Learning Objectives
This is an intermediate to advanced level course. After
completing this course, mental health professionals will be able to:
- Discuss the history and prevalence of ADHD in adults.
- Describe how the symptoms of adult ADHD represent a disorder of executive functioning and self-regulation.
- List
the steps in the assessment of adult ADHD.
- Explain
the role of clinical judgment in the evaluation of ADHD in
adults.
- Summarize two evidence-based therapies for management of ADHD symptoms and
associated executive functioning deficits in adults.
- Discuss two categories of FDA-approved medications for use with adults with ADHD.
- Provide specific recommendations to assist the adult client with ADHD in achieving more effective functioning in major life activities such as work, school, home management, and managing finances.
The
materials in this course are based largely on and adapted from the following
books by Dr. Barkley: Attention Deficit Hyperactivity Disorder: A Handbook
for Diagnosis and Treatment (4th ed., 2015, New York: Guilford
Press), ADHD in Adults: What the Science Says (2008, Guilford Press), Taking Charge of Adult ADHD (2021, New York: Guilford Press), and When an Adult You Love Has ADHD: Professional Advice for Parents, Partners, and
Siblings (2016, Washington, DC: Lifetools, American Psychological
Association Press). But other sources were used as well, many of which
can be found in the Resources and References sections at the end
of this course.
The course contains the most accurate information available to
the author at the time of writing. The scientific literature on ADHD grows
daily, and new information may emerge that supersedes these course materials.
This
course will equip clinicians to advise adults with ADHD and their loved ones on
the most effective methods for managing the symptoms of ADHD and associated
impairments in adults with ADHD.
Outline
- Introduction
- Brief
History of ADHD in Adults
- Prevalence
of Adult ADHD
- What
is the Nature of ADHD?
- Diagnostic
Criteria and Adjustments for Adults
- ADHD
Involves Executive Functioning Deficits
- How Do We Know ADHD Is a Disorder of Executive Function?
- Is Neuropsychological Testing Useful for Diagnosing Adult ADHD?
- Diagnosing Adult ADHD
- The
Important Role of Clinical Judgment
- Impairments:
What Are the Consequences of Untreated ADHD?
- Major
Life Domains
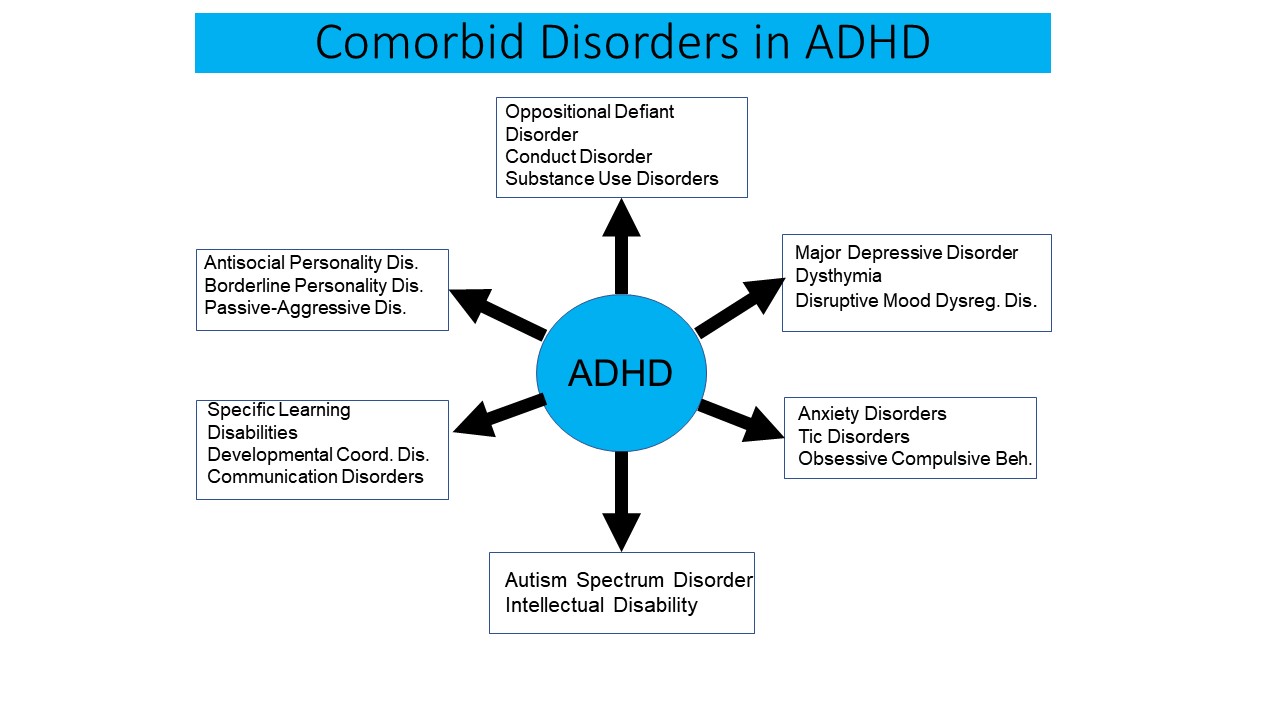
- Comorbid
Disorders
- Conclusion
to Impairments Linked to Adult ADHD
- Addressing
Reactions to the Diagnosis
- Helping
the Client Understand and Accept Their Diagnosis
- Acceptance
and Ownership Do Not Mean Making Excuses
- Becoming
Educated About Adult ADHD
- Evidence-Based
Therapies
- General
Counseling
- EF-Focused
Cognitive Behavioral Therapy (CBT)
- Coaching
- Medication
Management
- Other Issues in Using Medications for Adult ADHD
- Promising
but Under-Investigated Therapies
- Routine
Physical Exercise
- Marital/Couples
Counseling
- Vocational
Assessment and Counseling
- Technology
- Mindfulness
Meditation
- General
Strategies for Managing Adult ADHD
- ADHD
is a Disorder of Performance, Not of Knowledge
- Reject
Treatments that Don’t Address the “Point of Performance”
- Mental
Information Does Not Guide Behavior Very Well
- ADHD
Means Being Blind to Time
- ADHD
Reduces Internal or Self-Motivation
- Manage
the External Environment to Manage the Symptoms
- Rules
Alone Don’t Guide Behavior Very Well
- View
ADHD as the Diabetes of Psychiatry – A Chronic Disorder that Can Be Effectively
Managed
- Specific
Strategies for Assisting Adults with ADHD in Major Life Activities
- Work
and School Settings
- Managing
Health Risks
- Driving
- Substance
Abuse
- Conclusion
- Appendix
- Available FDA-approved Treatments for ADHD
- The Eight Stimulant Delivery Systems
- Resources
- References
Introduction
Despite
great strides in the identification, referral, diagnosis, and management of
adult ADHD over the past three decades (Faraone et al., 2024), much work remains to be done by mental
health professionals to further improve the delivery of mental health services
to most adults with ADHD. This course seeks to help ameliorate that situation
by briefly reviewing the nature, diagnosis, comorbidity, and impairments associated
with ADHD. It then provides both an overview of the evidence-based approaches
currently available for the management of adult ADHD as well as myriad specific
recommendations for the management of the various domains of impairment that
are a consequence of adult ADHD.
Beginning
in the 1990s, thanks to several large follow-up studies with adults, both the
general public and many mental health professionals became aware that ADHD was
not just a disorder of children but persisted into adulthood in at least 50%-65%
of all cases diagnosed in childhood. Moreover, evidence began to accumulate
that ADHD could be diagnosed in 3%-5% of the U.S. adult population. Many of
these cases had never been diagnosed as such in childhood even though they
likely had the condition. A major US population survey conducted in 2006
reported that 90% of those meeting diagnostic criteria for adult ADHD had never
been diagnosed with it or received any treatment for it. And just 25% were
receiving any treatment for any mental health condition. Yet the survey found
these adults to be suffering impairment in several major life activities. Now,
more than a decade later, the situation for adults with ADHD has and continues
to improve, although the majority are likely still not receiving appropriate
diagnostic and treatment services specifically for their ADHD. More mental
health professionals are now well aware that adults can have ADHD, and many are
seeking more information about its identification, diagnosis, and management. That
is the purpose of this course: to assist in providing up-to-date continuing
education training in how to recognize and treat ADHD in adults.
A Brief History of ADHD in Adults
The
history of ADHD is extensive for the childhood stage of the disorder. Far less
information exists concerning the history of ADHD in adults, largely because throughout
most of the past century ADHD was widely held to be a disorder strictly of
childhood. While popular interest in the possibility that adults can have Attention
Deficit Hyperactivity Disorder (ADHD) most likely originated with the
bestseller Driven to Distraction, published in 1994 by psychiatrists
Edward Hallowell and John Ratey, clinical and scientific papers acknowledging
the existence of an adult version of this disorder date back at least 50 years,
possibly even two centuries.
The
first paper in the medical literature on disorders of attention that described
a condition highly similar to ADHD is a short chapter in a German medical
textbook by Melchior Adam Weikard in 1775. Weikard described symptoms of
distractibility, poor persistence, impulsive actions, and inattention more
generally in both adults and children. The next reference to adult ADHD was in the
medical textbook by the Scottish physician, Dr. Alexander Crichton, in 1798. He
discussed two attention deficits, one of which is very similar to adult ADHD
while a second dealt with low levels of arousal, alertness, and energy that may
be similar to the increasingly studied second attention disorder known now as cognitive disengagement syndrome (previously called
sluggish cognitive tempo). Crichton espoused the view that inborn forms of
inattention would diminish with age in some though not all cases. Noteworthy as
well was that Crichton felt that problems with attention were associated with
many other mental and physical disorders, and that there are different
components involved in attention, making it multidimensional rather than
unitary, as modern researchers now also believe.
We must skip 104 years ahead to find the next reference to attention disorders in the medical literature. In his series of three published lectures to the Royal College of Physicians, George Still (1902) described 43 children in his clinical practice having serious problems with sustained attention and in the moral control of their behavior. By the latter symptom, Still meant the regulation of behavior relative to the moral good of all. He viewed the latter construct as a conscious comparative process in which one evaluates both the present and likely future consequences of one’s actions for both one’s self and for others prior to choosing a course of action. Most of his cases were not just inattentive and lacking in forethought but also were quite overactive. He proposed that the immediate gratification of the self was the “keynote” quality of these and other attributes of the children. In addition, among all of them, passion (or heightened emotionality) was the most commonly observed attribute and the most noteworthy. Still noted further that a reduced sensitivity to punishment characterized many of these cases, for they would be punished, evenly physically, yet engage in the same infraction within a matter of hours. Still believed that the major “defect in moral control” so typical of these cases was relatively chronic. While it could arise from an acquired brain defect secondary to an acute brain disease, and might remit on recovery from the disease, in most cases it was chronic.
Here
again we see reference to the possibility that ADHD may persist into adulthood,
thereby logically opening the door to the possibility that adults can possess
this same pattern of symptoms dating back to childhood.
The
first papers on research studies involving adults having actual ADHD seem to
date to the late 1960s. At that time, the disorder was known as Minimal Brain
Damage or Dysfunction (MBD) and its likely existence in adults was supported by
three sources. The first of these was the publication of several early
follow-up studies demonstrating the persistence of symptoms of
hyperactivity/MBD into adulthood in many cases. The second source was the
publication of research showing that the parents of hyperactive children were
likely to have been hyperactive themselves and to suffer in adulthood from
sociopathy, hysteria, and alcoholism, not to mention the usual symptoms of inattention,
lack of impulse control, and excess activity levels, all of which logically
implies that ADHD could exist in adults. The third source directly supporting
such a conclusion was the publication of studies on adult patient samples that
were believed to have hyperactivity or MBD. Noteworthy for our purposes here
was the finding that such adults had an early history of
hyperactive-impulsive-inattentive behavior dating back to childhood and that was
highly predictive of placement in an adult group characterized as impulsive-destructive,
again implying a persistent course of this behavioral pattern from childhood to
adulthood.
Adults
in the studies were typified by marked difficulties concentrating, being
emotionally labile, fearing their loss of impulse control, and showing marked
irritability as well as anxiety and self-depreciation. Problems with poor motor
skills and sluggish reaction or response timing were noteworthy. While EEG and
neurological exams were normal for gross findings of hard neurological signs,
all showed evidence of “soft” signs of “neuro-integrative disturbances” such as
motor clumsiness, poor balance, confused laterality, and poor coordination.
Psychological testing also revealed evidence of perceptual-motor problems and
motor incoordination and timing.
Especially noteworthy was the large clinical study by Anneliese Pontius (1973) of more than 100 adult cases of MBD. She noted that many demonstrated hyperactive and impulsive behavior and that their disorder likely arose from frontal lobe and caudate dysfunction. Such dysfunction would lead to their “inability to construct plans of action ahead of the act, to sketch out a goal of action, to keep it in mind for some time (as an overriding idea) and to follow it through in actions under the constructive guidance of such planning” (p. 286). Moreover, if adult MBD arises from dysfunction in the frontal-caudate network, it should also be associated with an inability “to reprogram an ongoing activity and to shift within principles of action whenever necessary” (p. 286). She went on to show that indeed, adults with MBD demonstrated such deficits indicative of dysfunction in this brain network, making this the first paper to argue that adult ADHD was likely a disorder of the brain’s executive function networks – a conclusion supported decades later by neuro-imaging and neuropsychological research.
By
the mid-1970s, researchers investigated the efficacy of stimulants with adults
having MBD using double-blind, placebo-controlled methods to assess response to
methylphenidate, pemoline (another stimulant), and the antidepressants
imipramine and amitriptyline. Paul Wender (1976) was likely the first to do such studies. About two thirds of cases showed a favorable
response to either the stimulants or antidepressants. Yet, it would not be
until the 1990s that both the lay public and the professional field of adult
psychiatry would begin to seriously recognize the adult equivalent of childhood
ADHD on a more widespread basis and to recommend stimulant or antidepressant
treatment in these cases.
By
the mid-1990s, Paul Wender set forth explicit criteria for the manner in which
the diagnosis of ADHD in adults should be made, recognizing that nether the diagnostic
criteria proposed for the syndrome of childhood hyperactivity in 1968 nor the
later Attention Deficit Disorder in 1980 were developmentally appropriate for
adult patients. Wender proposed an approach for diagnosis of ADHD in adults
(Wender, 1995) that was subsequently used in a number of research projects,
especially medication trials. Patients and an additional informant, preferably
a parent, were to be interviewed to assess retrospectively the childhood
diagnosis of ADHD. Evidence was also to be obtained for ongoing, continued
impairment from hyperactive and inattentive symptoms. Seven symptoms were
proposed to characterize the phenomenology of adult ADHD, namely, 1)
inattentiveness; 2) hyperactivity; 3) mood lability; 4) irritability and hot
temper; 5) impaired stress tolerance; 6) disorganization; and 7) impulsivity.
Known as the “Utah criteria,” these diagnostic guidelines required a
retrospective childhood diagnosis, ongoing difficulties with inattentiveness and hyperactivity, and at least two of the remaining five symptoms. A rating scale
was also constructed to aid in the retrospective diagnosis of childhood ADHD. The
Utah criteria have declined in use among investigators and clinicians in favor
of using DSM-5-TR criteria that have been adjusted for use with adults.
A
further watershed moment in the history of adults with ADHD was the development
and FDA approval of the first medication for adult ADHD, the non-stimulant atomoxetine
(Strattera®), by the Eli Lilly & Company. It was investigated in thousands
of adults with ADHD in several randomized, placebo-controlled trials and found
to be useful for its management. Later, stimulants (methylphenidate, mixed
amphetamine salts) would eventually be studied more thoroughly for use with adults
with ADHD and receive similar FDA approval for such. New delivery systems have
also been subsequently developed that permit greater sustained therapeutic
action across the day than did immediate release preparations. These include
osmotic pumps (Concerta®), variable timed-release pellets (Focalin XR®, Metadate
CD®, Ritalin LA®, Adderall XR®, et al.), and skin patches (Daytrana®), besides
the earlier-available but clinically disappointing wax-matrix sustained release
formulation of methylphenidate (Ritalin SR®).
More
recently, a new non-abusable formulation of a mixed amphetamine compound (Vyvanse®)
received FDA approval for use with ADHD. In this delivery system, the pills must be dissolved and then absorbed through the gut before the amphetamine compound can be activated and available for therapeutic blood levels to become available and thus manage adult ADHD symptoms. By late 2018, yet another delivery system was FDA-approved, this one being a delayed onset version of methylphenidate that can be taken at night and that reliably activates the next morning, about nine hours after ingestion (brand name awaiting assignment). The company may have plans to use the same delivery system for an amphetamine-based delayed onset medication in the future.
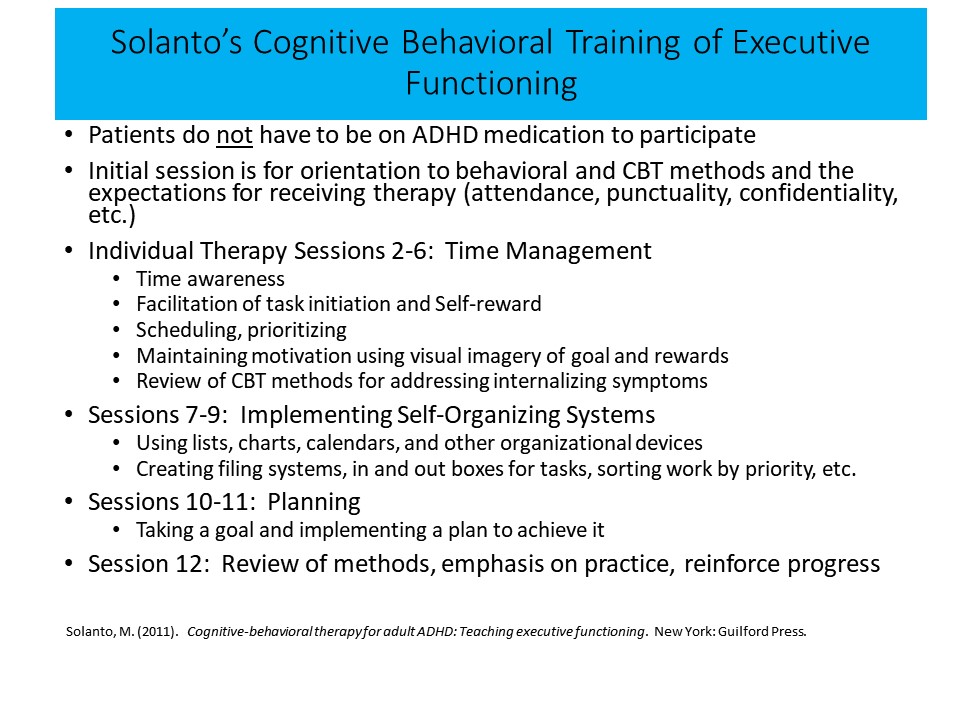
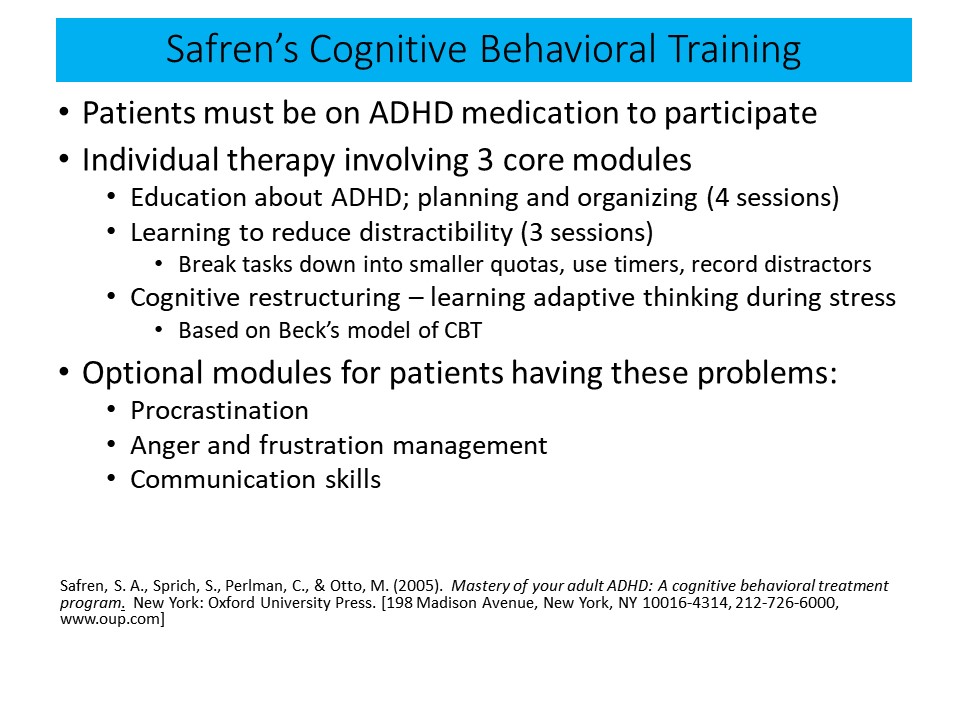
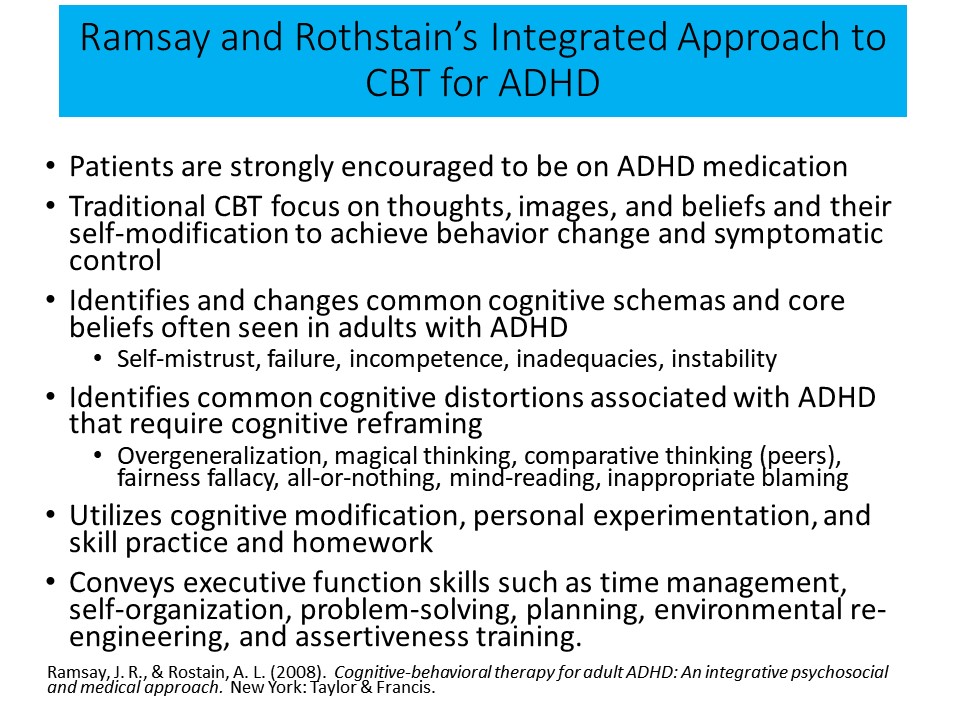
Psychological
treatments for adults with ADHD, though numerous in clinical practice, have to
date not received as much serious scientific scrutiny as medications. This
remains a glaring deficiency in the clinical scientific literature on the
disorder in adults, though it is improving of late. Cognitive behavioral
therapies focusing specifically on adult ADHD symptoms and associated deficits in executive function (EF) have been developed by
Safren and colleagues, then of the Harvard Medical School, independently by
Ramsay and Rothstein at the University of Pennsylvania Medical School, and most recently by Solanto and colleagues now at Montefiore Medical Center in Long Island, NY. All focus to varying degrees on the executive function deficits associated with ADHD
Prevalence of Adult ADHD
It
appears from both childhood follow-up studies and, more directly, from studies
of adult general population samples, that the prevalence of ADHD in adults in
the United States is approximately 5%. Based on this figure and the 5%
estimated prevalence for ADHD in adults, it seems likely that at least 14
million adults in the US probably have ADHD. This is a sizeable number, making
it imperative that the mental health, medical, and educational professions, as
well as employers, become more aware of the existence of this disorder and its
treatments.
