwater.com/lista.shtml
For information on not-for-profit nursing homes, continuing care retirement
communities, assisted living and senior housing facilities, and home and community-based
service providers, look at the Leading Age website (formerly known as the American Association of Homes and Services for
the Aging) http://www.leadingagemenh.org/
For information on substance abuse issues, visit Florida Alcohol and Drug Administration http://www.fadaa.org/


 ContinuingEdCourses.Net is approved by the American Psychological Association (APA) to sponsor continuing education for psychologists. ContinuingEdCourses.Net maintains responsibility for this program and its content.
ContinuingEdCourses.Net is approved by the American Psychological Association (APA) to sponsor continuing education for psychologists. ContinuingEdCourses.Net maintains responsibility for this program and its content. ContinuingEdCourses.Net, provider #1107, is approved as an ACE provider to offer social work continuing education by the Association of Social Work Boards (ASWB) Approved Continuing Education (ACE) program. Regulatory boards are the final authority on courses accepted for continuing education credit. ACE provider approval period: 3/9/2005-3/9/2027.
ContinuingEdCourses.Net, provider #1107, is approved as an ACE provider to offer social work continuing education by the Association of Social Work Boards (ASWB) Approved Continuing Education (ACE) program. Regulatory boards are the final authority on courses accepted for continuing education credit. ACE provider approval period: 3/9/2005-3/9/2027. ContinuingEdCourses.Net has been approved by NBCC as an Approved Continuing Education Provider, ACEP No. 6323. Programs that do not qualify for NBCC credit are clearly identified. ContinuingEdCourses.Net is solely responsible for all aspects of the programs.
ContinuingEdCourses.Net has been approved by NBCC as an Approved Continuing Education Provider, ACEP No. 6323. Programs that do not qualify for NBCC credit are clearly identified. ContinuingEdCourses.Net is solely responsible for all aspects of the programs. ContinuingEdCourses.Net is recognized by the New York State Education Department's State Board for Psychology (NYSED-PSY) as an approved provider of continuing education for licensed psychologists #PSY-0048.
ContinuingEdCourses.Net is recognized by the New York State Education Department's State Board for Psychology (NYSED-PSY) as an approved provider of continuing education for licensed psychologists #PSY-0048. Older adults
suffer from the same psychological problems as younger adults. While the proportion of mental health
problems is approximately the same for younger adults, older adults are more
vulnerable than younger adults to develop psychological problems resulting from
factors that impact the quality of life such as stress, ill health, loss,
decline in cognitive skills, and changes in living situations.
Older adults
suffer from the same psychological problems as younger adults. While the proportion of mental health
problems is approximately the same for younger adults, older adults are more
vulnerable than younger adults to develop psychological problems resulting from
factors that impact the quality of life such as stress, ill health, loss,
decline in cognitive skills, and changes in living situations. Findings from
the 2000 Medical Research Council Cognitive Function and Aging Study suggest that the relationship between “normal” brain aging and the dementias is
best represented by a continuum.
In the study, the brains of 209 older people (of which 100
met the clinical criteria for dementia) were examined to distinguish a normal
aging brain from that of one suffering from dementia.
Findings from
the 2000 Medical Research Council Cognitive Function and Aging Study suggest that the relationship between “normal” brain aging and the dementias is
best represented by a continuum.
In the study, the brains of 209 older people (of which 100
met the clinical criteria for dementia) were examined to distinguish a normal
aging brain from that of one suffering from dementia.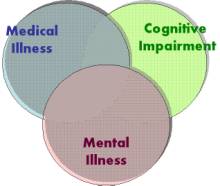 Older adults
present with a vast array of behavioral and psychological symptoms. An assessment of the older adult must
address the realms of mental symptoms, medical problems, and cognitive status
Older adults
present with a vast array of behavioral and psychological symptoms. An assessment of the older adult must
address the realms of mental symptoms, medical problems, and cognitive status