It
also makes it essential that we understand as much about the expression of this
disorder in adulthood – along with its comorbid psychiatric disorders and
impairments in major life activities – if we are to be able to better
understand the disorder and to be able to manage it and its consequences more
effectively.
What is the Nature of ADHD?
ADHD
is recognized in the Diagnostic and Statistical Manual of Mental Disorders
(5th edition, or DSM-5-TR, 2022) as a neurodevelopmental
condition that consists of developmental delays or deficiencies in at least two
significantly related domains of neuropsychological abilities. These two
dimensions are referred to as inattention and hyperactive-impulsive symptoms (Faraone et al., 2024).
Readers
should understand that despite the criticisms and limitations I will level at
these criteria, at least as they pertain to the diagnosis of adults, they are
the most empirically-based, rigorously tested, and logically coherent criteria
of their time for the diagnosis of ADHD, especially in children.
The Symptoms of ADHD
The DSM-IV criteria specified a set of 18 symptoms divided into two lists; inattention and hyperactivity-impulsivity, on which were nine symptoms each. These symptoms have to occur often or frequently and been present for at least six months. In the subsequent DSM-5-TR published in 2022, the same 18 symptoms continued to be employed but they have been given clarifications in parentheses for use with adolescents and adults. The age of onset has now been adjusted upward to age 12 given that the earlier age seven had no scientific validity to it. By increasing the age of onset of the disorder, it was hoped that more adults who otherwise meet all other criteria for the disorder except the age of onset of seven years old will now be eligible for the diagnosis; a good thing. The threshold for the diagnosis remained at six symptoms on either list for children and is reduced to five for adults. This too is an improvement, although most studies on this issue would suggest that four symptoms would be even better.
A further improvement is the explicit recommendation that symptoms reported by patients be corroborated through someone who knows the patient well. Also beneficial has been the removal of the subtyping scheme such that ADHD is now viewed as a single disorder in the population, which behavioral genetic studies of large populations clearly suggest. Clinicians can now specify which symptoms are more evident in the clinical presentation at the time of assessment, such as Predominantly Inattentive Presentation. Still, some problems remain with the DSM criteria that were not addressed in DSM-5-TR. But that is not to imply any stability for that presentation or qualitative differences from the other presentations, as cases can move from one to the other presentation over time and development.
Diagnostic Criteria and Adjustments for Adults
There is little evidence to suggest that ADHD symptoms currently identified in the DSM-5-TR, designed as they were for use with children, best characterize adults with ADHD. My colleague, Kevin Murphy, and I (and others) identified nine symptoms that were the most useful for identifying adults with ADHD, six of which were not in the DSM-5-TR but came from our evaluation of executive functioning in daily life using my rating scale of that domain. The proposed criteria are:
Has four of the first seven, or six of all
nine of the following symptoms that have persisted for at least six months to a
degree that is maladaptive and inconsistent with the subject’s developmental
level:
- Often easily distracted by
extraneous stimuli
- Often makes decisions impulsively
- Often has difficulty stopping
activities or behavior when they should do so
- Often starts a project or task
without reading or listening to directions carefully
- Often shows poor follow-through on
promises or commitments they have made to others
- Often has trouble doing things in
their proper order or sequence
- Often more likely to drive a motor
vehicle much faster than others (excessive speeding) (If person has no driving
history, substitute: “Often has difficulty engaging in leisure activities or having
fun quietly.”)
- Often has difficulty sustaining
attention in tasks or leisure activities
- Often has difficulty organizing
tasks and activities
Some of the above symptoms that cause
impairment were present before age 18. Some impairment from these symptoms
is present in two or more settings (e.g., work, educational activities, home
life, social functioning, community activities, etc.). And there must be clear
evidence of clinically significant impairment in social, academic, domestic
(cohabiting, financial, child-rearing, etc.), community, or occupational
functioning.
Another
problem with DSM-5-TR is that the greatest weight is given to inattention (nine
symptoms), followed by hyperactivity (six symptoms), with the remaining three
symptoms thought to reflect impulsiveness. Most of those impulsive items
reflect principally verbal behavior. The words “impulsive” or “poorly
inhibited” are not even mentioned in the symptom list despite being viewed
currently as a core feature, if not THE core feature of this disorder. This has
proven to be a glaring oversight because the symptom of “makes decisions
impulsively” and others related to it (acts before thinking, has difficulty
waiting for things, etc.) are among the most discerning symptoms for
distinguishing ADHD from other psychiatric disorders as well as from the
general non-disordered population. While DSM-5-TR tested additional symptoms of impulsivity,
it was elected not to include them, perhaps due to concerns that it would
increase the prevalence of the disorder.
In order to make the original DSM-IV symptoms more specific to adults, given that they were developed originally just for children, the DSM committee added clarifications to many items in parentheses. Our research on these clarifications, however, shows that they are only weakly related to the original symptom they are supposed to clarify and behave more like new or additional symptoms of ADHD. A few may be as or more related to anxiety as they are to adult ADHD. It is therefore possible that in using these clarifications, one is actually using a list of symptoms far larger than the original 18 items, thus making the cutoff score of five symptoms on each list questionable as the cutoff point for determining presence of disorder. Not doing so could lead to diagnosing a larger percentage of adults with this disorder than would be the case with the earlier DSM-IV criteria. In short, one cannot add more symptoms to the list and not adjust the cutoff score accordingly. For these reasons, I recommend ignoring the clarifications in parentheses and just using the original DSM item wording when evaluating adults until more research can clarify the validity of these item clarifications.
Also
problematic in DSM-5-TR is the requirement for the age of onset of symptoms to be by
age 12. Unlike the assessment of children, the clinical evaluation of adults is
highly dependent on patient self-reporting. However, adults have a limited
recall of the exact time course and nature of symptoms within the developmental
time frame associated with so precise a childhood onset and have a limited
recall of the domains of childhood impairments related to those symptoms.
Moreover, many adults who present for clinical care are unable to provide independent
evidence of the disorder, either through retrospective parental report or
records of academic functioning. Adults do not typically come to clinical
evaluations with their parents in order to provide the customary evidence for
judging symptom onset as is done in children.
Add
to this the likelihood that ADHD may create a positive illusory bias in adults
concerning their possible impairment – as it does in children with ADHD – that
could possibly diminish self-awareness of symptoms and impairments. This gives
a further reason to question the reliance upon adult patients for establishing
the age of onset of their symptoms and associated impairments. I argue that the
criterion should be abandoned or redefined to include the broader period of
adolescence to young adulthood (ages 18 to 24). No evidence is available in the literature to our
knowledge that suggests that onset of ADHD symptoms at or after age 12 results
in a qualitatively or even quantitatively different disorder than cases of ADHD
having the earlier recommended symptom onset (Vater et al., 2024). And my own research showed that
ages 12-18 would have been even more sensitive to and inclusive of those with an otherwise legitimate disorder.
A
further limitation of the DSM-5-TR for use with adults is that it requires that
some impairment from the symptoms is present in two or more settings (e.g., at
school or work and at home). Problematic here, obviously, is that adults are
involved in far more numerous and important adaptive settings or domains of
major life activities than this criterion stipulates. Not only are the settings
specified here too global to be of much good to the clinician evaluating
domains of impairment (e.g., “home”), but they ignore many more domains of
major life activities that are not only more specific but also comprise
important domains of adult adaptive functioning. General functioning within the
larger organized community (e.g., participation in government or formally
organized community groups, cooperation with others living in the same
neighborhood, abiding by laws, driving), financial management (e.g., banking,
credit, contracts, debt repayment), parenting and child-rearing (e.g.,
protection, sustenance, financial and social support, appropriate education,
discipline), marital functioning, and routine health maintenance activities are
additional domains of major life activities in which symptoms may produce
impairment that would not be evident in children. Current criteria fail to
reflect these potential areas of impairment.
A
further difficulty with DSM-5-TR is that controversy exists over the definition of
impairment due to an enormous increase in requests for special accommodations
in employment and high-stakes academic testing under the Americans with
Disabilities Act (ADA). Further specification of the meaning of impairment in
DSM-5-TR is necessary so as to avoid misunderstandings among clinicians and public
agencies. Some clinicians assess impairment based on comparison of deficits
relative to a person’s intellectual level, much as had been done in the earlier
history of defining learning disabilities as being significant discrepancies
between IQ and some specific area of academic achievement, such as reading.
Others believe impairment is based on how well an individual functions relative
to their specialized peer group, particularly if they are unusually intelligent
or well-educated, such as fellow gifted individuals or peers in medical or law
school.
Still
others have argued that impairment should mean serious dysfunction in the performance
of major life activities (e.g., family, marital, social, or occupational
functioning) that are required of society in general. More to the point, this
view holds that impairment should be defined as being relative to the norm or
average person, as required by the ADA, and not relative to some narrow, highly
specialized and accomplished subset of adults or to an estimate of one’s
general cognitive ability, such as IQ. I prefer the latter view of defining
impairment because of a number of factors: its consistency with scientific
views on valid mental disorders (harmful dysfunctions that are failures or
severe deficiencies in mental adaptations as noted by Jerome Wakefield [1992]);
its consistency with the ADA, with associated court rulings, and with the
legislative intent behind the ADA (granting protections and accommodations to people
functioning well below normal or average); and simple fairness or justice –
individuals should not be viewed as disordered and granted special protections,
accommodations, disability financial benefits, or other societal privileges
when they are not below the average of the population at large. It is
inherently unfair to grant advantages to those who are not actually subnormal.
Also, this latter view of impairment respects the fact that one’s intelligence
is not an indicator of functioning in all avenues of adult life nor are
disparities between IQ and some other measure of adaptive functioning. The
DSM-5-TR should have made the criteria for impairment clearer as to the domains it
encompasses and the comparison group to be used for its determination.
Despite
these continuing problems with the DSM-5-TR criteria for adults with ADHD, the
changes that were made to DSM-IV are an improvement and make DSM-5-TR more
sensitive to the detection of the disorder in adults than its predecessor DSMs.
Even so, readers need to be alert to these limitations as they go about
applying DSM-5-TR criteria to the diagnosis of ADHD in adults.
Other
points to keep in mind in using DSM-5-TR are as follows:
- As we will see shortly, there are far more cognitive deficits linked to ADHD
hiding behind these two dimensions than their names imply. The disorder is
classified as neuro-developmental because the scientific evidence for
the substantial role of neurological and genetic causes in ADHD is now
overwhelming and irrefutable. ADHD is considered to be neuro-developmental because
it is primarily the result of a delay or lag in specific mental abilities and
it arises during the developmental course of the individual, most often before
16-18 years of age. Those deficits are largely due to delays and/or
dysfunctioning in the maturation of the brain areas that underlie EF.
- Such brain maldevelopment seems to arise largely from genetics, but can also
occur as a consequence of damage or other disruptive influences experienced by
the person at any time during development, most often during prenatal brain
formation (Faraone et al., 2024). Thus, ADHD can arise de novo in an adult as a consequence of
brain injuries even after development is completed, such as may occur secondary
to repeated closed head trauma, tumor, stroke, or other adverse events that
impact the functioning of brain regions and circuits known to support EF and
self-regulation (largely the prefrontal lobes and networks).
- ADHD presents largely the same in both sexes, despite popular opinions to the contrary (Babinski, 2024; Babinski & Libsack, 2025). That said, females were grossly underdiagnosed in earlier decades for various reasons and so the rise in diagnoses in females of late is positive news. And while the symptoms may be largely the same between males and females, there are significant differences in the nature of the comorbid disorders that link up with ADHD in each sex as well as differences in the domains of impairment likely to be affected. Moreover, symptoms in females may fluctuate far more dramatically across the month and likely the lifespan as a result of changes in the sex hormones in females (Ang et al., 2024; see also, Harper & Lewis, 2025).
The symptoms of ADHD are dimensional in that they reflect the extreme end of a
continuum (most likely a bell-shaped distribution) of normal or typical human
ability in these two areas. Therefore, adults with ADHD have a disorder that:
- is
beyond their own choice or making;
- is
intrinsic to their psychological and physical nature;
- is
not a categorical condition, such as being pregnant, but is dimensional;
- differs
primarily from the behavior and abilities of others in these dimensions as a
matter of degree (quantitative), not of kind (qualitative);
- will
most likely become evident sometime during childhood development (probably
before age 16 in 98% of cases);
- is
likely to be pervasive across many but not necessarily all situations;
- is
likely to be persistent over time for many but not necessarily all cases; and
- leads
to impairment in one or more major domains of life activities.
In summary, it is important to understand the nature of adult ADHD and its need for treatment. For one reason, as noted above, a substantial percentage of adults in the U.S. have ADHD (one in every 20-25). For another, they will be increasingly presenting to outpatient clinical services for diagnosis and management of their disorder as public awareness of adult ADHD continues to increase. Moreover, they are likely to be suffering impairments in many domains of major life activities (see Consequences of Untreated ADHD, below) given the important role of EF in adult daily life.
Without identification and treatment, ADHD in adults will contribute to their experiencing increased harm or suffering to themselves as well as to society and may likely underlie the reason they are not benefiting much if at all from treatments aimed at the other disorders that may coexist with adult ADHD (substance use, marital problems, occupational difficulties, driving impairments, weight control and health maintenance, etc.). Unmanaged adult ADHD may also be costing society billions of dollars annually as a consequence of these unaddressed or under-addressed impairments and comorbidities.
For these reasons, this course will provide readers with information on the outcomes of unmanaged ADHD in adults as well as review the treatment options that can help to reduce or eliminate these impairments.
ADHD Involves Executive Functioning Deficits
Many clinical researchers, myself included, conceptualize ADHD and its symptoms as involving deficits in the following mental abilities, often referred to as executive functions (see Dr. Barkley’s course on this website on Executive Functioning (EF), Executive Functioning: Critical Issues for Understanding and Managing Deficits).
Self-regulation (SR) relies on executive function and its underlying brain networks. Therefore, ADHD could also be called EFDD (executive functioning deficit disorder). The reason I prefer the term SRDD (self-regulation deficit disorder) is that it is the obvious and repeated failure to demonstrate self-regulation that is so apparent to those with ADHD, their families, and clinicians who are trying to evaluate and manage it.
Goal-directed
persistence and resistance to distraction (inattention)
What
separates the attention problems seen in ADHD from those evident in other
disorders such as depression is that those with ADHD have problems with
sustaining attention to and persisting toward a goal, either self-imposed or
assigned by others – in short, they suffer in their attention to the future.
They are less able to persist at getting things done over time, in time, and on
time that involve delayed or future events. Thus, they pay attention to what is
happening now just fine but not to what they need to be doing to be ready for
what is coming next or what they have been assigned to do. Even if they try to
persist toward tasks or goals, they are more likely than others to react to
distractions, which are events that are not relevant to the goal or task. Those
distracting events are not just irrelevant things occurring around them, but
also irrelevant ideas occurring in their mind. The problem here is not one of
detecting those distractors as well as others do, but in failing to inhibit
reacting to those distractors as well as others.
The EF-SR theory can further enlighten us as to the nature of the inattention occurring in ADHD; this is incredibly illuminating for clinically understanding ADHD but also for its differential diagnosis from other mental disorders that adversely affect attention, but in entirely different ways. Consider that attention represents a relationship between a stimulus and the perceptual-motor response of the individual who orients to it, explores it, and then may stay engaged with it. Attention therefore represents a form of stimulus control. But just what kinds of stimuli or events are failing to control or elicit such engagement from people with ADHD compared to other types of such stimuli or events?
Those with ADHD have little trouble paying attention to the now – the momentary present and external environment; in fact, that's the problem. What is going on immediately in front of them in that moment has a much stronger pull on engagement of their responses than do the private, mental representations about the tasks they have been asked to do or the future they plan for them and the behavioral sequences or schemas needed to make that future happen. Those mental representations are held in the two working memory systems – visual and verbal. Thus, what people with ADHD are inattentive to are those mental representations – about tasks, goals, time, and delayed consequences and the future in general – which are thus far less able to capture or control the actions of the individual with ADHD. Such representations are simply not compelling enough to govern their immediate behavior relative to the events playing out around them.
Reframing the inattention of those with ADHD in this way can vastly improve differential diagnosis, helping us distinguish between the inattention seen in ADHD and that seen in many other psychiatric and neurodevelopmental disorders. Disorders such as depression, anxiety, or even autism spectrum disorder can also result in a type of inattention. But people with these disorders are inattentive to events or stimuli in the now – just the opposite of ADHD. That type of inattention is now called Cognitive Disengagement Syndrome (see Becker, et al., 2022). In that case, mental representations (thoughts) about their problems, worries, fears, or just their daydreams or mind wandering (as in autism) are all too powerful in capturing and sustaining the engagement of the individual, decoupling the attention of the person from the external world and shifting it to a focus on mental events. People with these other disorders are mentally preoccupied instead of engaged with the ongoing flow of the now and the things on which they should be working. You can see this in the mental rumination of depression, in memory re-experiencing as in anxiety or PTSD, in self-absorption over possible adverse consequences that might happen to them, improbable as they are likely to be, and certainly in the obsessions of someone with OCD. Likewise, people suffering from the new attention disorder of sluggish cognitive tempo may be preoccupied simply with mental daydreaming or mind wandering to the point that it is maladaptive or pathological.
In sum, where people with ADHD are decoupled from being governed by thoughts and plans related to tasks and goals (the future), and thus overly attentive to the external now, those having other disorders are decoupled from events in the external world and overly attentive to mental events or thoughts.
Working
memory
A
large part of the adult’s inattentiveness in ADHD comes from the inability to
hold in mind what goal they have chosen or been assigned, what steps are involved,
the most efficient sequence for attaining that goal, and monitoring when it has
been accomplished. This reflects a deficiency in working memory, which is remembering
what to do. Memory for facts, knowledge, or information is not so much the
problem as is remembering what is to be done and persisting at it until it is
completed. Even if they try to hold in mind information that is to guide their
behavior toward a goal or task, such as instructions or assignments clinicians
give them, any distractions occurring around the adult with ADHD will disrupt
and degrade this special type of memory. The mental chalkboard of working
memory is wiped clean by the distraction and so the affected adult is now off
doing something other than what they are supposed to be doing. And having
reacted to a distraction, and so gone “off-task,” the adult with ADHD is far
less likely to re-engage the original and now-uncompleted goal or task. In sum,
the adult with ADHD is less likely than others to remember what they were
supposed to be doing. Yes, adults with ADHD are forgetful. But it is a special
type of forgetfulness – it is forgetting what they are supposed to be doing
(forgetting the goal, specifically, and the future more generally).
Inhibition
Adults
with ADHD are not just impulsive (poorly inhibited) in their actions, which
leads them to move around, touch things, and otherwise behave too much (the “Hyperactivity”).
Their deficit in inhibition extends to their verbal behavior (talking excessively)
and to their cognitive activities or thinking (impulsive decision-making). It
also interferes with their self-motivation, meaning that they are more likely
to opt for immediate rewards or gratification than others do. Put another way,
they have a high time-preference and so steeply discount the value of a future
or delayed event or consequence (reward or punishment) more than others do –
they prefer to have small results now rather than larger results later.
Finally, their impulsiveness is evident in their emotions. They display their
emotional reactions more quickly and more often than do others of their age.
And, if strong emotions have been provoked by some event, they will have a far
more difficult time moderating or otherwise self-regulating that emotion. So
adults with ADHD are less patient, more easily frustrated, quicker to become
emotionally aroused, more excitable, sometimes sillier, yet also more likely to
react with anger. And so the adult with ADHD is more likely to respond with
aggression when provoked. They show emotions that are less mature and
appropriate to the situation and less consistent with or supportive of their
future welfare than others do.
Planning
and Problem Solving
ADHD
is associated with difficulties in generating multiple possible options for
overcoming obstacles encountered when pursuing goals, or in contemplating
multiple solutions posed by problems. A related deficit is in the ability to
construct and execute the steps of a plan necessary to attain a goal. This
difficulty is often evident in school or work settings in problems with mental
arithmetic, providing verbal narratives to questions posed by others, and in
rendering oral reports, written reports, and other tasks in which a complex,
well-organized response is necessary.
A
recurring theme here is that ADHD interferes with thoughts, actions, words,
motivations, and emotions aimed at organizing behavior across time and
preparing for the future instead of just reacting to the moment. To act
impulsively, fail to persist, and be distractible is to be nearsighted toward
the future – to be preoccupied by moments and so be blind to time. The
aforementioned cognitive deficits will then disrupt the adult’s EF in daily
life activities, as will be evident in problems with:
- Self-Awareness – less able to
monitor their own activities, report accurately on their own behavior and
performance, and describe their inner states and outward behavior as reliably
or accurately as others.
- Self-Restraint – deficient
behavioral inhibition, limited self-control, poor delay of gratification, and
difficulties subordinating one’s immediate interests and desires to those of
others.
- Self-Management
to Time – poor time management and organization across time to achieve one’s goals or
accomplish assigned tasks.
- Self-Motivation – an inability to
activate and sustain motivation to continue relatively boring, tedious,
effortful, or lengthy tasks in which there is no intrinsic interest or
immediate payoff.
- Self-Organization
and Problem-Solving – difficulty with organizing one’s personal space,
desk, locker, academic materials, etc. so as to accomplish work efficiently and
effectively. Forgetfulness of what is to be done or what was assigned. Also,
deficits evident in tasks that require working memory and thoughtful problem-solving,
as noted above.
- Self-Regulation
of Emotions – difficulty with inhibiting the expression of impulsive emotions in reaction
to emotionally provocative events. This is evident in being easily excitable,
prone to both positive and negative emotional outbursts, and
greater-than-typical impatience, frustration, anger, hostility, and reactive
aggression.
How Do We Know ADHD Is a Disorder of Executive Function?
As the great neuroscientist Joaquin Fuster so eloquently argued in his 1997 book on the prefrontal lobes, the quintessential function of that brain region is the formation of goals and the cross-temporal construction, organization, and maintenance of behavior needed to attain desired goals, or what constitutes a hypothetical future. In other words, the role of executive function is to allow us to behave in ways that serve the future we want. So, if what we see in ADHD at a much deeper level than inattention, hyperactivity, and impulsivity is a deficit in self-regulation, it must be rooted in problems with these executive functions. And, in fact, neuroanatomy tells us that is so.
The Neuroanatomy of ADHD
The areas of the brain most reliably associated with ADHD are the prefrontal cortex, the anterior cingulate, the basal ganglia (especially the striatum), the cerebellum (especially the central vermis), and the amygdala (not always reliably implicated). Research demonstrates that these regions are functionally interconnected to form one of the seven major brain networks – the executive system. In my view, that system underlies the human capacity for self-regulation and, as Fuster concluded, for the cross-temporal organization of behavior toward goals (future-oriented action). There are at least four subnetworks in the executive network, each of them associated with different parts of the brain, that can help us understand how executive functions help us self-regulate – or, in the case of ADHD, make it difficult to do so:
- The Inhibitory Executive Network: Think of this subnetwork as allowing us to resist responding to goal-irrelevant events, or distraction. It's responsible for the voluntary inhibition of ongoing behavior and emotions, as well as the suppression of competing responses to goal-irrelevant events, both internal and external.
- The "What" or Cold Executive Network: Essentially, this network allows what we think about (mainly imagery and self-talk) to guide what we do. It also permits the higher-level function of the manipulation of goal-related mental representations (analysis and synthesis, or mental play) so as to support planning and problem solving.
- The "When" (Timing) Executive Network: When we choose to act can be as or more critical to the success of a plan than what we had planned to do, and it's this subnetwork that gives us a subjective sense of time and the temporal sequencing of thought and action as well as the timeliness in executing such actions.
- The Hot (Emotional) or "Why" Executive Network: This is probably the subnetwork that makes the final decisions about goal choices and the selection of planned actions to attain them. But it also permits the top-down regulation of emotion in the service of those goals and our longer-term welfare, probably through the use of self-imagery and self-talk, or the working memory network above.
You may be wondering where hyperactivity fits into the executive function neuroanatomy picture of ADHD. In part, it certainly arises from defective functioning of the inhibitory network. But in addition to the subnetworks listed in the sidebar is the motor activity regulation network. Disturbances in this network are thought to also give rise to the hyperactive symptoms of the disorder.
If what you are seeing in a patient includes problems with goal-directed attention and volitional inhibition, resistance to distraction, working memory (forgetfulness in daily activities), sense of time and timing, time management, planning and problem-solving, self-organization, emotional self-regulation, self-motivation, and self-awareness – essentially the major executive functions – and not just the traditional DSM-5-TR ADHD symptoms, then a patient may well qualify for a diagnosis of ADHD and certainly has executive function deficits underlying them. When you see this in patient after patient, with ADHD it is easy to come to see that, logically, ADHD must be EFDD at its root.
What does this mean clinically? It means that:
- ADHD comprises a far broader array of cognitive and behavioral deficiencies than is reflected in the current clinical view as set forth in the DSM-5-TR. To call this merely an attention disorder is both to trivialize the condition and to be clinically unproductive.
- You need to listen for the deficits in the various executive functions as you interview patients about these executive function domains, going beyond a mere exploration of just the DSM-5-TR ADHD symptoms.
- It is this broader array of executive function deficits that accounts for the range of impairments that people with ADHD experience across most domains of major life activities.
- These executive function deficits are the things that will require accommodations and other treatments well beyond what might be suggested from the traditional ADHD symptom dimensions.
Because the executive function subnetworks functionally interconnect – that is, they interact in varying ways from patient to patient – ADHD will be heterogeneous across cases. Don't expect symptomatic presentations to be identical or even highly similar. When you know that some networks may be more (or less) adversely affected by the various etiologies of ADHD than others, you know that close scrutiny will be required by the astute diagnostician to appreciate the diversity of clinical symptoms patients may demonstrate.
The
vast majority of adults meeting diagnostic criteria for ADHD fall in the bottom
7% of the population in each of these major areas of EF in daily life. It is
easy to see how such deficits would produce a myriad of difficulties with
functioning in various major life activities that typically place a premium on
these EF abilities. Those are the areas of daily functioning that adults with
ADHD are most likely to describe as problematic for them. So clinicians should
be listening carefully for complaints that fall into these areas when they
initially evaluate an adult with ADHD or are working with them initially in a
counseling or coaching circumstance.
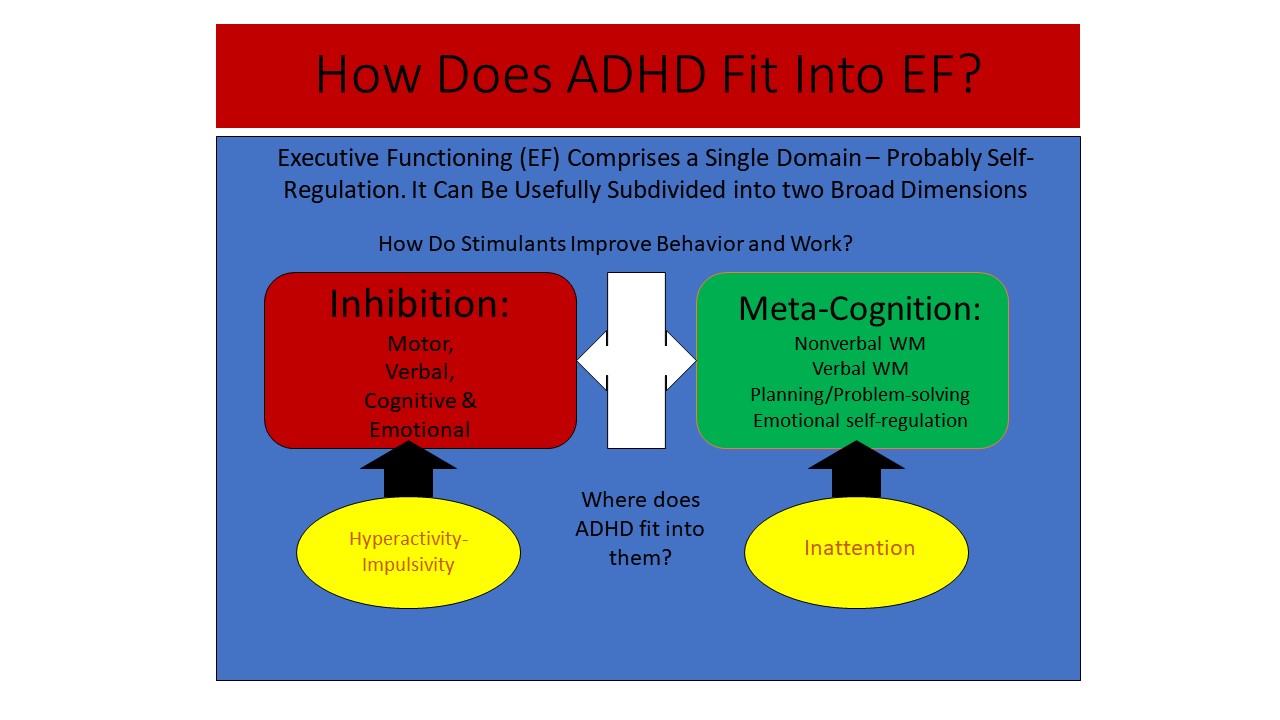
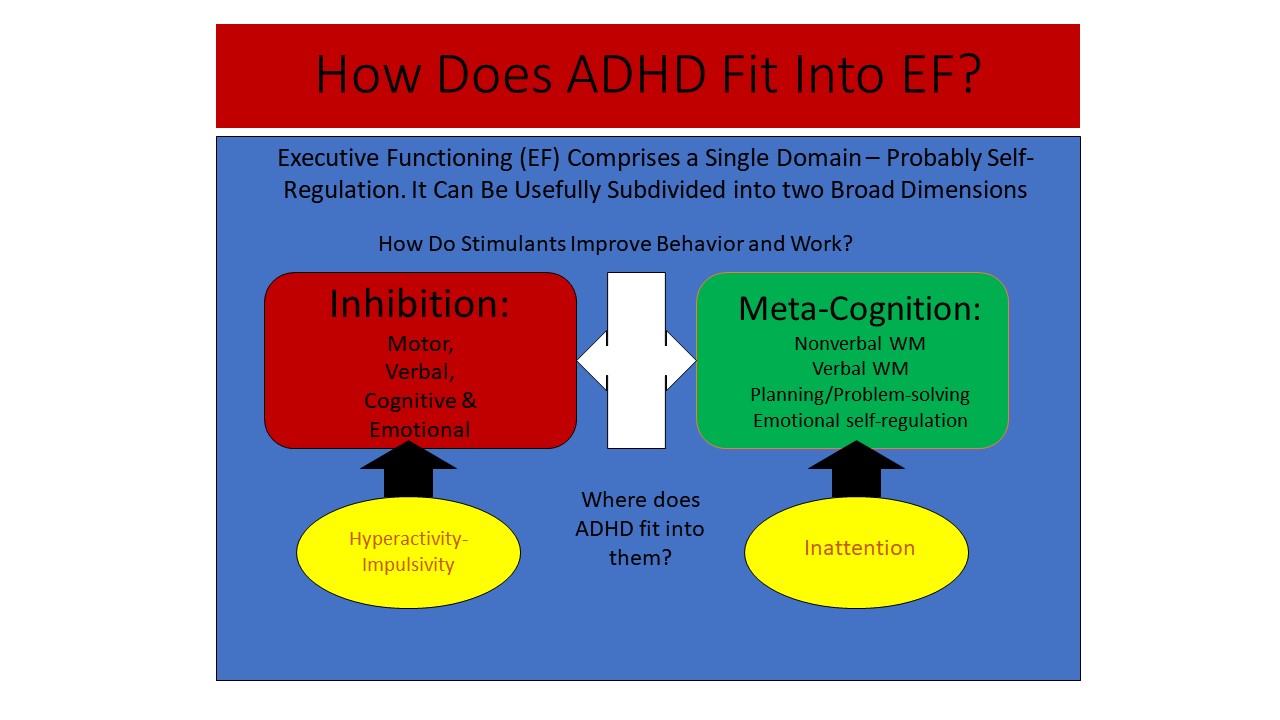
The DSM Criteria Within the EF-SR Theory
The Figure below shows that executive function comprises one primary construct. All research on executive function measures reveals such a single major construct, which I view as self-regulation. That broad domain of executive function can be divided into two: inhibition and metacognition, which, as shown in the figure, can be further dissected into smaller dimensions of executive functions that are partially coupled to each other. The lower half of the figure shows that the two traditional symptom dimensions of ADHD (inattention and hyperactive-impulsive behavior) are simply subsets of the two main dimensions of executive function. This means executive function is both one thing (self-regulation) and many things (it can be subdivided into narrow-band executive functions related to broader bands of inhibition and metacognition).
Is Neuropsychological Testing Useful for Diagnosing Adult ADHD?
Given the role of EF in ADHD, it would seem that EF tests ought to be useful in diagnosing adult ADHD. But they are not. Some of my scientific colleagues argue that ADHD is not a disorder of executive functioning, citing the fact that only a minority of people with ADHD fail their executive function tests and test batteries. Unfortunately, this argument does not explain the serious and pervasive deficits in executive function, self-regulation, and the cross-temporal organization of behavior so evident in daily life in those with ADHD, as shown by self- and other ratings and in clinical interviews. Telling, here, is the substantial body of evidence showing that ratings and observations of executive functioning in daily life are not significantly correlated with the results from those executive function test batteries. So clearly, whatever executive function tests may be measuring, it is not executive functioning in daily life. Critics of the EF-SR Theory of ADHD see this as just more evidence against rating scales; they see the tests as being the gold standard for assessing executive function.
Some also assert the false criticism that such ratings are subjective and so are limited in what they can tell us about executive functioning. I and others see this lack of a correlation between tests and ratings as evidence against the ecological validity of the tests – they are not the gold standard for measuring executive function. Moreover, these tests are poor at predicting impairment in major life activities known to be rife with executive function and self-regulation. Multiple studies using rating scales of executive functioning in daily life clearly attest to the fact that a vast majority of patients with ADHD are impaired in the major executive function domains: time management, self-organization and problem-solving, self-restraint, self-motivation, and the self-regulation of emotions.
A further criticism of the use of psychometric and other tests for evaluating ADHD is that they have given rise to theories about the nature of ADHD that predict nothing of clinically useful consequence outside of their own test results or those tests with highly similar formats. So, the wise clinician is likely to respond to such theories as delay aversion, a limited cognitive energy pool, etc., with "So what?" What exactly does it mean in real life to display, for example, delay aversion on a lab task of that construct other than intolerance of delays on tests? What does it predict about the individuals' life outside the lab and how they are functioning in various important domains? What does it tell us about other risks they are likely to experience given that testing deficit? Does it inform us as to the occupations they should consider or avoid, or the accommodations in work or educational settings they should request?
In sum, what does it say about how to help those patients in relevant and important natural settings where impairments exist? And does it inform us on what other treatments may need to be done to address this core problem, such as with aversion to delay? The answer to them all is a resounding “No.” In other words, you cannot take such deficient test performances to “the clinical bank” because they have no practical cash value, so to speak, for guiding us in helping clients.
The lab tasks are bereft of clinical meaning for providing assistance with differential diagnosis or patient care.
Diagnosing Adult ADHD
In
order to capture all of the relevant information needed to adhere to the DSM-5-TR
diagnostic criteria for adult ADHD as well as to the modifications to it
discussed here, the assessment of a client for adult ADHD should incorporate
the following procedures: an open-ended general interview; a structured
interview of relevant DSM-5-TR disorders; rating scales of adult ADHD symptoms,
executive functioning, and functional impairment; a review of archival records:
corroboration of symptoms through someone who knows the patient well: psychological
screening tests for IQ and learning disorders (achievement); and consideration
of malingering.
These
are listed below and discussed in more detail in the chapter on assessment of
adults by J. Russell Ramsay, Ph.D. in the 2015 edition of my ADHD Handbook
for Diagnosis and Treatment (Guilford Press).
- Use
self-report of ADHD symptoms
- For
current symptoms, use DSM-5-TR flexibly (lower threshold 4+ symptoms)
- For
childhood recall of symptoms, use DSM-5-TR for children (6+ symptoms)
- Mandatory
corroboration of symptoms and impairments by someone else
- Obtain
paper trail of impairments (archival records)
- Establish
the onset of symptoms by age 12
- Chronic
course; no periods of remission
- Impairment
in major life activities (by interview and Barkley Functional Impairment
Scale; Guilford Press)
- Use
average-person standard, not intra-person
- If
impairment came much later in late adolescence or adulthood, explain why
- Use
rating scales of adult ADHD symptoms (Conners scale, Barkley scale)
- Use
rating scales of Executive Functioning (tests are far less sensitive than
ratings; Behavior Rating Inventory of Executive Functioning – Adults;
Barkley Deficits in Executive Functioning Scale)
- Rule
out other disorders, explanations:
- low
IQ or Learning Disorders (IQ & achievement screening tests)
- anxiety
or depression as causes of inattention (Symptom Checklist 90-R rating scale)
- Sluggish
Cognitive Tempo/Concentration Deficit Disorder (see Fact Sheet at
www.russellbarley.org)
- Document
comorbid disorders (highly likely to be found) using structured interview of DSM-5-TR
criteria for relevant disorders that seem likely to be present given the
initial interview
- Evaluate
for possible malingering (high in college student referrals)
- Triangulate
results of multiple sources and methods
- Consider
using symptom validity tests
- No
fool-proof means to establish malingering with certainty
The Important Role of Clinical Judgment
As
noted earlier, no precise age of onset of symptoms producing impairment should
be required for a diagnosis of ADHD. The DSM-5-TR recommends age 12 but an upper
boundary of ages 16-18 has been recommended by others based on extensive
research on the issue. Typically, my colleagues and I require corroboration of
ADHD symptoms and impairment from someone else who knows the person well – such
as parents, siblings, or spouses/partners – as part of a clinical diagnosis of
ADHD.
The
clinician conducting the interview should exercise judgment as to
whether the patient’s reports on these matters could be considered to be
realistic or have some veracity. As a consequence, a few individuals may be
clinically diagnosed as having ADHD by the clinician despite their not meeting
diagnostic criteria strictly by their own initial self-report. Others who meet
criteria based solely on their self-report may not be granted the clinical
diagnosis of ADHD. The latter may have other disorders that interfere with attention,
such as anxiety disorders or depression, but do not have the cardinal features
of ADHD (chronic ADHD symptoms from childhood). A moment’s reflection will show
several reasons for why this necessarily has to be the case.
First,
the self-reported ADHD-like symptoms may be clinically judged to be better
accounted for by the presence of another diagnosis (such as dysthymia,
depression, anxiety, substance abuse, marital problem, a situational stressor,
etc.). This is a requirement of the DSM criteria for ADHD that may often go
overlooked in research studies that select their ADHD group merely by rating
scales or solely on self-reported information. This criterion can only be
executed via clinical judgment and knowledge of differential diagnosis and cannot
be incorporated into some mindless algorithm that relies exclusively on
self-reporting.
Second, the symptoms that patients endorse and/or the associated impairments they allege may not rise to the level of being clinically significant in the clinician’s judgment. DSM criteria require that symptoms be both developmentally inappropriate and lead to impairment, which inherently involves clinical judgment. For example, a patient may endorse 14 of the 18 symptoms but the examples of the symptoms given were judged to be clinically trivial and the impact they had in producing clinically significant impairment is either minor or non-existent. Likewise, another patient may give evidence of having no real impairment other than an internal perception that they were somehow not working up to their potential or not being as successful or effective as they thought they should be. In other words, there is no other historical corroborative evidence in these reports that the behavior of which they complain is actually a symptom (abnormal) or that the impairment claimed is so interfering with their functioning that it resulted in being well below the average-person standard discussed above. For example, in the second patient’s case, despite their reported symptoms, they had suffered no problems in school, had received no prior psychological treatment, had received no accommodations for a disorder at school or at work, was happily married, demonstrated no occupational impairment, or failed to manifest convincing social or daily adaptive impairment that in the clinician’s judgment was significant and a consequence of ADHD. In some cases, these are what one might call “ADHD wannabes” who are self-diagnosed before coming into the clinic, typically based on reading a popular trade book on ADHD in adults or hearing media accounts of the disorder and believing themselves to have it. In short, to be eligible for the diagnosis of ADHD, patients have to have a sufficient number of DSM symptoms that in the clinician’s judgment produce clinically significant real-world functional impairment in major life activities.
Third, for the clinician to render an ADHD diagnosis, they need to see fairly compelling evidence of an onset of symptoms sometime during childhood or adolescence, a chronic (unremitting) and pervasive pattern of ADHD symptoms, and impairment that could be reasonably attributed to ADHD. The clinician should not simply record mere self-reported symptom counts or statements of impairment, relying solely on a judgment-free algorithm. It is clear that some patients do not have a good perspective on what constitutes impairment. For example, a patient may have denied having any significant impairment, yet a closer look at their history and school, driving, and other archival records may show substantial struggles in school achievement and deportment, in adverse driving outcomes, in conduct in the community (delinquency), in their job performance or social relationships, or in just managing daily major responsibilities. However, they might have simply chalked it up to "I just hated school" or their job, or their friend or partner, etc., rather than viewing it as stemming from any sort of disorder.
Finally,
there has to be convincing evidence that the symptoms actually developed and produced
impairment sometime during childhood or adolescence. Consistent with the criticisms
raised above about the DSM criteria for ADHD, when many patients are asked about
onset, they have a hard time specifying an exact age. They use phrases such as
"as long as I can remember,” "always," "forever," etc.
Others give evidence of a very poor memory of their childhood and cannot
remember when they first noticed problems, yet they may have given the
clinician other information that helped attach an age to the onset of symptoms
producing impairment (such as getting suspended or held back in first grade).
In addition, some might say their impairment began in high school, yet during
the interview or from inspecting school records it becomes clear that the
impairment had begun much earlier. Our research in fact showed that, on
average, patient reports of age of onset were 4-5 years later than was the
actual onset as recorded in longitudinal studies following them from childhood
to adulthood. And we found that parent reports were no more accurate concerning
retrospective recall of age of onset of their child’s symptoms when judged at
the child’s adult follow-up. Hence, differences could exist in self-reported
perceptions of onset (and even parents’ reported age of onset) versus a
clinician’s determination of onset based on the totality of information
received during the assessment.
Clinical Tips
As noted above, various limitations have been evident in the DSM criteria across the manual's many editions. It's important to be aware of those that persist and how to deal with them to produce the most accurate diagnosis for your patients.
1. Particularly when assessing adolescents (or adults), don’t place so much emphasis on the hyperactive symptoms. Six symptoms out of nine on the DSM list reflect excessive activity, even though for at least the last 40 years impulsivity has been viewed as just as much if not more involved in ADHD as hyperactivity. Hyperactivity is at best reflective of early childhood disinhibition of motor movement and declines so steeply over development that such symptoms are of little diagnostic value by late adolescence and certainly by adulthood. This is one reason clinicians before the 1980s thought the disorder was outgrown by adolescence. Today, the symptom list is losing its sensitivity to detecting true disorder over development.
2. Look for additional symptoms of impulsivity. Poor inhibition should be reflected not just in speech (currently the DSM criteria include only three verbal symptoms) but in other domains such as motor behavior, cognition, motivation, and emotion. Ask parents whether their children:
- Often fail to consider the consequences of their actions;
- Have trouble motivating themselves to persist toward goals;
- Have trouble deferring gratification or waiting for rewards;
- Lack willpower, self-discipline, drive, determination, and “stick-to-it-iveness”; and/or
- Seem unusually impatient, easily emotionally aroused, easily frustrated and quick to anger
None of these aspects of disinhibition or poor self-regulation are included in the DSM-5-TR (or earlier) criteria, yet abundant research shows they are as common in people with ADHD as are the traditional DSM symptoms and, with age, more so than those of hyperactivity. Be sure to ask about them anyway.
3. Use rating scales of ADHD symptoms that have their norms broken down by sex and not just by age. The DSM-5-TR criteria fail to recognize that females may be as impaired as males but at lower symptom thresholds, because (a) females become impaired in certain domains of functioning at lower levels of symptoms than do males, and (b) males were overrepresented in field trials for earlier versions of the DSM, thus making the symptom threshold gender-biased. Research suggests that females in the general population, at least in childhood and adolescence, do not show as much of the symptoms as their male peers, making it harder for a female to meet the DSM criteria even though she may be just as impaired as a male.
4. Think of inattention as metacognitive and other executive function deficits in daily life, particularly those reflecting self-awareness, working memory, poor self-organization, poor emotional self-regulation, and deficient time management. That way, you will know to go beyond focusing merely on DSM symptoms in your assessment of your clients in your interviews and selection of rating scales, among other assessment methods. You will also know in your open-ended initial interview to listen for these types of complaints in order to better help you identify whether ADHD is present or not. You also can better understand the pervasive impact of their symptoms on their daily functioning in major life activities as they explain to you all of the domains in which they are ineffectively functioning. Furthermore, you can better explain the nature of their disorder to them in the feedback conference when your evaluation is completed, allowing them to better understand why their condition is so serious, impairing, and pervasive across major domains of life. It will also help you to appreciate why teens (and young adults) may seem to be outgrowing ADHD, based on DSM criteria, when they are far less likely to be outgrowing their EF-SR deficits and may even be demonstrating increased impairment with age.
5. Don't adhere too rigidly to thresholds for meeting diagnostic criteria when there are clear signs of significant impairment. You are not making a dichotomous decision – disorder or no disorder – or dealing with symptoms whose presence or absence creates a sharp distinction between the two. Keep in mind that ADHD (and EF-SR) is not a category but a dimension. Empirical research asserts that ADHD falls along a continuum in the general population. It is a developmental disorder distinguished more from others by a quantitative difference from normative behavior than as a qualitatively distinct category. So you will see clients who don't meet all of the DSM criteria yet who are experiencing impairment and seek out your assistance with alleviating or at least compensating for it. As practitioners we are valued by society not so much because we can make diagnoses but because we relieve suffering; the rendering of a diagnosis is a means to that end and not the end itself. This means you should diagnose ADHD if:
- Your clients or their caregivers state that the child or teen has a high number of ADHD (and EF) symptoms (above the 20th–16th percentile or so in severity) and there is evidence of impairment in major life activities (harm), even if the client fails to meet all DSM-5-TR criteria; and/or
- Symptoms developed sometime during development, usually before ages 21-24 or so and meet all other criteria for the disorder. DSM-5-TR has raised the age of onset for ADHD from age seven to age 12, but research repeatedly shows that both patients and those who know them well are not reliable or accurate in recalling the age of onset of the symptoms and hence the disorder. It is a mistake therefore to consider age of onset in diagnosing ADHD, all else hitting the stated thresholds.
Impairment is key to diagnosing ADHD.
6. Always consider the source of information when assessing a child or teen for ADHD. The DSM has a requirement for cross-setting occurrence of some symptoms in the diagnostic criteria, but some care must be taken not to confuse that with differences in the reports of others being called on to provide information about the individual. At the individual level of analysis there can be substantial differences in the number and severity of symptoms reported by different observers across the different contexts they supervise. For example, it is well known that parent and teacher agreement on any dimension of psychopathology in children or teens is notoriously low, with correlations averaging just 0.25–0.30. To avoid conflating such natural reporter disagreement with cross-setting occurrence, the DSM should be understood to require that only one or more symptoms need to be present in any given situation as reported by one source, while more symptoms producing impairment may be reported in other settings by other sources. It is the total number of different symptoms endorsed across such reporters that needs to rise to the required symptom threshold (six for children, five for adults). You do not need six (or five) from both sources.
The same caution about conflicting observer reports applies to comparing self-reports by children and teens with ADHD and their parent or others’ reports of their ADHD symptoms. Up until the client is in their twenties, the correlation between self- and other reports is only modest, reflecting low degrees of agreement. The EF-SR theory of ADHD explains this phenomenon: the development of executive functions that create self-awareness lag behind in those with ADHD. Therefore, you should adhere to the newly inserted criterion in DSM-5-TR to corroborate what patients are reporting through another source. If no parent, sibling, or long-term caregiver is available, then available archival records may have to suffice, such as earlier medical/psychiatric records, educational transcripts, or report cards, driving records, work history, etc.
7. Think of – and explain – ADHD as being the diabetes of mental health. DSM-5-TR specifies that impairment may exist in home, educational, peer, or occupational settings, but, because it still focuses on ADHD as deficits in attention or activity regulation, it does not convey how far beyond these domains ADHD has an adverse impact. When you view ADHD as founded in deficits in executive functions and self-regulation, which are requirements for functioning well in most domains of life, you can not only better understand why your clients are struggling to function effectively in so many domains of life and health but you can also better explain to them and their loved ones why that is the case. And why it is imperative that the disorder be treated on an ongoing basis as if it were the diabetes of psychiatry. I return to this point in later chapters that deal with impairment and with adopting the treatment framework provided by the EF-SR theory.
8. Don't assume that ADHD disappears in adolescence. DSM criteria are progressively less developmentally sensitive with increasing age. They lose their capacity to detect true disorder to some extent by adulthood. But if we apply developmentally relative criteria for a diagnosis such as exceeding the 93rd (+1.5 SD) or 98th (+2 SD) percentile relative to same-age peers and requiring evidence of impairment, up to 56% and 49% of childhood cases, respectively, continued to be symptomatic even if not fully diagnosable by DSM criteria. And if we had employed more symptoms of EF-SR deficits beyond the traditional ADHD symptoms, even more cases would be classified as developmentally deviant. Notice that using a developmental approach to diagnosis identifies twice as many cases as being persistent in their disorder as do the DSM criteria.
If the presence of impairment was the only criterion employed, then over 80%-85% were still impaired in one or more daily life activities by adult follow-up. During my research collecting population-representative norms for my EF rating scales (see separate manuals for children and adults), I observed that despite the well-known decline in ADHD symptoms in the general population with age from childhood into adulthood (and onward) [as seen on ADHD rating scales], there was little or no obvious decline in the various EF components on those ratings across childhood (ages six–18), such as for self-organization, time management, self-motivation, self-restraint, and planning/problem-solving. What this likely means is that the ADHD symptom lists are not capturing the far wider range of EF deficits associated with this disorder that are not declining with development as much as are the more childhood-focused traditional DSM symptoms.
All
of these issues should be kept in mind when making the diagnosis of ADHD. The
DSM-5-TR should be viewed as providing only rough guidelines for making this
diagnosis in adults, and requires sound clinical judgment to implement the
guidelines properly in adult cases. Interview and rating scale forms that the
clinician may find helpful in conducting this evaluation can be found in my
rating scales of adult ADHD and Executive Functioning more generally (See Resources).
Moreover, impairment can be assessed using my new impairment rating scale which
for now remains the only normed rating scale of adult impairment.
Impairments: What Are the Consequences of Untreated ADHD?
Unmanaged
ADHD can lead to numerous adverse consequences in many areas of adult daily
life. Here are briefly described the various domains that can be negatively
impacted by adult ADHD. More detail on these impairments can be found in others
of my courses on adult ADHD. These are the domains for which clinicians are
going to have to provide treatment. After all, treatment should not be targeted
only at symptom reduction but at decreasing impairments in major life
activities. Such advice occurs later in this course. For an even more detailed
look at these various domains of impairment, see my textbook, Attention
Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment (4th ed., 2015). Not all adults with ADHD experience impaired functioning in all of
these areas, but such an adult is more likely to have difficulties in these
domains than would a typical adult. Yet with clinical help and proper
treatment, much improvement can usually be made in these domains for the adult
with ADHD.
Clinicians
will see that ADHD has a pervasive negative effect in someone’s life if it is
not properly treated. While such a diagnosis can initially prove discouraging
to the adult patient with ADHD, the fact is that ADHD in adults is among the
most treatment-responsive psychological disorders currently known. This brief review
is to show that adult ADHD is a serious condition if not properly treated, and
to help clinicians motivate clients to take it seriously and get treatment.
Before
discussing some specific impairments with which adult ADHD is associated in
various major life activities, it may be helpful to distinguish among the terms
“symptom,” “disorder,” “impairment,” and “disability,” as used here. As I have
written elsewhere, I consider symptoms to be the cognitive and
behavioral expressions of a possible disorder shown by an individual. A
psychological or psychiatric disorder exists when such symptoms reach
such an abnormal or statistically aberrant degree of frequency or severity as
to result in impairment in one or more major life activities. Disorders begin
where impairment begins.
Impairment to me refers to
the degree of functional ineffectiveness an individual is experiencing in a major
life activity where such ineffectiveness has reached a degree where serious
harm or adverse consequences are occurring to the individual as a result. That
is, the ineffective functioning has reached such a degree that the environment
is “kicking back,” or generating adverse consequences. So, symptoms are the
expressions of a disorder while impairment is the consequence of those
expressions.
A disability is a domain- and setting-specific term used by government and
regulatory bodies to refer to the degree of impairment (functional
ineffectiveness) an individual may be having in one or more major life
activities that warrants either protection from discrimination, as under the
Americans with Disabilities Act; or an entitlement to societal support, as
under disability insurance, workman’s compensation, or the Social Security
Administration. A disability is typically judged as existing against the
standard of a normal or typical person, which is to say that the individual
must be functioning significantly below the typical adult in the general
population, and not just relative to their general cognitive ability or a
highly specialized peer group (i.e., law students). While professionals often
use the term impairment and disability to mean the same thing, government and
regulatory bodies have their own definitions of a disability that must be met
in order to gain access to certain protections and entitlements.
Major Life Domains
Returning
to the discussion of impairments associated with adult ADHD, below are two diagrams
showing many of the domains of impairment that can occur or have already
occurred to a far greater extent in adults with ADHD than in the typical adult
population. The first deals with domains impaired during childhood and the
second with those likely occurring in adulthood. Space does not permit delving
into each in much detail, but below are summaries of at least what is known
about the risks that arise in most of them.
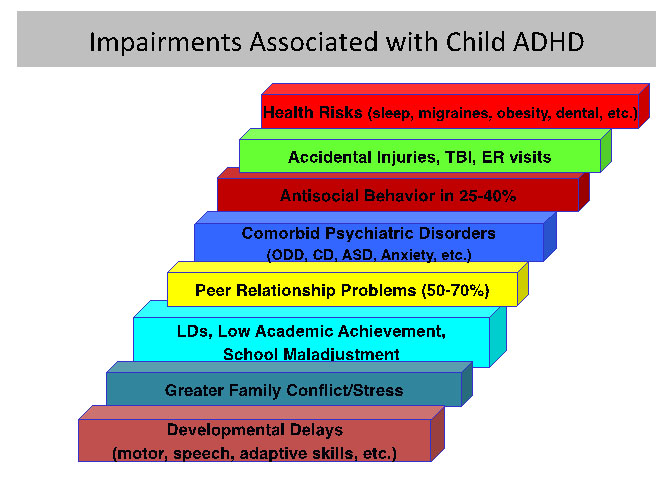
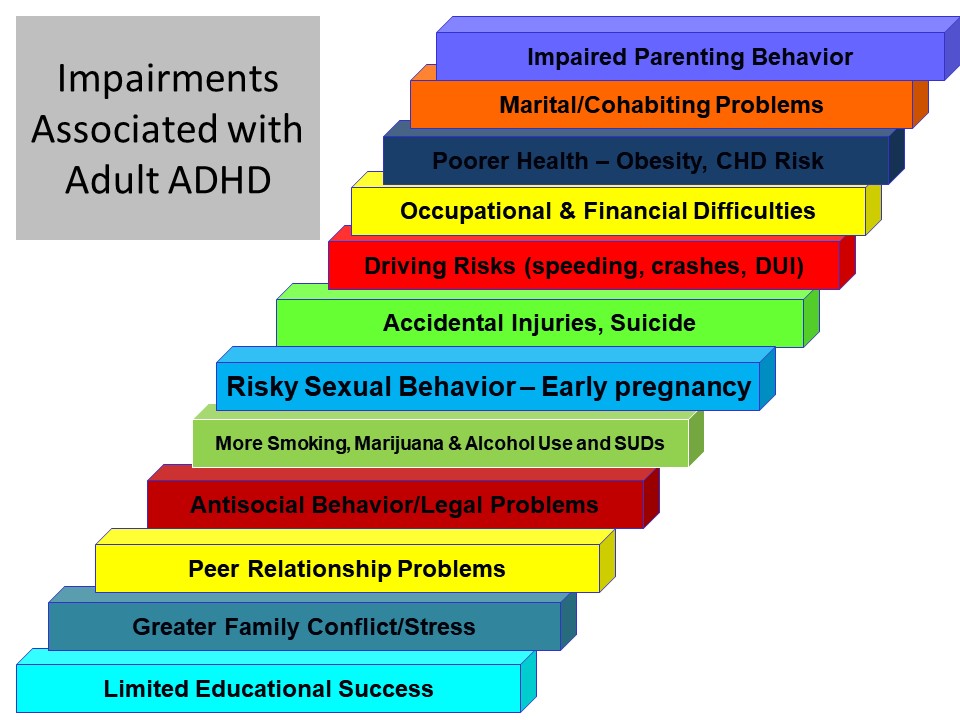
Consequences
at School
Undoubtedly, the domain of education is the one most likely to be adversely
affected in the histories of adults having ADHD and it is affected more
severely than might happen in other domains. This is especially so in childhood
and adolescence because of the requirement to be in school during these years.
But adult ADHD can also have an adverse impact during young adulthood if the
adult with ADHD went beyond high school for any additional education. And ADHD can cause problems in their current life if they are participating in any adult
continuing-education programs, such as additional college or technical training
or work-related training. All of this makes perfect sense when clinicians
consider the problems ADHD produces in inhibiting behavior, paying attention,
remembering instructions, resisting distractions, sitting still, and being
quiet. It is even more obvious when clinicians consider the executive deficits
discussed above – poor time management, self-organization, problem solving,
emotional self-control, self-restraint, and self-motivation. All of these
mental abilities are essential for functioning effectively in school or in any
other educational setting as an adult.
People
with ADHD are more likely to have been held back in a grade (25%-50%), placed
in special education (50%-80%), suspended for inappropriate conduct (20%-60%),
expelled (10%-15%), or to have quit (10%-35%) before completing high school.
They are therefore less likely to attend college. And, if they do attend, they
are less likely to complete that program (5%-10% vs. 35%-41% of adults). They
have more days of unexcused absences from school, a lower class ranking in high
school, a lower grade point average in high school, and, if they attended
college, more grades of D and F than adults in a general community sample.
Individuals with ADHD therefore often have less education than do others their
age. Obviously, those with high levels of intelligence are better able to
achieve more years of education and some may even complete advanced graduate
degrees. Yet overall, the educational system can prove to be a very difficult
situation for adults who had ADHD when they were growing up.
There
are well-known downstream negative effects on one’s life if a person does not
get a good education. The amount of money a person is likely to earn both
annually and across their lifetime is directly related to how much education
they received. And the amount of education a person receives is likely to
determine the types of occupations they will be able to pursue. Not graduating
from high school, for instance, results in not getting access to many work
opportunities and types of occupations. This results in a far more restricted
range of work opportunities for such a person than for someone completing high
school or someone who gets at least some college. So even after people with
ADHD eventually leave school, there may be lasting detrimental effects on their
adult lives from their educational difficulties.
Consequences
at Work
The domain of current functioning most impaired in adults with ADHD is that of work or occupational functioning. Again, this makes perfect sense given the symptoms of the disorder and the deficits in self-control and EF discussed earlier. If an adult is poorly inhibited, easily distracted, unable to sustain their attention as long as others, forgetful, and generally demonstrates less self-control or self-discipline than others because of their ADHD, work life can prove to be quite a struggle. Of course, all this depends on the kind of work an adult chooses to do. Some jobs are more ADHD-friendly than others. For instance, an adult with ADHD might find being a salesperson or physical education teacher to be better suited to their ADHD-related symptoms and so will be less impaired by those symptoms in such jobs. But they would find it difficult to deal with their symptoms if they worked at a desk job dealing mainly with paperwork or in which they had to manage a lot of time-sensitive logistics, such as an event planner, builder, or factory plant manager. Yet even when an adult with ADHD finds an occupation in which they are less affected by their ADHD, they may still have trouble with the organization and time management aspects of even these ADHD-friendly occupations. As they enter the workforce, teens and adults with ADHD have more problems in performing their work as well as others. They start working at a younger age than others, which may sound like a good thing for them, but this is probably due to their being less likely to pursue further education after high school or to even graduate from high school. It also means they do not have the skills necessary to move up in entry-level jobs, such as fast-food worker, restaurant busboy or waitress, lawn-care worker, farm field-hand, or construction worker. More adults with ADHD change jobs out of boredom than do other adults. My own research has found that adults with ADHD were two to three times more likely to be dismissed from a job due to poor conduct and were fired from a greater percentage of the jobs they had held since leaving high school than were other adults. More than half of adults with ADHD have been fired from a job at least once and have quit jobs impulsively, with no other job to go to when they quit. Perhaps this explains why a substantial number of adults with ADHD may go for several months or longer being unemployed.
Concerning behavior at work, adults with ADHD show more oppositional behavior such as being hot-tempered, argumentative, or defiant. More than half the adults with ADHD who participated in the study noted above had significant problems getting along with others. They were also less punctual for work, appeared to manage time less efficiently, were more forgetful and disorganized, and so required more supervision than did other workers. Clearly this results in an adult with ADHD receiving lower ratings of their work performance from supervisors than do others without ADHD. All this inevitably leads to an adult with ADHD having a greater likelihood of having formal disciplinary actions taken against them by their employers than would typical adults.
These difficulties as well as a propensity for being more easily bored by work than others may explain why an adult with ADHD spends significantly less time in any given job than do others. As a result, they wind up having held more jobs in their checkered work history than do other adults. All of these problems can lead to lower earnings, less opportunity for workplace advancement, and overall lower-status jobs than adults without ADHD who persist far longer at the jobs they take.
Adults with ADHD also have more accidents at work, suffer more injuries, make more claims for worker’s compensation, and take more unexcused absences from work. They also may use more of their sick leave and spend more of their time at work not being especially productive than do adults in the general working population. They are also more likely to file for disability claims or Social Security Disability Insurance. And if they drive a vehicle for a living or do so often simply as part of their work, they show a greater risk for vehicular crashes. Just as was found with schooling, the workplace setting is likely to pose significant challenges to adults with ADHD more so than other adults, even those with other psychological disorders.
Antisocial
Behavior and Its Consequences
Children with ADHD are routinely found in follow-up studies to be more likely
to engage in antisocial activities, to be arrested, and to be jailed as they
grow up than are non-ADHD children. A substantially greater proportion of
adults with ADHD have engaged in shoplifting, stealing without confronting a
victim, breaking and entering, assaults with fists, carrying an illegal weapon,
being arrested, and being sent to jail than is the case in typical adults. In
addition, more adults with ADHD have sold drugs illegally in comparison to
community control groups. The most common forms of antisocial activity for the
adults with ADHD were shoplifting (53%) followed by assaulting someone with
their fists (35%), and selling illegal drugs (21%). While much of this risk for
antisocial behavior was mediated by the presence of a childhood history of Conduct
Disorder (CD) (established retrospectively), even the non-CD subset of those
having ADHD still committed more antisocial activity than the control groups.
Consequences
in Money Management
Adults with this disorder have a hard time managing their money, paying their
bills, and handling credit. Impulsive people like those with adult ADHD find it
hard to defer gratification, think about and plan for the future, or follow
through on promises and commitments. And so they do not do very well handling
their finances. Adults with ADHD are more likely to use their money unwisely,
make purchases without thinking, and too often use their credit cards on
impulse, resulting in overspending their budgets or income. They are also less
organized and more forgetful when it comes to paying bills on time. These money problems may even have led the adult with ADHD to return to live in their parents’ home because they simply cannot make it financially on their own; at least not yet.
Because
adults with ADHD are less likely to save money and more likely to buy things on
impulse or to go on shopping sprees, their credit card balances are higher than
those of typical people of their age and they often exceed their credit limits
more than adults without ADHD. Many adults with ADHD have trouble sticking to a
budget, if they have made one at all. As a consequence, they are more likely to
have had their utilities turned off because of late or non-payment of their
accounts. Missing loan payments, such as for car loans, is also more common in
adults with ADHD than in other adults, which may explain why they are more
likely to have their cars repossessed. It should be obvious from this why
adults with ADHD have a poorer credit rating than typical adults.
When
people have difficulty with handling money, they often borrow it from friends,
family, or even coworkers. In our research, we found that adults with ADHD were
more likely to borrow from relatives and friends than did other adults, thereby
placing a greater burden on others to help them with their financial problems
than is the case in adults who do not have the disorder. Trouble handling
money, then, may be yet another reason clients with adult ADHD are in need of
treatment and counseling on financial management.
Consequences
in Friendships
The symptoms of ADHD and its underlying problems with self-regulation are
likely to create numerous social difficulties for adults with ADHD. The list of
18 symptoms listed earlier reads like a scroll of impaired social behavior – lack
of persistence, high distractibility, poorly inhibited behavior, impulsive
decision-making, excessive talking, frequent interruptions, intrusions on
ongoing activities of others, difficulties following instructions, blurting out
of responses in conversations, and inability to engage in leisure activities
quietly. Not surprisingly, adults with ADHD often report significant impairment
in their social relationships.
Studies
of children with ADHD found that at least 50% had no close friends by the time
they reached second or third grade. If the children also had trouble with anger
and defiance, this number rises to 70%. As a result, children growing up with
ADHD are far less likely to have been invited to play at the homes of other
children, to be included in sleepovers with friends, to be asked to birthday
parties, or even out on dates as they became teenagers. For those who are
hyperactive and impulsive, their talkative and generally outgoing and easily
excitable nature may make them fun to have at a party, or in a short-term
relationship. But it can be stressful and overbearing over the longer term.
Such social problems are likely to continue into adulthood in many cases. So
clinicians may hear that the adult with ADHD might have memories of childhood
that are filled with social problems.
The
penchant of children and adults with ADHD to have more problems with emotional
self-control guarantees by itself more mercurial, conflict-ridden, and
distressing relationships with others than is the case for typical people.
Research shows that children and adults with ADHD have significant problems
with anger and hostility. Those problems, not surprisingly, make them more
likely to be rejected by others. This negative effect on others does not take
weeks or years to develop, but can occur within minutes or a few hours of a
child or adult with ADHD entering a new peer group.
Adults
with ADHD often complain of significant problems with both initiating and
maintaining social relationships. They may have unstable personal
relationships, break off those relationships over trivial matters, or have
difficulty with those social skills needed for maintaining friendships. This
may result in their having fewer close friends, and some have even become
social isolates or recluses by middle age. This is, in part, a consequence of a
life-long course of social difficulties and in part an attempt to avoid any further
such hazards. Their relationships are often described as being frequently
punctuated with conflicts with those they considered to be friends or social
acquaintances. One reason for this is that adults with ADHD can have trouble
negotiating and resolving the everyday conflicts with others that anyone is
likely to encounter. Those unresolved conflicts might add up over time, causing
the friendship to end. The greater propensity to show strong emotions during
social interactions with others is often one cause of this among many, though
not all, adults with ADHD. The adult with ADHD is also more likely to be loud,
boisterous, silly, or clownish more than others.
A further difficulty likely to contribute to the social and friendship problems of the adult with ADHD is the adverse effect the disorder has in diminishing their self-awareness or self-monitoring of their ongoing behavior. Adult patients have often said that they simply did not realize just how poorly they were coming across to others during various social encounters. It is not surprising that such lack of awareness leads to social problems with close friends or acquaintances. Moreover, the difficulties adults with ADHD might have taking turns during conversations or social encounters, and their unguarded comments or insensitivity to the social etiquette appropriate to the moment, likewise cause harm in their social relations. These difficulties can arise because an adult with ADHD often does not realize these social violations until it is too late. The social cost has been exacted and others are likely to steer clear of further interactions with them.
Adults with ADHD are often described as being self-centered, demanding, intrusive, or insensitive to the feelings or needs of others. They are more likely to be unappreciative of assistance from others. And they can be socially “sticky,” not knowing when to end the interaction and move on or let the other person do so. It is therefore not just the impulsiveness or inattentiveness of ADHD that tarnishes social encounters with others. It is also the poor emotional self-control, the more limited self-monitoring of social behavior, and the impaired ability to participate in the necessary give-and-take that makes for a successful social encounter.
Thus,
one of the major reasons adults with ADHD can be so demoralized at times about
their situation in life is not just their checkered educational histories or
periodic failures in school or in the workplace. It also can arise in many
cases from this detrimental impact of their behavior on building supportive and
lasting social relationships with others. No wonder adults with ADHD often have
feelings of low self-worth.
Consequences
in Dating, Marriage, or Cohabiting
One
of the most important domains of adult life is in the relationships we have
with people with whom we become intimate, such as in dating, marriage, or
living with a partner. Because of the closeness and frequency of interactions
in such relationships, not to mention the shared responsibilities they often
involve, one should not be surprised that they can be negatively impacted by
ADHD when it exists in one member of that relationship. Divorce rates are
nearly three times higher among adults with ADHD by the time they are in their
mid-40s. Adults with ADHD (especially women) may be less likely to be married
than others of the same age who do not have ADHD because of their interpersonal
difficulties. By mid to late life (60-94 years of age), adults with ADHD may
also have fewer family members involved in their social network and so may
experience emotional loneliness. Even if they stay married, adults with ADHD
are four to five times more likely to report having fair- to poor-quality
relationships than do typical adults. As many as 58% of adults with ADHD have
maladjusted marriages and low levels of marital satisfaction compared to 25% of
typical adults.
The
chart below shows some of the specific problem behaviors that occur in couples
in which one has adult ADHD.
Problems Reported by Couples
Where One Person Has ADHD |
These
were identified as trouble spots by Drs. Robin and Payson in a survey
conducted with couples in which one of the adults had ADHD:
- Doesn’t
remember being told things
- Says
things without thinking
- Zones
out during conversations
- Has
trouble dealing with frustrations
- Has
trouble getting started on a task
- Underestimates
the time needed to complete a task
- Leaves
a mess
- Doesn’t
finish household projects
- Doesn’t
respond when spoken to
- Doesn’t
plan ahead
|
One
factor that may contribute to their relationship troubles and reduced
satisfaction is that adults with ADHD report being markedly more likely than
others to have engaged in extramarital affairs. Another is that adults with
ADHD are often more emotionally impulsive and are especially quick to react to
others with impatience, frustration, and anger. Such behavior can obviously
generate more hostility in close relationships. Even young adults with ADHD who
are in intimate relationships have been observed to engage in more negativity
and less positivity during situations of conflict than do typical young
couples. Perhaps as a consequence, adults with ADHD may be almost twice as
likely to engage in violence in intimate relationships .
Certainly,
we all recognize that financial problems that occur within a marriage or
intimate relationship can be a major source of distress. As discussed above,
ADHD in an adult greatly increases the likelihood they will have such financial
difficulties. These financial problems can be yet another reason for the
greater marital conflict, poor marriage quality, and higher divorce rates
evident in adults with ADHD.
Pera and Robin (2015) wrote about the types of problems encountered in couples
where one has adult ADHD. They include:
- Disorganization;
forgetfulness; poor follow-through
- Combative
communications; poor listening
- Problematic
parenting style
- Poor
decision-making and cooperation
- Self-centeredness
and insatiability
- Learned
helplessness (Giving up on things when “nothing seems to work.”)
- Impulsive
spending; acting without thinking of consequences
- Low
intimacy
- Moodiness
and temper; low frustration tolerance
- Reactive
aggression toward intimate partners
- Lack
of interpersonal sensitivity; impaired empathy
- Mental
rigidity; difficulty with transitions, compromise, and cooperation
- Poor
coping strategies developed over a lifetime of unrecognized or unaddressed ADHD
Studies
conducted with college students in the U.S. and China found that increased
levels of ADHD symptoms were associated with increased fear of intimacy in
intimate relationships, lower expectations for intimacy in their relationships,
and lower relationship self-confidence. Yet the researchers had not found any
greater levels of sexual anxiety in young adults with high ADHD symptoms.
If
the adult with ADHD is in an intimate relationship, the other partner may
experience resentment or anger, or feel over-burdened. They report that it can
feel as if they are raising another child, given the amount of extra time,
effort, and resources they may have to invest in repairing the consequences
caused by the ADHD in their partner. In some cases they may even have suffered
emotional or physical abuse stemming indirectly from the disorder, given that
adults with ADHD have been shown to manifest more violence toward their
intimate partners.
Consequences
in Parenting
ADHD
in a parent can make them less attentive to their children, less rewarding of
their children, more inconsistent in using discipline, and more likely to
respond with impulsive comments, directives, commands, or reprimands. In
general, they can be more hostile toward their children than typical parents
are. While this is not always the case for every parent having ADHD, on average
they are more likely than other parents to manifest these difficulties. Parents
with ADHD also seem to be less adept at problem-solving as it applies to
dealing with child behavior problems. The home life that such parents arrange
for their children has also been noted to be less organized, more chaotic, and
to have routines that are less structured and inconsistent than occurs in
typical families. Thus, parents with high levels of ADHD symptoms or a full
diagnosis of the disorder clearly struggle with maintaining a consistent, calm,
and organized approach to managing children.
Given
that the children of adults with ADHD are also more likely to be ADHD as well
as oppositional, the ADHD in both parent and child can greatly magnify the
problems in family functioning. The impaired parental behavior created by adult
ADHD can obviously result in higher levels of stress in the family lives of
adults with ADHD. This is worsened when the child also has ADHD. It is also
likely that the above parenting problems in an adult with ADHD will contribute
to a greater occurrence of child misbehavior, such as defiance, arguing,
tantrums, and neglect of typical home chores and schoolwork assigned to that
child. Again, if that child also has ADHD, the odds are even greater that these
other difficulties with defiance and chores and schoolwork will arise.
As
noted above, parents with ADHD are less likely to monitor their children’s
activities than do parents who do not have ADHD. Inadequate parental monitoring
of their children is one of several factors that can increase the risk of
accidental injuries in those children. This may help to explain, in part, why
children with ADHD have higher rates of such injuries of all types than do
typical children. Not only are children with ADHD more impulsive and
risk-taking, their parent with ADHD may be less attentive to their activities, may
be monitoring them less often, and thus may be less able to detect and prevent risk-taking
behavior that can lead to accidents.
One
might think that such parenting problems would be a very good reason for the
parent with ADHD to get additional professional help with child management,
such as is commonly done in standard parent-training programs for parents of
defiant children. But if that parent’s ADHD is not being treated, it can
interfere with their success in such a training program. This is yet a further
reason why adult ADHD needs to be identified, diagnosed, and treated – it has a
detrimental effect on the family ecology, child rearing, and response to child
management training.
Parental
ADHD can also be yet another factor that could potentially damage a person’s
marital harmony besides those issues mentioned above under Consequences in Marriage.
It can do so by contributing to a greater degree of stress that one or both
parents may be experiencing in raising their children. Adults with ADHD who
have children are substantially more stressed in their roles as parents than
are other adults. This stress stems partly from the parent’s own symptoms of
inattention, distractibility, and poor impulse-control. It is also related to
their difficulties with controlling their emotions and to the other EF
difficulties discussed earlier (time management, organization, etc.). But it
can also arise from the fact that adults with ADHD are eight times more likely
to have children with ADHD than typical adults because of the strong genetic
contribution to this disorder. Research suggests that 30%-54% of children of
adults with ADHD will also have ADHD, thus creating an even more ADHD-filled
family environment. Also, the children of adults with ADHD may be more
oppositional and defiant even if they do not have ADHD. Children who argue,
defy, throw tantrums and otherwise refuse to obey can place a great deal of
stress on even typical parents. But such behavior in a child can overwhelm
adults who have ADHD and emotion-regulation problems of their own. Having a
child with ADHD, regardless of whether or not one parent has the disorder, can
significantly increase the risk that those parents will divorce. Should one
parent also have ADHD, those odds are further increased, unsurprisingly.
Risky
Sexual Behavior
ADHD is not associated with any higher incidence of sexual disorders,
thankfully. But my own research with Dr. Mariellen Fischer and other colleagues in Milwaukee found some other problems with sexual
behavior. We found a pattern of early initiation of sexual intercourse during
adolescence (one year earlier on average) and an overall riskier pattern to
their sexual activity as teens or young adults (more partners, less use of
contraception). This riskier pattern of conduct led to a nearly 10 times
greater risk for having been involved in a teen pregnancy, either as the father
or the mother (38% for the ADHD group vs. 4% for the control group). We also
found a four times greater risk for having had any sexually transmitted
diseases (STDs) in the ADHD than in the control group (17% vs. 4%) by age 20.
These patterns of sexual risk-taking and even early parenthood continued into
the young adult years in the group with ADHD. Young adults with ADHD become
parents far earlier than do others, sometimes as teenagers when they are not
prepared to be parents to a baby. Kate Flory, Ph.D. and her colleagues found similar risks in their own follow-up study in
Pittsburgh, further confirming this increased problem with risky sexual
behavior. For this reason, teens and young adults with ADHD seem more likely to
place their children up for adoption or have the children be raised by their
own parents (the baby’s grandparents) than might other teens or young adults.
Health and Medical Problems
There
is a small but growing amount of scientific evidence that children and adults
with ADHD are prone to certain health problems more than others. For several
decades we have known that adults with ADHD voice more complaints about bodily
symptoms, such as headaches, stomachaches, and vague bodily concerns that may
have little if any medical origins. These are known as “psychosomatic” or
“somatoform” symptoms.
Sleeping
Problems
More
adults with ADHD have sleeping problems (40%), than do those without the disorder.
These are not the result of taking stimulant medication for their ADHD,
although sometimes those drugs can result in more insomnia than usual. Even
off-medication, adults with ADHD report more insomnia or trouble getting to
sleep, more restlessness while sleeping, and more waking during the night.
Those adults also have a greater chance of having restless leg syndrome, a
condition in which they feel that their legs have to be moving for them to be
comfortable. An adult with ADHD also may have less efficient sleep, more
breathing problems during sleep, and report being more tired the next day. That inefficient sleep and greater tiredness can make their problems with attention worse, as clinicians can imagine. Treating their ADHD symptoms with medication during the daytime can sometimes help reduce these sleeping problems. Some research
suggests that taking melatonin at bedtime (delivered under the tongue) may help
induce sleep earlier than usual. Otherwise, the sleeping problems may need to
be directly treated with other medical and psychosocial interventions. Some
adults with ADHD find it helpful to create a “going to sleep” routine in which
they disengage from technology, social media, and other more exciting
activities, especially those that involve focusing for extended periods on a
lighted computer, smartphone, or iPad screen. Also, this can include taking a
shower at night before bedtime rather than in the morning, reading, or having
light conversation with a partner before falling asleep, and then turning on a
sound generator that plays soft music without lyrics or even a “white noise”
machine so there is some background stimulation.
Excess
Weight, Obesity, and Eating Disorders
Another
problem for adults with ADHD is an increased risk for being overweight or
having obesity. Adults with ADHD, or those children who grew up with it, are
twice as likely to be obese (have a body mass index over 30) than typical
adults. Likewise, adults who are obese are six to eight times more likely to
have adult ADHD. This relationship of ADHD to obesity arises as a result of the
poor impulse control specifically, and poor self-regulation (executive functioning)
more generally linked to ADHD. If clinicians couple that with situations where
junk food is readily available, it is no surprise that the adult with ADHD
tends to consume more such food than others. But it is also the case that
adults with ADHD do not exercise as often, pay less attention to maintaining a
healthy lifestyle, smoke more tobacco and marijuana, drink more alcohol, and
are more likely to interact with electronic media such as TV, Internet
videogames, etc. Teenage girls and women with ADHD may be three to six times
more prone to binge eating or even the more extreme disorder of bulimia. This
is especially so if they also have co-existing anxiety or depression. All of
these factors may contribute to the risk of being overweight that can be
associated with adult ADHD. Some research now shows that treating ADHD with
medication in such obese individuals is likely not only to improve their ADHD
but also to result in reduced weight (a well-known side effect of ADHD
stimulant medications).
Heart
Disease
By adulthood, children growing up with ADHD may have significantly lower HDL
cholesterol (high density lipids or “good” cholesterol) than do typical adults.
This gives adults with ADHD a poorer HDL-to-Total cholesterol ratio, both of which
are risk factors for future cardiovascular or coronary heart disease (CHD).
Future risk of CHD has been repeatedly linked to several health and lifestyle
characteristics, with the most frequent being: smoking, high blood pressure,
elevated serum cholesterol (and specifically HDL:LDL and HDL:Total ratios),
excess body mass index, diabetes, and infrequency of exercise. In the study
noted above, it was found that the risk of developing CHD was 26% higher for
the next five-year period and 33% greater for the next 10-year period of life
if current lifestyles were to continue for our ADHD group. And this was at the
young adult age of 27, on average. The point here is that growing up with ADHD
that persists into adulthood is associated with an increasing risk for CHD in
future years, even if at a small magnitude of risk at young adulthood. It was
also found that adults with ADHD that had persisted since childhood had a 40%
greater risk for current and future atherosclerosis of the coronary vessels.
Once again, if clinicians think or already know that the adult with ADHD may show such a high risk profile for CHD, that is but one more reason to encourage them to get treatment for their ADHD (and CHD risk) if they have not done so already.
Excessive
Substance Use and Abuse
Adults
with ADHD are predisposed to difficulties with substance use, dependence, and
abuse, regardless of their sex. Those adults are more likely to smoke
cigarettes and marijuana than other adults and to smoke more of these
substances than do adults without ADHD who routinely use them. Once they begin
smoking, adults with ADHD may increase their use more rapidly than others who
experiment with tobacco. One reason for the greater use of tobacco may be that
it serves to partially treat ADHD symptoms. Nicotine, the addictive compound in
tobacco, is a stimulant that has been shown to improve symptoms of ADHD. So
this might be an instance where some adults with ADHD are self-medicating, that
is, self-treating their disorder with nicotine. Even where that is not the
case, the poor impulse control associated with ADHD would make an adult more
likely to use and less likely to be able to quit using tobacco or other
potentially addictive drugs.
Caffeine
is also considered a stimulant. Not surprisingly, research finds that young
adults with ADHD consumed more caffeinated drinks per week than did young
adults in the control groups. Again, this might be an effort at self-medication
– trying to treat the ADHD symptoms by increased use of readily available
stimulants. But caffeine is not especially effective at doing so because it
increases the wrong neurotransmitter in the brain (epinephrine) and in the
wrong regions (brain stem) than those involved in adult ADHD. So clinicians
should not encourage the adult with ADHD to just drink more coffee or other
caffeine-containing beverages to try to manage their symptoms.
Alcohol
is another substance that adults with ADHD seem to use more often than typical
adults, even though in this case it does not treat their symptoms. But it may
give them a temporary sense of wellbeing, help reduce their focus on their
problems, and even reduce any anxiety they may be experiencing over those
problems. Perhaps this is why some of them drink more alcohol than is typical.
Alcohol is known to temporarily constrict or reduce awareness of or concerns
about time, such as the past and future. For that reason, it may help reduce
concerns about ongoing problems and conflicts. Interestingly, some of the genes
that seem to be linked to ADHD are also known to convey an increased risk for
substance use disorders such as nicotine abuse and alcoholism, providing yet
another explanation for the increased consumption of these substances.
Accidental
Injuries
For
more than 40 years, scientists have known that children with ADHD are
considerably more likely to experience injuries due to accidents of all types
than are children growing up without ADHD. Interviews with parents of these children
find that:
- As
many as 57% are described as accident-prone.
- More
than one in five is likely to have experienced at least one episode of
accidental poisoning compared to a risk of just one in 12 for children without
ADHD.
- More
than one in four will suffer bone fractures compared to one in eight children
without ADHD.
- As
many as one in six children with ADHD have had at least four or more serious
accidental injuries, such as broken bones, lacerations, head injuries, burns,
severe bruises, lost teeth, or accidental poisonings.
- The
injuries children with ADHD sustain are also more frequent, more severe, and
potentially longer-lasting.
Other
studies have found that children with ADHD are more likely to be involved in
either pedestrian-auto or bicyclist-auto accidents while they are out playing
in their neighborhoods than are other children. Also, when someone with ADHD
has an accident as a child, the accidents are more serious ones and the
injuries they suffer are likely to be more severe and long-lasting than is the
case for children who do not have ADHD. Recent research suggests that treatment
with stimulant medication can reduce these risks of accidental injuries.
Beyond
these childhood risks, adults with ADHD continue to be at a higher risk for
experiencing accidental injuries at home and at work. Because of these greater
risks of accidental injuries and other such injuries, ADHD can be considered a
life-threatening disorder. It is therefore not surprising to learn that children
with ADHD (and other disruptive behavior problems) were more than twice as
likely to die before the age of 46 than children without the disorder (2.8% vs.
1.3%). Recently, adults with ADHD have been found to be 1.8 times more likely
to die during any four-year period relative to typical adults, and these deaths
are three times more likely to have resulted from accidents. Across adulthood,
those with ADHD are nearly five times more likely to die compared to typical
individuals, often as a consequence of accidents or suicide. Given all of the
health risks noted above, and especially the risk for accidental injury, if
left untreated across adulthood, ADHD may well shorten a person’s life
expectancy by as much as 7-13 years (Barkley et al., 2019; O’Nions et al., 2025).
Driving
One
area of adult life that poses serious risks for someone with ADHD is driving a
motor vehicle. After all, since inattention is the most common cause of
accidents while driving, ADHD (being a disorder of attention) would be highly
likely to cause far more accidents than would be the case for a typical adult.
Many
studies have focused on ADHD and driving risks. They find that adults with
ADHD:
- have
slower and more variable reaction times;
- make
more impulsive errors;
- demonstrate
more variable steering of their vehicles in the roadway;
- are
far more inattentive and distractible while driving than other adults;
- are
more likely to employ unsafe driving practices, such as not wearing a seat
belt, not keeping their attention on the roadway instead of twiddling with the
stereo controls or radio stations, text messaging or talking on cell phones
while driving, or just socializing too much with others in the vehicle; and
- are
more prone to road rage or driving-related anger and aggressive use of a motor
vehicle when angered.
Such
poor driving habits can easily lead to various adverse consequences in the
driving histories of adults with ADHD. Among these is a three to five times
greater frequency of receiving traffic citations, especially for speeding, as
well as for illegal parking. The latter problem arises from their impatience –
they do not want to take the time it may require in a crowded traffic area to
search for a parking space. So they just park anywhere they like, impulsively.
Given their impaired driving behavior, adults with ADHD are more likely to
experience these adverse consequences:
- experience
50% more vehicular crashes;
- have
more severe crashes as measured by dollar damages and people injured;
- are
involved in more than twice as many accidents in which they were held to be at
fault;
- are
likely to have more accidents while using other vehicles, such as motorcycles,
dirt bikes, all-terrain vehicles, snowmobiles, etc.;
- are
more likely to have had their license suspended or revoked as a result;
- are
more likely to engage in reckless driving;
- are
more likely to drink alcohol and drive;
- are
more impaired in driving from that alcohol than others;
- have
had an average of three times more license suspensions/revocations;
- acquire
nearly three times more speeding citations; and
- have
more than twice as many speeding citations and total citations on their DMV
records.
Fortunately,
the driving-performance problems of teens and adults with ADHD can be improved
with medications. Hopefully, this may serve to reduce their risks for these
adverse and even life-threatening driving outcomes.
Excessive
Internet Use and Addiction
Research
is only beginning to explore the relationship between ADHD and excess use of
technology such as computers, smartphones, etc. for playing games and using
social media. What little has been done so far suggests that young adults with
ADHD are two to three times more likely to use the Internet excessively,
especially for gaming, and to even develop an Internet addiction. Internet or
gaming addiction involves such symptoms as an excessive preoccupation with the
Internet or videogame, uncontrolled impulses to use it, usage more than
intended, tolerance, withdrawal, impairment of control, excessive time and
effort spent, and impairment in decision-making ability concerning the use of
the Internet or videogames. The more severe are someone’s ADHD symptoms, the
more likely they are to develop an Internet or gaming addiction. This risk is
also increased if the adult with ADHD uses marijuana, alcohol, or tobacco. The
risk is further heightened if they have co-existing social phobia and/or
depression with their ADHD. Treating ADHD with medication might reduce
excessive Internet or game use in young adults with the disorder.
Conclusion to Impairments Linked to Adult ADHD
Clinicians can now see that adult ADHD can have a wide array of negative effects on various major areas of adult life when untreated – school, work, money management, friendships, dating and marriage or cohabiting, risky sexual activity, parenting, and health and medical problems. I summarize all of these in a single Figure below.
The economic impact of these problems is substantial for the individual with the disorder, for their families, and for their community. The social and emotional consequences that flow from a life fraught with these adverse outcomes for those with adult ADHD are also just as serious, substantial, numerous, and no doubt troubling. That all of these negative outcomes would arise in conjunction with ADHD is easily understood in view of the symptoms of ADHD and the attendant problems with self-control. What is clear here is that ADHD in adults has substantial and varied adverse impacts on numerous major life activities. In view of all of the health and medical risks discussed above, ADHD is not just a mental health problem, it is also a public health problem.
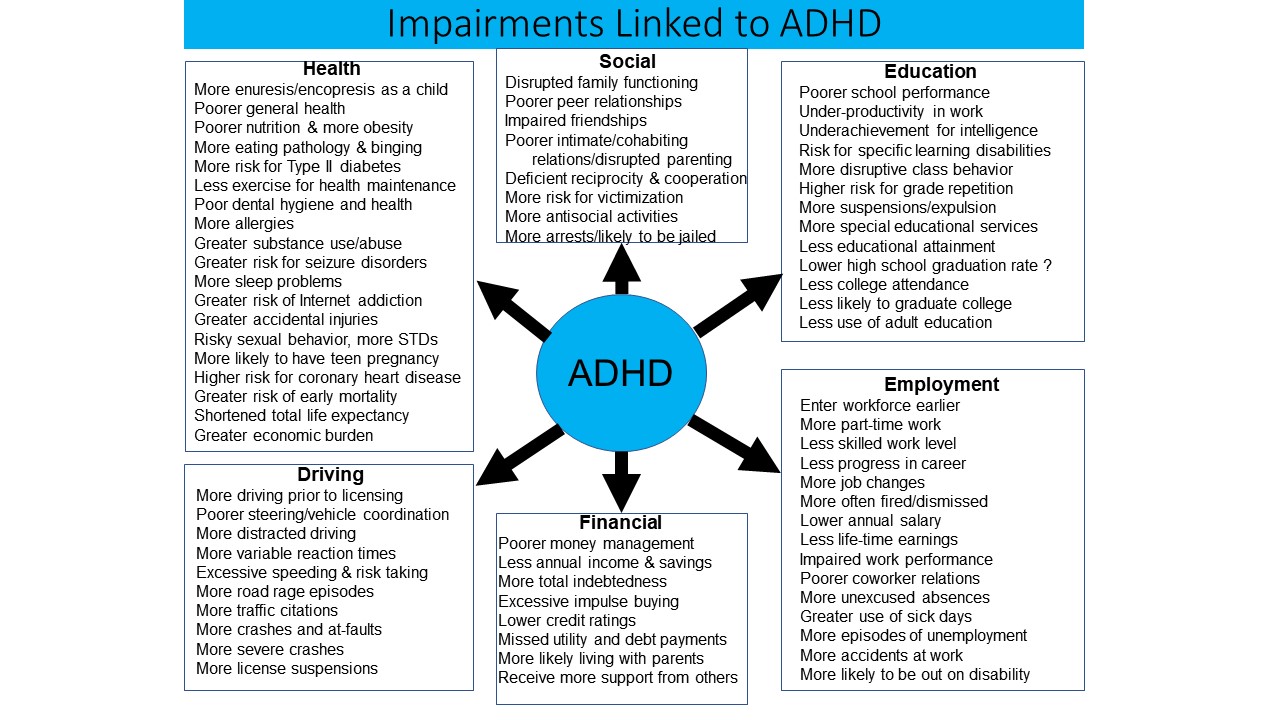
As discouraging as these various risks may seem, they may also serve to motivate adults with ADHD to get and stay in treatment for their ADHD, if they have not already done so, in order to try to reduce these risks. Clinicians will find numerous recommendations in the second half of this course for how best to help the adult with ADHD in dealing with many of the domains of life discussed here. Adult ADHD is a highly treatable disorder; it is more treatable than most other psychiatric disorders. The problems we face are not lack of effective treatments, but a lack of awareness about this condition, the fact that adults with it often do not get referred and diagnosed, and that those adults may not get access to appropriate care.
Comorbid Disorders
While
not necessarily a consequence of ADHD, there is compelling evidence that having
a diagnosis of ADHD increases the liability for certain other psychiatric
disorders.
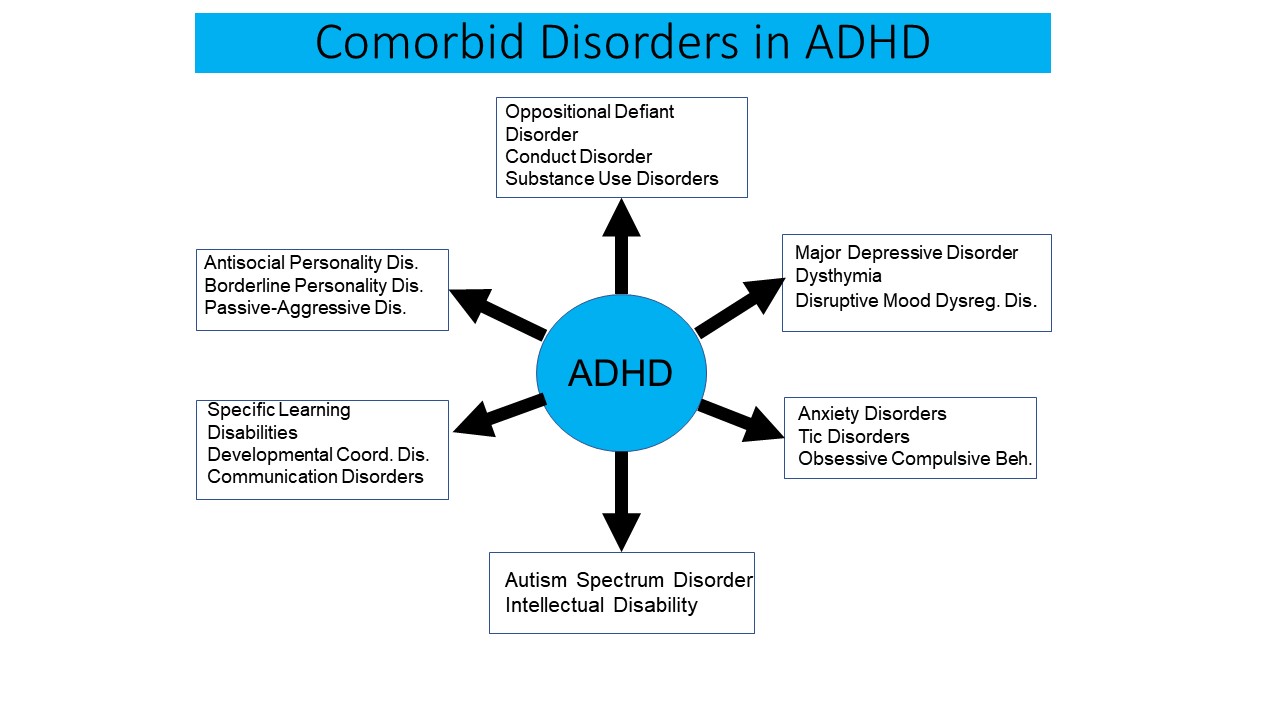
More than 80% of our ADHD groups had at least one other disorder, more than 50% had two other disorders, and more than a third had at least three other disorders, these levels being markedly higher than in our control groups in both studies. As in the prior literature on children and adults with ADHD, we found a markedly elevated risk for Oppositional Defiant Disorder (ODD), and to a lesser extent for Conduct Disorder (CD), in our clinic-referred ADHD group and in our hyperactive children as adults. Current ADHD was especially associated with a childhood history of ODD.
The
internalizing disorders of major depressive disorder, dysthymia, and anxiety
disorders are more likely to occur in ADHD cases referred to clinics than are seen
in a community control group. But MDD and anxiety disorders are also
significantly elevated in non-ADHD clinical control cases seen at the same ADHD
clinic and thus may not be as specifically linked to ADHD as to general
outpatient psychopathology. Even so, both epidemiological studies in children
and adults find some association between ADHD and depression that make it
unlikely that our findings of a limited association are purely due to referral
bias. Nevertheless, the relationships that do exist are not as strong when
comparisons to other clinical samples are used than when comparisons to community
samples are studied. Our Milwaukee Study did not find an elevated risk for MDD
specifically in those with persistent ADHD into adulthood, but did find an
elevated risk for depressive personality disorder and for mood disorders more
generally, both of which suggest some link between ADHD and the level of
depressive symptoms, even if not with full syndrome MDD. Neither study found
any elevated risk for OCD, bipolar disorder, or schizophrenic spectrum
disorders.
Adults
with ADHD have a greater risk for alcohol use disorders and also showed a
greater risk for cannabis use disorders compared to community controls. Alcohol
use disorders and risk for any drug use disorder may be specifically linked to
ADHD, though the level and type of drug use disorders probably have more to do
with comorbid CD and antisocial personality disorder as well as local access to
specific drugs than to ADHD, per se.
Concerning
the risk of suicidal ideation and attempts, ADHD may only slightly increase the
risk for both ideation (25% vs. 15-16%) and attempts (6% vs. 2-4%) prior to 18 years
of age. After age 18, however, ADHD in adults is linked to elevated rates of
suicidal thinking (27-29% vs. 6% in controls). And it has been repeatedly
linked to a greater risk of suicide attempts relative to a community control
group (8% vs. 1%). The greater risks of ideation were largely mediated by the
presence of MDD and, to a lesser extent dysthymia, but were not especially
related to the presence of comorbid CD. The greater risk for attempts is
directly linked to the impulsivity dimension of ADHD.
Addressing Reactions to the Diagnosis
Many
adults have one or more of the various reactions associated with grieving when
diagnosed with ADHD, as noted below. By recognizing these reactions and
understanding their origin (e.g., grieving their diagnosis), clinicians can
help the adult with ADHD negotiate these initial reactions and hopefully come
to a state of acceptance of their disorder. For without such acceptance,
cooperation with subsequent treatments is likely to be suboptimal, if they
engage in treatment at all.
Relief
Fortunately,
most adults with ADHD are open to accepting their disorder and move on to
learning about ADHD following their diagnosis. This is largely owing to the
fact that they initiated the request for the evaluation to begin with and so
had some openness to hearing about the nature of their problems, symptoms, and
impairments. These adults may experience a sense of profound relief at finally
knowing what they have and how it accounts for their life-long struggles. They
can reframe their past from being one in which the problems were due to being
stupid, lazy, or unwilling to improve. In place of self-recrimination, they now
know that ADHD is largely a result of a neurological disorder of the brain’s
executive system.
There
is also relief in knowing that the likely reason for many of the problems these
adults with ADHD experienced in school, work, and/or social relationships was a
subtle neurobiological deficit in the brain over which they had little control.
As Dr. Kevin Murphy explains it:
“Their problems
were not the result of deliberate misbehavior, low intelligence, or lack of
effort. These misguided and damaging perceptions should be recast in a more
positive and hopeful light, so patients can begin to rebuild their self-confidence
and believe that successful treatment is possible. As a consequence, patients
will ideally be in a better position to break out of the shackles of feeling
stuck, demoralized, and chronically frustrated.”
Demoralization
Upon
receiving the diagnosis, some adults with ADHD experience temporary
demoralization or dysthymia. That is because, after all, it is a chronic
disorder that has no quick cure such as an antibiotic that may treat a
transient infection. No advice, therapy, or drug to date gets rid of ADHD
permanently, even if it can be managed quite effectively. Clinicians can
therefore understand why the diagnosis might be at first disheartening to the
client. As Dr. Kevin Murphy has written:
“Most adults with
ADHD have suffered years of feeling demoralized, discouraged, and ineffective
because of a long-standing history of frustrations and failures in school,
work, family, social, and daily adaptive domains. Many report a chronic and
deep-seated sense of underachievement and intense frustration over squandered
opportunities, and are at a loss to explain why they cannot seem to translate
their obvious assets into more positive outcomes. Furthermore, many
report having heard consistent complaints about themselves from parents,
teachers, spouses/partners, friends, or employers. Such complaints focused on
their behavioral, academic, interpersonal, or productivity shortcomings. The
cumulative effect of such a history can sometimes lead to feelings of intense
frustration and demoralization, and to a sense of anticipating failure as the
predictable outcome of their efforts. Sadly, some appear so wedded to this
belief system that they eventually give up believing life could be different
for them. Many are completely unaware that their condition is a highly
treatable one.”
What
other reactions might clinicians see in the adult with ADHD immediate following
a professional diagnosis of ADHD?
Anger
Many
adults, upon learning of the diagnosis, may react with anger and frustration
for various reasons, as noted above. Not the least of these is the long delay
to finally receiving the appropriate diagnosis for their problems, especially
if they have sought help previously only to be told they had a different
disorder or no disorder at all. Anger can also arise from learning that their
condition is quite treatable and thus many of the harms that have befallen them
earlier in life might have been avoided had a knowledgeable clinician diagnosed
and managed their ADHD properly.
Sadness
or Loss
Other patients, upon their diagnosis, show a mixture of both sadness and anger
because of previous adverse events they have experienced that likely stemmed
from their disorder. The sadness comes from recognizing that some of these
adversities cannot be repaired. These irreparable harms might include lost
relationships or marriages, visitations with or custody of their children after
an acrimonious separation or divorce, lost education and related opportunities,
lost jobs and other employment opportunities, previous drug abuse and its
consequences, and even previous arrests, jail time, or related harms caused to
victims of their previously impulsive and even anti-social activities.
And
then there are the many social relationships such as friendships that fell
victim to the individual’s inappropriate ADHD behavior. Those relationships may
be difficult or impossible to re-establish or reclaim. The list here could be
nearly endless, but the point is that many adults come to realize that even now
that they have the proper diagnosis and a treatment plan, little can be done
about some of the past irreparable harms that have occurred because of their
previously undiagnosed ADHD.
A
Grief Reaction
All of the above are actually part of human grieving. So it is understandable that adults with ADHD may show a grief reaction when they first receive a diagnosis of ADHD. They are grieving what has been lost and may not be recovered. Yes, there is some relief in knowing what the core problem is and what can be done about it. But there is also a profound sense of loss as to adversities and harms that have befallen them in the past that didn’t have to be that way if only they had been diagnosed and treated earlier. This sense of loss for what might have been may be so strong a grief reaction that it requires counseling sessions with a clinician in order to assist them in understanding, venting, and resolving these reactions.
Also, the grief reaction that adults diagnosed with ADHD may experience may cause them, out of desperation, to try any quack remedy they may have heard about on the Internet or from other sources. They may start to think with their grief and not with their brain. That means they may look for promises of quick cures rather than the evidence-based treatments that do not make such promises but are more likely to be effective in the longer-term.
Clinicians can help adults with ADHD negotiate and resolve many of these reactions by simply being a sensitive listener to those reactions. Acknowledge that one understands how they can feel that way, thus legitimizing the feelings. Sympathize with the unfairness of it all – that it had to take this long to get the right diagnosis and treatment – then encourage them to move past such grief responses to a healthy acceptance of the disorder. Hopefully, after the catharsis and exorcising of past regrets comes an acceptance of their condition. With that acceptance or ownership of the disorder, they can adopt a more forward-looking perspective of hopefulness, based on the knowledge that ADHD is highly treatment-responsive and that one’s future does not have to look like one’s past.
Helping the Client Understand and Accept Their Diagnosis
Over
years of working with adults with ADHD, we have learned that this next step is
a crucial one – it is all about the attitude adults with ADHD adopt toward this
diagnosis. Unless they develop an attitude of “owning” their disorder,
accepting the diagnosis for what it means, and then becoming educated about the
condition, they are not likely to accept treatment for it. Even if they are offered
treatments, they may not be likely to cooperate fully with the treatment plan.
In
that sense, ADHD is like diabetes. It is a condition whose symptoms can be
managed quite effectively on a day-to-day basis, yet the underlying cause of
those symptoms cannot be easily corrected or cured, if at all. The goal of
treatment then is essentially the reduction of any possible harm that might
come to adults with ADHD if their disorder is not managed well. It is to reduce
the risks they may experience for various adverse consequences that are likely to
occur if the disorder isn’t treated. Those harms can include all the areas of
impairment discussed in earlier sections (i.e., work, education, family life,
driving, etc.).
From
this point of view, ADHD must be managed on a daily basis if those secondary
consequences are to be prevented or at least reduced. That means treatment can
go on for years, just as it does for diabetics. Yet, like people with diabetes,
adults with ADHD can lead a relatively normal and fulfilling life when their
disorder is well managed. Fully engaging in this sort of ongoing or continuous
treatment, at least as needed, requires that a person first accept that they
have a chronic condition. They must first adjust their attitude toward
themselves and incorporate the diagnosis into how they personally view
themselves and what that means for getting help for it.
The adult with ADHD will need to own it, then learn about it, and lastly deal with it. Absent such acceptance, it is unlikely that anything further can be done to help them manage their disorder. Following acceptance, they must then learn as much as they can about this condition and hopefully that will lead them to be able to manage their disorder as best they can. These are things that no one else can do for them. The adult with ADHD must reframe their view of themselves and their life if they wishes to actually take charge and manage, if not master, their ADHD.
The extent to which ADHD may disable an adult is directly related to the environments they place themselves into and what changes they make in their surroundings (accommodations). It is also related to the kind of people they choose to be surrounded by and how well (or poorly) those people contribute to the adult’s impairments, either by worsening or improving them. The degree of the impairment the adult with ADHD experiences is also related to the resources they may have available and how well they use them.
Understand that while disorders belong to people, handicaps belong to situations. Change the situation well enough and a person can reduce or eliminate the degree to which they will be handicapped or disabled within a disorder. However, that willingness to modify settings so that one is less handicapped by their disorder first requires that the person accept that they have a disorder. The adult with ADHD has to own it!
Some
clinicians have worked with adults with ADHD who could acknowledge the disorder
at some detached intellectual level. They could even sit through counseling
sessions nodding their head in recognition of what was being said. But in their
head, in their personal life, in that inner sanctum of their mind where we hold
our self-image, they didn’t “get it.” These adults had not really owned the
disorder at all. They paid lip service to the diagnosis but privately denied
that this disorder is really a part of their self-image. So the adult with ADHD
might adopt some intellectual understanding of the information about ADHD but
not take on the entire package of the disorder or even accept that it is a disorder.
When
adults with ADHD accept their disorder and truly come to own the diagnosis, it
is not demoralizing at all – in fact, it can actually be
liberating. They come to understand that they are not dumb or stupid as many
had come to believe. The cloak of demoralization and moral self-criticism is
lifted, making them free to better understand the struggles of the past. They
also no longer have to play mind games with themselves or others in which they
deny, excuse, defend, distort, massage, or in other ways avoid accepting the
disorder, what it is, and what it means for their life.
Acceptance and Ownership Do Not Mean Making Excuses
It
is important to recognize here that owning the disorder does not mean using it
to make excuses for one’s inappropriate behavior. A diagnosis of ADHD does not
mean one is allowed to engage in violations of social etiquette, or even laws,
and claim not to be responsible – “it was my ADHD that did it!” Nor does it
mean committing various criminal acts or becoming drug dependent or a drug
abuser and then claiming it could not be helped – “it was my ADHD that did it.”
The diagnosis of ADHD provides an explanation but not an excuse. It can help
clinicians and the adult with ADHD understand why they may be having
difficulties behaving in a less-than-optimal or frankly inappropriate way. But
it does not excuse such behavior, especially from its consequences.
The
diagnosis is a means to motivate one to come to understand their ADHD and to
accept the diagnosis for what it represents in one’s life. It does not provide
carte blanche to behave in any unacceptable way one wishes while excusing the
conduct and its consequences. Clinicians must understand that to have adult
ADHD is not to be a victim whose circumstances are to be dealt with by
eliminating all accountability for one’s actions or to excuse one from doing
anything about the problem. The result of such an approach could be disastrous.
Becoming Educated About Adult ADHD
After adults with ADHD adjust to their initial reactions to the diagnosis, and then come to own the diagnosis as part of their identity, the next step in helping them build a treatment program is to help them learn as much as they reasonably can about ADHD, the condition, and its management. Clinicians can suggest books and videos to help the adult with ADHD improve their knowledge. Some of these are listed in the Resources section at the end of this course. Encourage the adult with ADHD to read widely, watch videos (I have many available on YouTube), listen to (and even talk with) other experts, ask questions, visit the most informative websites (also listed in the Resources section), follow up on what interests them, and pull together as much information about ADHD as they have time to do.
As
the author David Lindsey once wrote, “truth is an assembled thing!” It
comes from no one book, source, expert, guru, video, or website. The more
widely clinicians pursue information, the more likely clinicians and the adult
with ADHD are to be able to distinguish the knowledge that is most reliable and
trustworthy from that which is fashionable, flimsy, baseless, or outright false
or misleading. There is much reliable science-based knowledge about adult ADHD.
Yet there is also much nonsense, misinformation, and blatant propaganda that
one needs to filter out as unreliable, unrepresentative, and even intentionally
misleading.
Be
skeptical. Especially, beware of the Internet. It can be both a blessing and a
curse in finding information about any disorder. If one enters ADHD into a
browser, you will get millions of “hits.” Yet only about 10-20 websites offer
truly accurate, science-based information. Many of these are listed in the Resources section. Look for what seems to be the consensus of the clinical and scientific
experts who specialize in the disorder. If the adult with ADHD really wants to
read the science behind any specific topic related to ADHD, then do not have
them use a general browser like Google, FireFox, or Safari. Use Google
Scholar – a browser that searches just the scientific journals and
textbooks for what is known on that topic.
Evidence-Based Therapies
The
following therapies have a sufficient body of evidence supporting their
effectiveness in the scientific literature so as to consider them for routine
use in the management of adult ADHD (Ostinelli et al., 2025; Yang et al., 2025). That said, all treatments, including
psychosocial ones, are associated with adverse events. These may arise from the
mere fact of human diversity, unusual patient characteristics or comorbid
disorders which may be exacerbated by these therapies, from incompetence or
misapplication by therapists, or from misunderstanding and misapplication by
clients. For an excellent discussion of these issues, see the articles on the
side effects of these therapies in the March 2018 issue of The ADHD Report (Guilford Press, www.Guilford.com).
General Counseling
An important step involved in treating an adult with ADHD after they have been properly evaluated and diagnosed is to make sure they are well educated about the disorder, its true nature, causes, risks, and both the general management principles reviewed earlier as well as the treatments set forth below. Adults
with ADHD can’t fully benefit from or participate in treatment of their
disorder if they are not fully aware of the broad knowledge that exists about it.
Counseling them about ADHD serves that important purpose. Self-education
through trade books, the Internet, and other sources is fine, but many adults
with ADHD often choose to also receive one or a few sessions of general
counseling with a mental health professional knowledgeable about the disorder.
This can help them get more fully educated about it and have their specific
questions about their own unique case answered. Accessing a knowledgeable and
trusted professional can usually provide reliable information about the
disorder quickly, without the need to sort through the myriad information,
points of view, and even propaganda about the disorder available through other
sources such as the Internet.
Apart
from conveying such information, short-term counseling with a professional can
often help to address some of the phases of grieving or adjustment to the diagnosis
discussed earlier that may have arisen since the adult with ADHD received their
initial evaluation. Some of those reactions can be serious enough to warrant
working through them with a competent professional instead of struggling with
them on one’s own.
Along with the need to maintain a realistic picture of adult ADHD, there remains the equally, if not more important, attitude of instilling hope that things can be improved. Absent such hope, there is little likelihood that the adult with ADHD is going to undertake the various treatment programs and coping strategies that are necessary to successfully manage this disorder and its associated impairments. They must come to feel that getting treatment has a high likelihood of improving the quality of their life, which it does. They also need to know that people close to them sincerely believe that they can benefit from treatment. And they need to know that supportive others may even opt to be their partners in that treatment process, if possible, to help them to be more likely to engage in it and benefit from it. Counseling can inspire hope while also tailoring general information on the disorder to the client’s specific case.
Although
such counseling sessions are generally offered as a short term course, additional
sessions may be needed periodically as new problems or impairments arise, new
issues come to the fore, or symptoms break through from being effectively
managed. All of these situations may require readjustment of the treatment
components, such as medications, to deal with them. Such counseling may also
serve as a central hub for the other components of the treatment package needed
to manage an adult’s ADHD. For instance, the therapist can help in:
- arranging
for a vocational assessment and consultation on occupational problems,
- referring
the patient to an expert psychiatrist or other medical specialist for
consideration and management of their ADHD medication,
- consulting
with college student disability services on ADHD accommodations in that
setting,
- getting
appropriate couples counseling with a knowledgeable marriage counselor, and
- locating
appropriate individual, group, and medical therapies for substance use
disorders.
Professionals
and even adult ADHD coaches can also assist the adult with ADHD in applying the
general strategies for coping with ADHD from the perspective set forth earlier
of adult ADHD as a disorder of EF. (Also see later sections of this course.)
Further advice on how best to cope with working memory problems and
forgetfulness, poor impulse control, organization and problem-solving,
emotional self-control, as well as time management may all be provided by this
counselor. Or the counselor can arrange for a consultation with someone more
expert in cognitive behavioral therapy that focuses on the executive deficits
associated with adult ADHD.
Help
the adult with ADHD identify not just problematic behavior and impairments and
what to do about them, but also the positive qualities and assets they may
have. Those assets can be brought to bear to either help deal with problems or
help offset the adverse consequences or demoralization one may experience from
them. Skilled therapists can help offset or counterbalance any negative
self-perceptions, promote greater self-acceptance, and reinforce strengths,
talents, and other qualities as needed for adults with ADHD. And certainly, if
there are comorbid psychological disorders co-existing with the ADHD, these may
require their own separate psychological or medical treatments that can be
provided by or arranged through the general counselor/therapist.
EF-Focused Cognitive Behavioral Therapy (CBT)
One
of the best scientifically investigated non-medical treatments for adults with
ADHD to date is Cognitive Behavioral Therapy (CBT), a widely used therapy
modality for various disorders including anxiety, depression, post-traumatic
stress disorder, substance-use disorders, and personality disorders among
others. This method of therapy has now been specifically adapted for adult ADHD
and targets the adult’s deficits in executive functioning, among other
ADHD-related symptoms and can even be delivered by virtual, internet means (Zhang et al., 2025). Traditional CBT helps a patient identify inappropriate
or maladaptive thoughts and associated negative emotional reactions,
environmental triggers for such unreasonable or irrational thoughts and emotions,
and ineffective behavior that may flow from or exist in conjunction with them,
and then suggests various ways to correct them. These suggestions typically
focus on helping patients modify or avoid problematic settings. It also helps
them learn to refocus their attention to less emotionally provocative aspects
of the setting. And it especially teaches them to rephrase and reframe
inappropriate thoughts and conclusions to more rational and constructive ones.
Some CBT methods also teach adults to self-soothe and otherwise cope with
negative emotions, construct more appropriate coping strategies, and reduce or
prevent inappropriate actions. Therapy can also teach an adult how to
substitute more constructive behaviors that may flow from the problem situation
and from the patient’s thoughts about and reactions to it.
For
adults with ADHD, CBT goes even further than this traditional paradigm. It
strives to identify problematic behavior and thoughts and to substitute more
specific coping strategies for the express problems these adults have with
self-restraint, time management, self-organization, problem-solving, emotional
self-control, and self-motivation, among others.
Professional
manuals on these methods for therapists are now available at major booksellers,
such as those written by Mary Solanto, Ph.D., Steve Safren, Ph.D., and J.
Russell Ramsay, Ph.D. The next three diagrams summarize the basic essential
features of these treatments.
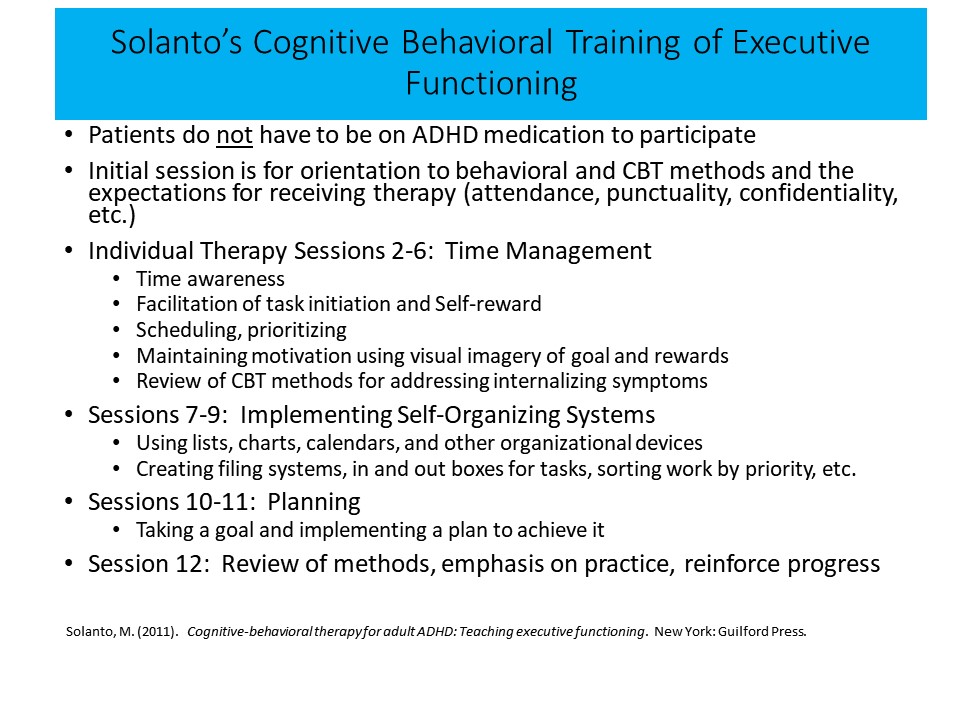
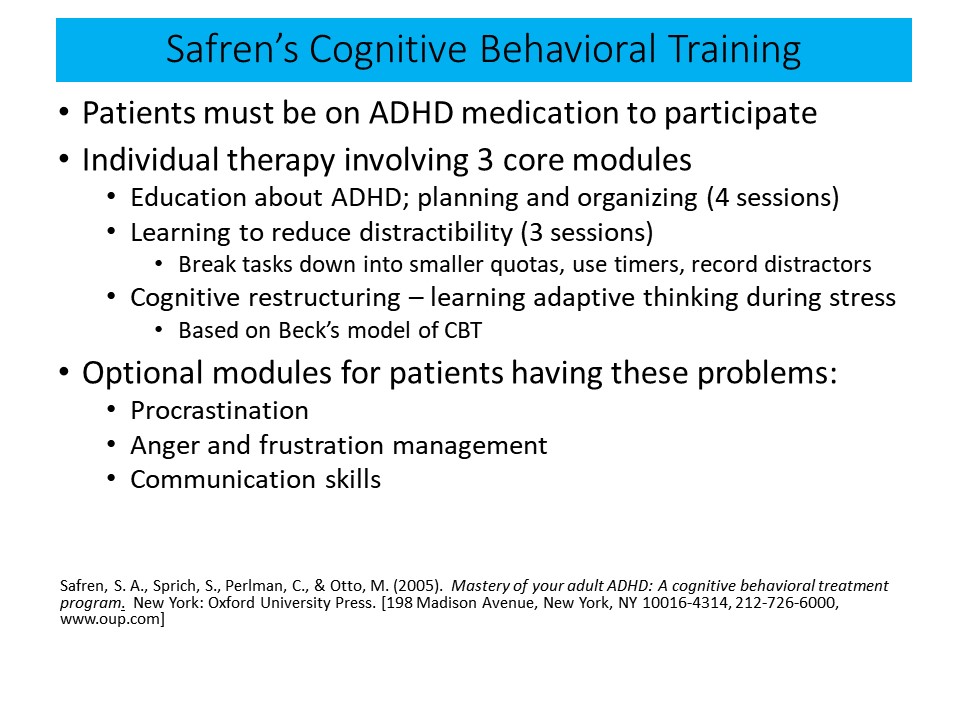
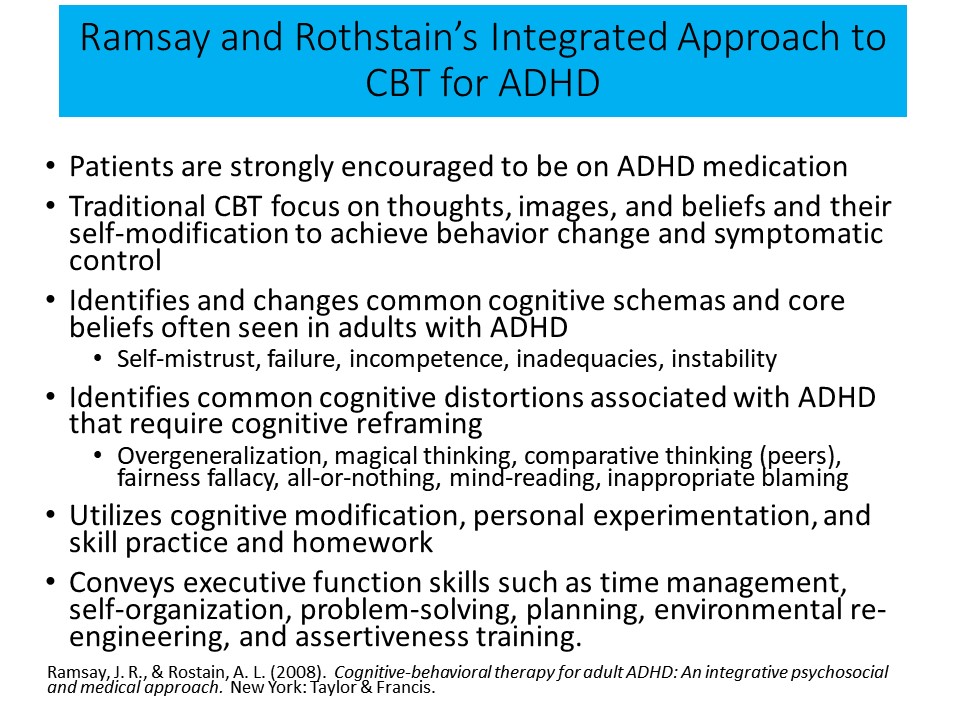
Trade
books for adults with ADHD also provide advice on these strategies, such as
those by Ari Tuckman, Ph.D., Craig Surman, M.D., Tom Brown, Ph.D., Lenard
Adler, M.D., Edward Hallowell, M.D., and myself. (See Resources at the
end of this course.)
It
is important to appreciate that these therapies are not an alternative to or
replacement for the ADHD medications discussed later in this course. Most
adults with ADHD benefit most from these therapies if they are also taking their
ADHD medications while they participate in CBT. The medications are usually
more effective than CBT alone, but using CBT with medication can further
improve the treatment response of the typical adult with ADHD (Ostinelli et al., 2025).
Knouse
(2015) has critically reviewed these and other forms of CBT for adults with
ADHD for their evidence base and effectiveness and also has a meta-analysis of
all of the studies (2017). he concluded, as he had done in an earlier
qualitative review in 2010, that the results of research support the
effectiveness of the forms of CBT adapted for adult ADHD in augmenting the
effects of ADHD medications and in reducing symptoms, EF deficits, and
impairments, whether in comparison to no-treatment wait-list control groups or
to more active therapies, such as psychotherapy or meditation. These
conclusions were echoed in another review of this literature in 2012 by Mongia
and Hechtman, who likewise concluded that CBT for ADHD
significantly improved functioning, particularly when combined with medication,
and augmented the effects of the ADHD medications. A more recent, large study
comparing medicated adults with ADHD receiving treatment as usual with those on
medication who also received CBT for adult ADHD, documented significant effects
on ADHD as well as some improvement in comorbid disorders over a more extended
follow-up period.
In a recent development, CBT for adults with ADHD has now been adapted by Will Canu, Laura Knouse and colleagues for application to the college population with ADHD. The program involves both a clinicians manual on how to implement the program (Canu, et al., 2023) and a workbook for students to help promote adoption of the strategies for addressing EF problems in the university setting (Knouse, et al., 2023).
Coaching
Another approach to helping adults with ADHD is Coaching; the adaptation of the life-coaching therapy modality to the specific needs of adults with ADHD. One general approach to Coaching is shown in the figure below for illustrative purposes.
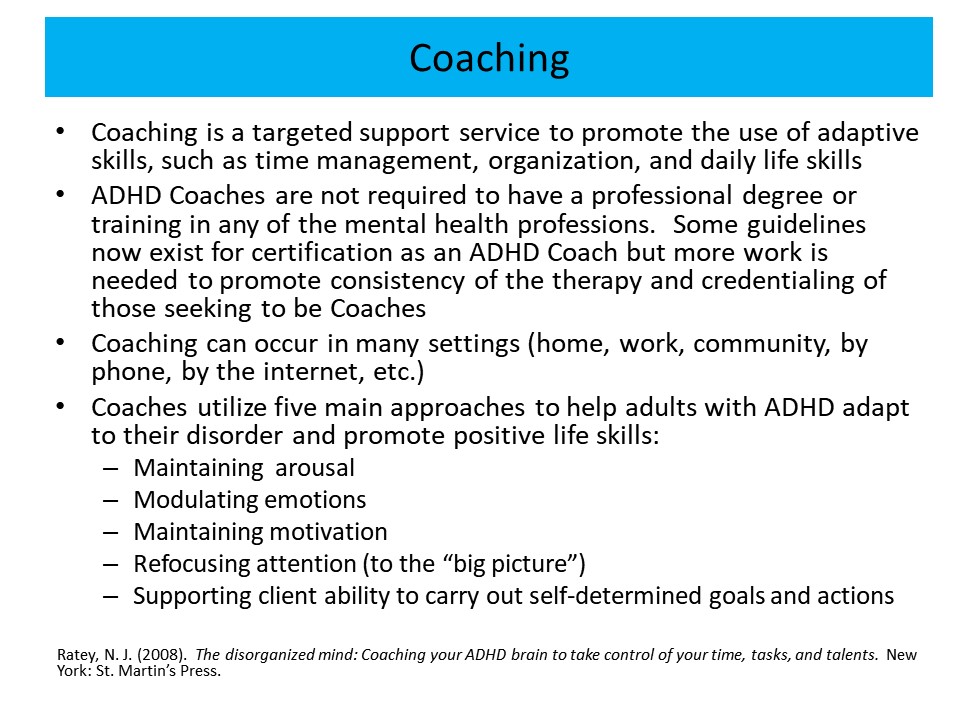
Coaching
typically involves providing an ongoing professional relationship that focuses
on the adult with ADHD taking action toward the realization of their vision,
goals, or desires. It uses a process of inquiry and personal discovery to build
ADHD clients’ levels of awareness and responsibility, to help them develop new
skills, and provides them with structure, support, and feedback. Like the
general counseling or therapy discussed above, Coaching is a supportive,
pragmatic, educational, and collaborative process. But it differs from
traditional general counseling in that a coach is in much more frequent contact
with an adult with ADHD, often several times each week. This is typically
accomplished using means of communication other than face-to-face sessions,
such as telephone calls, emails, text messages, and other social media. Contact
is usually accomplished using daily or less-frequent 10- to 15-minute telephone
conversations. These calls serve to identify goals, and strategies to meet
those goals, as well as providing compassionate, constructive, and otherwise
supportive advice to the ADHD client. Coaches can also provide the structure,
accountability, and at times gentle confrontation that may be needed to address
the Executive Functioning deficits noted above, typically by giving many of the
same suggestions given earlier about dealing with EF deficits. Murphy and
colleagues (2009) described several cases in which Coaching was used to assist
clients with adult ADHD.
A
small amount of research has been done to date on this therapy. It suggests
some promise as a standalone modality or as an adjunct to the ADHD medications
discussed in the next section. However, the studies to date are few in number,
of a small sample size, are less rigorous in methodology than is desirable, and
many concentrated on college students. Thus, while initial results are
promising, more research of a more rigorous nature with clinic-referred adults
with ADHD is needed to properly evaluate the utility of this therapy.
Professional associations now exist to provide training and guidance to
professionals who wish to practice Coaching with adults with ADHD.
More
information on this treatment approach can be found on the Internet. ADHD
Coaches can be located through several websites, including totallyadd.com. Be
aware that there is no licensing at the state or national level, nor is there currently
any credentialing or certification for adult ADHD Coaching that has been widely
adopted by the field. But that is changing for the better as professionals in
the Coaching community develop a consensus on what training is essential in
order for one to become an ADHD Coach. For now, understand that Coaches can
vary markedly in their educational background and depth of training about ADHD
and mental health services. Clinicians are cautioned to investigate the quality
and education of any Coaches the adult with ADHD may be considering employing,
just as clinicians would do with any other unlicensed services.
Medication Management
ADHD medications are the most effective treatments currently available for managing ADHD in adults. Period. No other approach to managing ADHD in adults results in as much control of the symptoms and executive deficits, as much improvement in the adverse impact of ADHD on major life activities, for as many people and in such an economical way as medication management of ADHD.
ADHD medications:
- Have a sizable evidence base for their effectiveness.
- Offer a window of safety that is incredibly well established.
- Improve 70%–90% of clinical cases, normalizing 50%–60% of such cases.
- Are convenient to administer.
- Provide an alternative when psychosocial treatments produce side effects, don’t work, or don’t work well enough.
- Are less expensive than psychosocial methods of treatment.
- Can be used for years, even into and across adulthood.
- Are active in community settings where no caregivers may be present to provide active psychosocial treatment (unsupervised activities, driving alone or with friends, free time in schools, bus rides, etc.).
- Reduce symptom severity and associated executive/self-regulatory deficits.
- May reduce family stress, parent-child conflict, adult-partner conflict.
- Reduce risks for of impairments in major life activities (home, school, peers, community).
- Reduce risks for some health-related problems (obesity, injuries, substance use, etc.).
- Reduce risks for some comorbid disorders, both externalizing (oppositional, conduct) and internalizing (anxiety, depression)
- Reduce economic burden to family and society.
- May offer the possibility of neuroprotection, (technically, neuro-enhancement) over time. (See discussion below.)
So if adults with ADHD opt not to use medication to master their ADHD for whatever reason, understand that they have just declined the most effective treatment currently available to deal with the disorder. It is a choice that is equivalent to a Type 1 diabetic choosing not to use insulin while trying to make a go of it in dealing with their diabetes strictly through diet, more exercise, and better hygiene. Maybe that will work, but it is much less likely to do so than would medication. And it will result in far less control of the disorder than using medication to manage it.
In
my experience and that of many of my expert colleagues, adults with ADHD who
choose not to try medication following their diagnosis typically return within
three to six months asking to go on it. That is because most come to realize
that all of the other options they’ve tried are not addressing their problems
very well. I am not saying here that some adults with ADHD cannot manage their
disorder without medication. Some can. This is likely the case for those adults
with marginal or mild symptoms of ADHD, who have no other psychological disorders,
who are otherwise healthy, maintain good nutrition, avoid abusing nicotine,
alcohol, and other drugs, exercise regularly, and who have made a number of
lifestyle modifications to permit them to function satisfactorily despite their
ADHD symptoms. These adults may be able to get by without medication. I applaud
them for doing so. But understand, these people are not representative of the
majority of adults with the disorder.
While
I recommend using medication, it should not be advocated as the only treatment
approach. There are many other methods that clinicians can use to assist
clients in mastering their ADHD, such as those discussed above. But for the
majority of adults with ADHD, especially those with moderate to severe
symptoms, medication management should be the core component around which to
build the other treatments – just as in managing diabetes. Those other
treatment methods will be designed to address what the medications are unable
to change or improve sufficiently so as to reduce the client’s ADHD-related
impairment in any particular area of their life. But those treatments can
rarely do it alone without being combined with ADHD medications.
In
addition to the practical fact that medications work and work well for most
people with ADHD, there is another reason they are so important for managing the
disorder. Research over the past decade has shown that the medications actually
help to either correct or compensate for the underlying neurological problems
that are likely contributing to the ADHD in the first place. Indeed, in
children who remain on the medications for several years, brain regions may
develop more similarly to those of their peers without ADHD.
These
medications control symptoms only temporarily. That control lasts only as long
as the medicines are in the blood stream, and hence in the brain of the adult
with ADHD, but they do work. We now know that ADHD medications can normalize
the behavior of 50%-65% of those with ADHD. And they result in substantial
improvements, if not normalization, in another 20%-30% of people with the
disorder. In other words, less than 10% of people with ADHD will not have a
positive response to at least one or more of the ADHD medications currently
available in the U.S.
When
the medicines work, they can result in substantial improvements in the symptoms
of ADHD. Those improvements are, on average, two to three times greater than
those seen with any other psychiatric medications used to treat other
psychiatric disorders, such as anti-depressants and anti-anxiety medications.
And that improvement in ADHD symptoms is likely to lead to significant
improvements in the downstream impairments in major life domains that are due
to those symptoms.
The various FDA-approved medications for ADHD are shown in the Appendix in Table 1. There
are two basic categories of ADHD medicines that are approved by the FDA for use
with adults – stimulants and non-stimulants. Both have to be taken
daily. As noted above, they all control the symptoms of ADHD only as long as
the adult with ADHD takes the medications. They produce no enduring positive
effects on the client’s ADHD once clinicians stop prescribing them. Ceasing the
use of medication often results in a return of the ADHD symptoms back to their
pre-treatment levels.
Both
types of ADHD medications typically work by increasing the amount of two (or
more) chemicals in the brain known as neurotransmitters. Those chemicals are
involved in permitting nerve cells to communicate with each other so the brain
can function effectively. More specifically, these drugs increase just how much
of these chemicals are residing outside of the nerve cells. That can increase
the activity of adjacent nerve cells. The two neurotransmitters are dopamine
and norepinephrine. By causing nerve cells to express more of these
neurochemicals, or by keeping the nerve cells from pulling these chemicals back
into the cell once they have been released, the drugs increase the
communication that occurs between nerve cells in regions of the brain that are
related to directly causing ADHD. In short, increasing these brain chemicals in
these regions lets that brain area function better and sometimes normally.
For
a detailed discussion of FDA-approved medications for use with adult ADHD in
the U.S., readers should consult the chapter by Dr. Jefferson Prince and
colleagues at Massachusetts General Hospital in my professional handbook on
ADHD (see Resources).
Stimulants
There are two basic types of stimulants currently marketed in the U.S. –
methylphenidate (MPH) and amphetamine (AMP). These stimulants act in the brain
to mainly increase the amount of dopamine available for use outside the nerve
cells. Yet they can, to a smaller extent, increase the amount of norepinephrine
outside the nerve cells as well. AMP does this mainly by increasing the amount
of dopamine that is expressed from the nerve cell when it is activated. To a
lesser extent, it may also block the transport system by which the dopamine is
normally re-absorbed back into that nerve cell after being released. That can
result in more dopamine being left outside the cell to continue to function.
MPH mainly acts by preventing the re-absorption of dopamine. That is why it is
known as a transport or re-uptake blocker.
Both
AMP and MPH have the potential to be abused because they increase dopamine in
regions of the brain known as reward centers. Stimulating those centers can
lead to an increased likelihood of addiction to drugs that do so. But ADHD
medications are very unlikely to do this when taken by mouth and swallowed, as
prescribed. They certainly can do so when they are sniffed through the nose as
a powder or injected into a blood vein in a solution, such as when mixed with
water. Because of this potential for drug abuse, the Drug Enforcement
Administration in the U.S. has classified the stimulants as Schedule II
controlled substances along with other potentially addictive drugs. This
classification places limits on how much of the drug can be produced annually,
how the drug is to be prescribed, how it is to be stored in pharmacies, and how
it is to be dispensed and otherwise monitored in the U.S.
There are up to eight different methods by which these two drugs are delivered into the body. They are described in the Appendix (Table 2) to this course. A liquid form of both of the stimulants is also available for children or adults who do not wish to swallow tablets or capsules and, more recently, a chewable form of AMP has come on the market that dissolves on the tongue without a need for water. The various methods also differ in how long they maintain the level of the drug in the body, and so in the brain. There are hundreds of studies on the safety and effectiveness of these stimulants and delivery systems.
The stimulants work primarily by increasing the action of certain neurochemicals that occur naturally in the brain. The way the brain handles information is based on how these chemicals that are produced in the brain cells (neurons) are released from them to communicate with (influence) other nerve cells nearby. Although we don’t know all the neurochemicals that are influenced by the stimulants, we do know that two of them are dopamine and norepinephrine. Both occur naturally throughout the brain but are concentrated very heavily in the prefrontal executive function regions and related brain areas and networks, which we believe may be one of the primary sites causing the problem in ADHD. By increasing the amounts of these chemicals that are released from nerve cells into the intercellular space or by keeping the released chemical there longer, the stimulants increase the action of these brain cells, which seem to be those most responsible for inhibiting our behavior and helping us use self-control.
Evidence from functional neuroimaging and studies of brain functional connectivity suggest that the stimulants activate both blood flow and electrical activity in areas of the brain that create goal-directed, task-oriented behavior, such as the EF networks, and enhance the stimulus or reinforcement (interest) value of these goals and tasks, probably through increased activity in brain reward circuits and regions (e.g., nucleus accumbens and ventral attention/reward networks). They may also achieve some of their effects by decreasing activation in brain areas that are subject to task-irrelevant distractions.
Therefore, it’s not surprising that an abundance of research shows these medications to be effective at the rates noted at the beginning of this section. If each of these stimulants is tried in succession, it is estimated that up to 91% of people with ADHD will respond to at least one of them. There are some cases in which medication alone is enough or is the only practical way to address the concerns a parent may have about a child. For most cases, though, the greatest benefit of stimulant neurogenetic therapy seems to come from a combination of these agents with other psychological and educational treatments, or in rarer cases, with other medicines.
Effects on Behavior and Emotions
Unquestionably, the stimulants produce positive effects on sustained attention and persistence of effort to work. The medicines also reduce restlessness and gross motor activity in children. In many cases, children's attention to assigned work is so greatly improved that their behavior appears normal. Most people taking the medicine are far less impulsive and have fewer problems with reactive aggression and impulsive emotions, noisiness, noncompliance, and disruptiveness. However, 5%–10% of cases may experience an increase in mood lability, dysphoria, anxiety, hostility, or explosive outbursts. Overall, the drugs improve an individual’s EF deficits and with it the capacity for self-regulation. Effect sizes (degree of improvement measured as a proportion of a standard deviation) for the stimulants range from 0.57 (MPH) to as high as 1.52 (AMP), which puts them among the largest documented in drug research in psychiatric medications. For instance, effect sizes for antidepressants or antianxiety medications are typically in the range of 0.3 to 0.4. Meta-analyses show that longer-acting stimulant formulations produce larger effect sizes than immediate-release versions.
For most comorbid conditions, however, the stimulants remain useful for ADHD management without typically exacerbating the comorbid disorder. However, in some cases, such as ASD, ID, OCD, tic disorders, and seizure disorders, side effects may be somewhat more common and response rates may be somewhat lower than the typical 75% response rate, or the degree of improvement (effect size) may be less than for non-comorbid cases or cases having comorbid ODD/CD. That said, there is some evidence that small minorities of patients with ADHD and comorbid anxiety, tics, or OCB may have those symptoms exacerbated by stimulants or, as in the case of anxiety, some cognitive toxicity (on working memory) might become evident. In other comorbid instances, doses may need to be somewhat higher, such as in comorbid ODD/CD.
Learning and Academic Performance
Numerous studies have been conducted on the effects of stimulants on intellect, memory, attention, and learning besides general behavior. The studies show that the stimulant medicines are very likely to improve attention, impulse control, fine motor coordination, reaction time, working memory, sense of time, and planning and problem-solving abilities on a variety of objective measures and even more on ratings of ADHD symptoms and EF deficits in daily life. When those with ADHD must perform learning tasks, the medicine seems to help them (a) be available for such learning if they are acquiring new information, and (b) perform more efficiently what they already know and in a more organized manner, with less task-irrelevant activity. Neurogenetic therapies especially result in those with ADHD being more productive (getting more work done), that is goal-directed. No medicine can actually improve intelligence or knowledge, but the stimulants increase the ability to show what one has already learned. And used over several years, that improvement in productivity and availability to learn new material does translate into improved academic knowledge (achievement) in the case of young adults. In general, the drugs produce their greatest influence in situations that require self-control, restriction of behavior to situational demands, and concentration on assigned tasks – situations like school and work.
Social Behavior
Treatment with stimulant medication has been found to reduce the intensity and improve the quality of social interactions between people with ADHD and others. Stimulants increase the ability to comply with instructions or commands and to maintain that compliance over time. The medicines also reduce behavior that competes with getting work done, such as inattention, distraction, restlessness, mind-wandering, and forgetfulness. In turn, others, such as parents, teachers, partners, or employers respond by reducing their level of control and their degree of supervision over the person with ADHD.
The degree of improvement differs among clients, and each should be expected to have a unique response. We are all unique individuals including in our brain functioning. Researchers have not seen important differences between males and females in their drug response, although one study suggested that females may experience optimum improvement from their daily dose somewhat later into the day than do males. Clinicians should expect to see greater improvement in ADHD symptoms and the EF-SR aspects of social behavior with moderate or higher doses but will have to try each client on several different doses before discovering which one is best. Even then, they may also have to try more than one drug or delivery system.
Brain Development and Functioning
Over the past decade, more than 33 studies have been published on the longer-term effects of stimulant treatment on brain development and functioning (see reviews by Frodl and colleagues in 2010, Spencer and colleagues in 2013, and specific research by Schulz and colleagues, and Ivanov and colleagues in 2014, and Moreno-Alcazar and colleagues in 2016 in the References). These studies document a quite surprising finding that is unreported by the popular media. Longer-term stimulant treatment may promote brain growth and connectivity in the very brain regions from which ADHD symptoms are known to arise – cortical gray matter, subcortical basal ganglia, and cerebellar regions.
While this usually requires several years of treatment, it has been noted most often in studies of children. But a more recent study with adults found similar results. It is not clear how long one needs to be on these medications to see these effects, what doses are optimal to produce them, whether one stimulant is better at doing so than another, and other important clinically relevant details. It is also unknown if the nonstimulants, like atomoxetine, have similar effects on brain growth. But given that the regions of the brain that this drug affects overlap by 70% or more with the regions in which stimulants are active leaves that possibility open.
These findings are robust enough to withstand a meta-analysis or two. Evidence to date suggests that this may occur only in a minority of cases (about 25%–40%), and it is not clear why they and not other cases of ADHD see such results. Fairness dictates that I convey that there is some skepticism among a few neuroimaging experts such as Katya Rubia, who remained unconvinced that the effects are real and not due to some methodological factors common to such naturalistic studies (cases are not randomized to active or placebo medications and followed over time). Future research will untangle all this, but for now they remain one of the more exciting findings in the neuroimaging of drug effects.
Duration of Drug Effects
Just how long drug effects last depends on the type of medicine and the preparation or delivery system being used to get the drug into the body and bloodstream. Regardless of how they are delivered into the body, these medications are swiftly absorbed into the bloodstream and cross into the brain quickly and easily. They are also largely eliminated from the body within 24 hours. This means that if someone has an undesirable reaction, it will usually last only a few hours to a day. But it also means children and teens must take this medication at least once daily every day to get its benefits.
The older immediate-release forms of these medicines, such as the pills Ritalin or Dexedrine, act quickly (typically within 30–45 minutes) to enter the bloodstream and begin to change symptoms. They reach their peak in improving behavior within 1–3 hours. They may control behavior for 3–6 hours, but each person reacts somewhat differently, and each stimulant acts differently. Some changes in behavior are noticeable within 30–60 minutes after taking the medicine, again depending on which one is being taken. The problem with these immediate-release versions is that people with ADHD had to take them several times a day, including during school or work, and that caused a lot of problems, especially for schools.
Besides these immediate-release fast-acting tablet forms of methylphenidate and amphetamine (Ritalin and Dexedrine), both come in sustained-release preparations. These latter preparations reach their peak influence somewhat later than the fast-acting forms (usually in 3–5 hours) and may produce effects that last much longer (typically 8–12+ hours). Also keep in mind that amphetamines, such as Dexedrine and the newer compounds Adderall, Adderall XR, and Vyvanse, are nearly twice as potent as methylphenidate preparations such as Ritalin. As a result, they may produce greater changes in behavior and their effects may last an hour or two longer than methylphenidate preparations are likely to do. Of course, being stronger, they can also result in somewhat more side effects. For instance, some research suggests that AMP is more likely to exacerbate tics than MPH. Because the AMP variants are stronger or more potent than MPH, they are typically given in somewhat lower doses (usually half as much as Ritalin or generic methylphenidate) to avoid overdosing or excessive side effects.
Clinical Tips:
- Clients often ask whether they could develop a tolerance to stimulants so that the current dose becomes ineffective over time. Though some physicians have reported that a few people in their practice seemed to develop some tolerance (loss of effect) over a longer period of use (typically 3–6 months), research studies have not been able to document such an effect.
- If you observe that a dose is losing its effectiveness, has the adult gained weight since starting on the medication? Increased body mass would require you to increase the dose to get the same effects on behavior.
- Clients may also ask whether they will need to have regular blood tests to monitor the amount of the drug in the bloodstream. This is not a requirement for taking the stimulant medications. The amount of drug in the bloodstream does not seem to be related to how well it works to control behavior, so there is no need for such tests.
Stimulant Side Effects
Adults can experience various side effects when taking these medicines. The vast majority are minor, although some can be annoying. Keep in mind that if any of these are bothersome enough to warrant stopping the medication, they will likely go away once the medicine “washes out” of the body – within 24 hours typically. Most of these side effects are clearly related to the dose of medicine: higher doses produce more side effects.
Clinical Tips:
- Note that it has been estimated that 1%– 3% of people with ADHD cannot tolerate any dose of any stimulant medication.
- Ask clients if any of their family members have had an adverse reaction to the medicine you are going to prescribe for their child. It’s impossible to predict whether someone will have any of the side effects discussed here, but there may be a genetic basis to expect that a client might have a similar reaction to that experienced by a close biological relative.
The following pages describe the side effects your patients might experience with the stimulant medications. How likely are the specific side effects?
- Over half of people with ADHD treated with these medications show decreased appetite and insomnia. To a lesser extent mild stomachaches or headaches occur (about 20%–35%).
- Even fewer people (<10%) may experience increased anxiousness, irritability, or proneness to feeling sad or crying. However, many of these side effects (especially those associated with mood) were present when the clients took a placebo. This means that sometimes these side effects may represent problems that are associated with ADHD rather than with the medicine in some cases. In most cases, the actual side effects were less frequent than this and quite mild.
Decreased Appetite
All of the stimulants seem to reduce appetite to some degree – temporarily and mainly in the late morning or early afternoon, which explains why more than half of all people on these drugs may eat little of their lunch while on the medicine. This is what may cause them to possibly lose some weight if their calorie intake falls below normal. For many people, their appetite comes back (sometimes with a vengeance!) by evening.
Increased Heart Rate and Blood Pressure
It is typical for heart rate and blood pressure to increase mildly while taking these medicines. These changes are minor, and are similar to walking up a half flight of stairs. They do not place most people with ADHD at any risk.
Insomnia
From one-third to nearly one-half of patients placed on stimulant medication may notice that it is harder to fall asleep at bedtime (insomnia) after taking these medicines during the day. Adults find this less of a problem than do parents of children with ADHD. Some research has found that 20%–35% of people taking stimulants during the daytime actually fall asleep better than they did prior to taking medication.
Clinical Tips:
- If insomnia keeps a client up longer than an hour past the typical bedtime, you (or the prescriber) can consider reducing the dose or having the client take the medicine earlier in the morning.
- Another option is to try a medication that does not cause this side effect, such as the nonstimulants.
Nervous Tics and Mannerisms
One side effect that you should be somewhat concerned about is the possibility of nervous tics – abrupt twitches of small muscle groups around the face or, less likely, in other parts of the body. Nervous blinking, squinting, or making faces are just some of the tics that can be seen. Other tics are vocal – abrupt noises such as repeated sniffing, throat clearing, or sharp, loud utterances. In its extreme form, the combination of multiple body tics with these vocal noises is called Tourette syndrome. You should know that 10%–15% of typical children and fewer adults will show some sort of tic or nervous mannerism during childhood, so simple or occasional tics are nothing to worry about if they develop and may have nothing to do with the stimulant medication. Some research has shown that such tics in people with ADHD may be made worse by the medicine in a minority of cases (about 35% or fewer). If this happens, in my experience the tics return to their normal level within a week or so after the medicine is stoppedIn about half of the cases, the pre-existing tics remain unchanged from their premedication level. Evidence suggests that the amphetamine preparations, such as Dexedrine, are more likely to result in a worsening of tics than are those containing methylphenidate.
A few adults have developed the full Tourette syndrome, though it is not clear in research studies that the medicine caused the disorder. It may have worsened it or hastened its appearance in someone who was prone to get the disorder in the first place. But this is quite rare. In most cases, as I discussed above, clients with a history of tics or Tourette syndrome can take the stimulants safely with no worsening of their tics.
We have noticed that up to 15% of clients placed on stimulants may develop other simple nervous mannerisms, such as nail biting, skin picking, lip biting, or hair twirling, even if they did not have them previously.
Clinical Tips:
- A prescribing physician should ask whether the adult with ADHD has a personal or family history of tics or Tourette syndrome before trying a stimulant drug. If so, start the client on a lower-than-usual dose of medicine to see how they may react to these drugs.
- When these medications are used and tics (or other nervous mannerisms) develop, the treatment should be stopped immediately. The tics or other behavior will usually subside within 7-10 days. Treatment can then be resumed at a lower dose if the client’s behavioral adjustment has deteriorated dramatically.
- If the tics return even at the lower dose, trying an alternative medication (such as the nonstimulants discussed below) may be successful.
- Failing this, clients should be warned not to be treated with stimulants in the future without alerting the treating physician to this history of tic reactions to the stimulant medicines.
- Should tics worsen for a client who had them before taking stimulant medication, you can stop the medication, whereupon the tics often return to their previous levels, and consider a nonstimulant medication for ADHD management instead.
Temporary Psychosis
This is a very rare side effect at the typical doses used for managing ADHD. All of the stimulant medications have the potential to produce temporary symptoms of psychosis (thought disorganization, rapid speech, skin hallucinations, extreme anxiety, super-sensitivity to noises, etc.) at very high doses. In very rare cases, this can happen at low doses. Such reactions occur in fewer than 1% of treated cases, being slightly more common in very young children and less so in older ones. If this occurs, the problem often lasts only until the dose wears off.
Long-Term Effects
Critics of stimulant use for treating ADHD have contended that the stimulants pose a high risk because we have no long-term rigorously controlled studies on the potential long-term negative effects that might be caused by persistent use of the medications. Parents and colleagues likewise often ask about the status of evidence for long-term safety and effectiveness. The critics are right, up to a point, that we have no such studies, with the longest controlled randomized trials lasting up to three years. But here is why: the studies needed to address this issue are unethical and would be exorbitantly expensive and take a long time to complete, ensuring that no medications would be approved for use until at least one generation of children or adults had been followed for life after receiving these medications.
So, to evaluate the stimulants’ long-term safety, we must turn to other, somewhat less direct sources of information. Here are highlights of what we know:
- The stimulants have been on the market for 70–90 years, and in none of the millions of patients treated with these medications, many for at least several years, have any reports of significant long-term side effects been noted.
- The results of more than 700 short-term scientific studies do not imply that significant long-term side effects would be likely.
- Finally, so far, findings from studies of the neurochemical actions of these medications in the brains of humans have not shown any clear indications that long-term or enduring side effects would be expected from extended oral medication use.
What is important is that our understanding of the risks associated with the use of medications be well informed. As of this writing, the stimulant medications are safer and more effective than for nearly every other class of medication used in psychiatry, and that is all that can be said presently.
Atomoxetine (Strattera) and Viloxazine (Qelbree)
Strattera (atomoxetine) and viloxazine (Qelbree) are nonstimulant medications developed for the treatment of ADHD; the former having been FDA approved since 2003 for children and adults with ADHD and the latter just receiving FDA approval for use with children in April of 2021. Both are specific norepinephrine reuptake inhibitors. They slow down the reuptake or reabsorption of the neurotransmitter norepinephrine back into nerve cells in the brain once that chemical has been released during activation of that nerve cell. Whereas atomoxetine and viloxazine primarily affect norepinephrine reuptake, they may also have some effects on the chemical dopamine (somewhat like the stimulants discussed above). However, viloxazine may also have effects on the neurochemical serotonin. Numerous studies have now been published that demonstrate the effectiveness of atomoxetine in the treatment of ADHD. Markedly less so has been published to date on viloxazine. There is also extensive research available on the safety of these medications when used with children, teens, and, in the case of atomoxetine, with adults who have ADHD.
Since first being approved by the FDA in 2003, more than five million patients have taken atomoxetine, providing ample evidence for its effectiveness and safety. Given its strong similarity to atomoxetine, viloxazine will likely show a very similar profile of benefits and side effects. However, just a few studies currently exist on its benefits and side effects. Thus, atomoxetine is to be preferred for the moment given its larger evidence base.
Nonstimulant Side Effects
Unlike the stimulants, these nonstimulants do not result in insomnia or difficulties falling asleep in the evening. Atomoxetine also results in mild increases in diastolic blood pressure and heart rate but with no significant changes on electrocardiogram patterns (ECG intervals). Fewer than 10% of patients treated with this medication required stopping the medicine because of significant side effects. Research has now followed treated cases for more than three years and supports the long-term efficacy, safety, and tolerability of atomoxetine for the treatment of childhood and adult ADHD. Again, such results are very likely to be found eventually for viloxazine as well but they simply have not yet been thoroughly studied.
From 2003 to 2010, just two cases of severe liver injury were reported to the manufacturer of atomoxetine and the FDA out of more than five million patients who have taken it since its FDA approval. These patients recovered with normal liver function after discontinuing the medication. It is not clear in one of these cases that the liver problem was related to the medication, while in the second case it may have been.
Clinical Tips:
- For now, atomoxetine is the preferred drug compared to other nonstimulants given the greater length of time it has been approved and used for ADHD, the far greater number of controlled studies investigating it, and the vastly greater number of patients treated with it to date.
- Early evidence suggests that while both medicines may take several weeks to titrate the medicine to a therapeutic dose, the titration time for viloxazine may be somewhat less.
- These medications should be discontinued in any patients with jaundice (yellowing of the skin or whites of the eyes) or laboratory evidence of liver injury.
- Experts and the manufacturer recommend that patients on atomoxetine be cautioned to contact their doctor immediately if they develop pruritus, jaundice, dark urine, upper-right-sided abdominal tenderness, or unexplained “flu-like” symptoms. However, any risk of liver problems appears to be exceptionally rare.
Anti-Hypertensive
Drugs
Two other medicines are sometimes used to treat adult ADHD, but they should be
considered “last choice” medicines to be used only if the other ADHD medicines
are not proving satisfactory. Both originated as drugs used to treat high blood
pressure, called anti-hypertensive drugs. One is clonidine, and works as an
alpha-adrenergic enhancer. Some nerve cells in the brain have little portholes
on them called alpha-2 receptors. These drugs seem to act to reduce or close
off these portholes, which results in stronger or more effective nerve signals
in those cells. At low doses, this drug appears to stimulate inhibitory systems
in the brain. The FDA approved an extended-release version of clonidine,
clonidine ER (Kapvay®), in 2010 as a treatment for ADHD in children
ages 6-17. But as noted above, physicians can use it “off-label” outside of
this age range, such as for adults with ADHD. It can be used alone or combined
with stimulants. The drug is not as effective, in my opinion, as the other ADHD
medicines discussed above. So it is sometimes used to treat ADHD when it
co-exists with another disorder such as conduct or antisocial problems, or
irritability and anger. It can also treat tic disorders and sleep disturbances,
and may reduce anxiety. Regular clonidine is fast-acting, but the extended-release
version approved for ADHD can last much longer.
Another
anti-hypertensive drug used for ADHD management is guanfacine. In 2009, the FDA
approved an extended-release version, guanfacine ER (Intuniv®) for
the treatment of ADHD in people who are 6-17 years old. Again, physicians can
use it with adults off-label if they think it essential to do so. The drug can
be given alone or in combination with either of the stimulant medicines
discussed above. There may be some advantages of guanfacine over clonidine.
These include less sedation, a longer duration of action, and less risk of
cardiovascular problems. Its benefit may be in helping to treat coexisting
disorders with ADHD, such as anger and aggression, and in reducing highly
impulsive or hyperactive behavior.
Clinicians
and adults with ADHD should be aware that there is very little research on
using these two anti-hypertensive drugs to treat ADHD in adults. That is why
they were FDA-approved mainly for children, on which more research was
available. Because of the lack of research, these drugs are considered
last-choice options for managing adult ADHD. The other ADHD medicines above
should be tried first.
Off-Label Medications
Another
non-stimulant, bupropion, is sometimes used for treating adults with ADHD but
it is not FDA-approved for doing so. The drug is sold under the brand
name Wellbutrin® here in the U.S. While it also increases
norepinephrine in the brain by a mechanism similar to that of ATX, it also
affects other brain chemicals. That can be an advantage if a physician is
trying to treat ADHD and another disorder that responds to bupropion at the
same time, such as anxiety or mild depression. But it can also produce unwanted
side effects as well. It also may not work as well as the stimulants if all one
is trying to change are ADHD symptoms. It has not been studied as extensively
as ATX and so its value in managing ADHD is less well established. Even so,
some physicians can still use this drug for treating ADHD if they choose to do
so, known as “off-label” use. More often, the drug is used to manage a
co-existing anxiety disorder or mild depression in patients who also have ADHD.
Other
non-stimulants have also been used off-label to treat adult ADHD, such as
anti-depressants, anti-anxiety drugs, and even some mood stabilizers or anti-psychotic
drugs. None of these are especially effective for managing ADHD or have as
extensive a research background as the FDA-approved medicines discussed here.
Often they are being used to manage another co-existing disorder and may even
be combined with the ADHD drugs discussed here. The anti-narcoleptic drug,
modafinil (Provigil®), has shown some promising results as a
treatment for ADHD symptoms in children. Yet even then, the results have not
always been replicated in other studies. There is also no research as of this
writing on using this drug with adults with ADHD. The drug increases
wakefulness and arousal and sometimes has been used to treat sleep apnea
(disrupted breathing while asleep). But the drug has not received FDA approval
for ADHD as of this writing.
What
to Expect from Medication Treatment
Most
adults with ADHD experience a significant improvement in their symptoms from
these medications once a therapeutic dosage has been found for them. A minority
of patients reported such remarkable improvements that they had become functionally
normal. If so, patients may be joyful or near tears over just how well they are
able to function now that they have been treated. For some people, the
medication is the only treatment they may require to address their ADHD-related
concerns.
Most
people report that their symptoms are improved substantially due to medication.
They are: (1) more productive at work, (2) more attentive while engaged in
various tasks, (3) less impulsive and more thoughtful about what they are
doing, (4) less scattered or distractible in their ability to focus on tasks
and complete them, (5) less forgetful, (6) better able to organize their
thoughts, (7) better able to carry on conversations with others, (8) able to compose
written projects such as business letters or reports faster and more
coherently, (9) more persistent in following through on promises to others or
on activities, and (10) better emotionally controlled or stable.
Not
infrequently, adults with ADHD often say that they finally know what it is like
to feel or behave like a “normal” person or at least nearly so. Just don’t
expect that all of the client’s symptoms or concerns will be miraculously
solved. Troubles at work, in relationships, in school, or elsewhere can arise
from other sources besides ADHD. Consequently, treating the ADHD does not
always eliminate these other problems or unresolved issues. As noted earlier,
most people with ADHD have at least one other disorder and many have two other
disorders. Those other disorders are not likely to be spontaneously cured by
effectively treating their ADHD. Other treatments will be needed to address
those disorders.
The dosages needed to treat ADHD vary substantially across people, with some requiring very small doses, equal to those used with children. Others need substantially higher doses well above the average. Expect the client’s physician to try a range of dosages. The doctor will start with a low dose and then increase it every week until a good response is obtained or the adult with ADHD reports such annoying side effects that going to an even higher dosage is no longer an option. The adult with ADHD has a 75% chance of responding to whatever ADHD drug is tried first. But they need to be patient (not a strong suit of most adults with ADHD), as it can sometimes take two to three weeks or even one to two months to find the best dosage for their needs. The adult with ADHD has a 10%-25% chance of not responding to the first drug tried, and a 3%-10% chance of not being able to tolerate the drug at all. Be sure that the physician is getting information from others who know the adult with ADHD well, such as yourself or anyone they may be living with at the time. Sometimes these drugs can be improving their ADHD symptoms but they seem less aware of that change than do those around them.
If the first drug tried does not work or does not work as well as the adult with ADHD and the doctor would like, don’t worry. There are several other options that may well be the right ones for her. Adults with ADHD should keep trying other ADHD medicines and delivery systems if they didn’t respond to the first one tried. These drugs are among the safest and best-tested in all of psychiatry. Therefore, it pays for the adult with ADHD and their prescribing doctor to experiment with different drugs, dosages, and delivery systems so as to find what is right for them. A physician should only go off-label and use a non-FDA-approved drug for the client’s ADHD if they have not shown a positive response to any of the ADHD medications or if there is a very good reason not to start them on an ADHD drug first.
Other Issues in Using Medications for Adult ADHD
Taking ADHD Medications during Pregnancy
The fact that ADHD brings with it an increased risk of early pregnancy means that clinicians need to prepare for pregnancy in adolescents. There is little evidence concerning the effects of any ADHD medications on pregnant mothers or their babies. One large study reported in 2013 found that women with ADHD who took their stimulant medications while pregnant did not have a higher risk of having babies born with any obvious malformations. But a subsequent large study did report a possible risk for cardiac malformations in the baby. That finding has yet to be replicated. And a recent meta-analysis on the issue found no evidence of teratogenic effects but also warned that the literature was too limited to offer any definitive conclusions (see Li, et al., 2020). That said, the drugs may need to be taken during pregnancy because the risks to the mother of being off medication while having ADHD may be greater than the risks identified to date for her or the fetus from taking the medication. For instance, unmedicated women with ADHD are more at risk for traffic violations and car crashes, risky sexual behavior and concomitant sexually transmitted disease, suicide, disrupted parenting, marital or cohabiting stress, sexual victimization or intimate partner violence, and accidental injuries, among other health risks discussed above. Of course, at this time all companies recommend that women discontinue their ADHD medications should they become pregnant, but that has as much to do with protecting the company from liability as it does with the risk-benefit calculus that must be made by a clinician. So, the woman and her doctor must weigh the disadvantages of stopping medication because it will result in an increase in their ADHD symptoms and all the attendant risks that go with that unmanaged ADHD.
Tolerance to Medication
Actual physical tolerance seems unlikely with the current ADHD medications. But some individuals report that their medication seems less effective about three to six months after starting their treatment. This usually requires adjusting the dose or, sometimes, changing to a different delivery system or even a different medication. Clinically, we sometimes see people complaining that their medicine isn’t working as well. However further information shows them going through an unusually stressful or demanding period in their life that may exacerbate their ADHD symptoms and make it more difficult for their usual dose to provide adequate treatment. Temporary dose changes or addressing the source of the stress may be needed at these times.
Generic vs. Brand-Name Medicines
The generic medications appear not to be manufactured with the same degree of rigor as the brand-name medications. The generics have been associated with numerous clinician and patient reports of greater variability in controlling the ADHD symptoms on a day-to-day basis or have been reported to produce less success in managing those symptoms overall. Should that occur, and a patient be on an insurance plan that required the use of the generic version first, physicians can request a transfer to the brand-name medicine.
Addressing Medication Noncompliance
One of the greatest difficulties with ADHD medications is not that they do not work – clearly, they do. It is that people with ADHD are less and less likely to stay on them over the first six months or the next few years of being treated. This can be hard for some clinicians to understand. After all, if medications are effective, then why wouldn’t someone want to remain on them to get the most benefit from the treatment plan? That’s because there are other issues that cause noncompliance with medication even if it is effective at managing a disorder. Also, this nonadherence to medical advice is not just a problem in the field of ADHD. It can be seen across most of medicine when dealing with chronic conditions, including high blood pressure, high cholesterol, diabetes, epilepsy, and other chronic conditions. People simply don’t always do what is best for them for various reasons, especially when taking medications for chronic conditions.
The first thing you can do to facilitate compliance is to tell the client often how much improvement you have noticed in the client's symptoms and functioning since they started taking the medication. Sometimes, adults with ADHD are less aware of how well the medication is working than are those around them who see them frequently. So be sure to let them know of any positive signs you see that the medication may be helping them to deal with ADHD and the impairments in life activities it may be causing. If an adult still seems uncertain about using the medication, then consider some of the following reasons that those with ADHD may cease their medication even if it is effective. Along with these issues, I suggest some things you can do to hopefully address them.
Noncompliance Can Be Due to ADHD
Having ADHD can further contribute to the more typical problems with adhering to medical advice. That is because ADHD creates problems with self-regulation, which are the very mental abilities (the executive functions) we use to do what is best for us over the long term. It makes perfect sense that people who have a disorder of self-control have difficulty properly controlling the management of their medicine. That is because ADHD involves:
(1) Poor time management. Someone with ADHD may not take medications in a timely and consistent manner, may miss appointments with physicians to get refills, might fail to get to the pharmacy on time to get the refill (it’s closed), may miss the deadline to file for a renewal if it is via a mail-order prescription service, etc.
(2) Poor working memory, self-organization, and problem-solving. This can lead an adult with ADHD to not always remember to take the medications or parents with ADHD to not remember to have their child with ADHD take them as prescribed; to refill them when needed; to deal with the problems that can be posed by insurance companies or others that are covering part or all of the medication costs; much less even make and get to the doctor’s appointment to get a refill on their prescription, or to the pharmacy to fill it.
(3) Deficient self-restraint. This deficit often leads adults with ADHD (or parents with ADHD) to impulsively quit using the medication (or stop their child's medication) if there are annoying or unpleasant side effects; if the cost doesn’t seem worth the benefits to them; if they fear they or their child may be stigmatized if it is revealed to others that they take such medication; or if someone told them that the medications are dangerous and they can get by with natural remedies or healthier food.
(4) Low self-motivation. If this occurs, it can lead the adult with ADHD, or a parent of a child with ADHD, to do all the above, as well as to not even bother trying to make regular doctor’s appointments, take medication regularly, refill prescriptions, etc., all of which take not only time but extra effort.
(5) Poor emotion regulation. Many adults with ADHD have this problem. If so, it can lead them to become angry and quit the medical system, or get into arguments with family members if you bug them too much about taking the medicine, getting appropriate dosage adjustments, having patience while the medications first begin to be taken, etc.
(6) Diminished self-awareness. Many adults with ADHD are not as aware of the positive reductions in their symptoms and better functioning as those around them are.
(7) Positive illusory bias (viewing problems and deficits as not as bad as others see them or evidence proves them to be or not existing at all). This can lead an adult with ADHD to simply not see the problem area in the first place or to underappreciate its seriousness.
Another problem is that many of these medications, especially the stimulants, last only three to 12 hours in their effectiveness, depending on the type of medication and which delivery system is used (pills, pellets, pump, etc.). This means that there will be times, especially in the early mornings before the medication is taken or at night when it has worn off, that the medicine is not working at all because it is largely out of the bloodstream. Here again, the problems with ADHD symptoms and executive deficits can now interfere with complying with medical advice by the adult with ADHD.
Clinical Tips for Helping an Adult Become More Compliant
- Go back and review some of those treatment recommendations made earlier concerning the EF deficits and how to manage them. You can use these ideas to help your client cope with some of the executive deficits related to working memory, time management, organization, etc. When applied to helping the adult remember to take medications, keep doctor’s appointments, deal with pharmacies, etc., those suggestions might just help.
- Putting the pills in a pill organizer showing days of the week, available at any pharmacy, can help. Then try suggesting that the adult place this container right beside the bathroom sink where the person with ADHD always goes every morning. Putting it right in front of the adult while at the sink might help them with remembering to take their pills. But they still may need reminding each week to refill the organizer.
- To aid with self-awareness and that positive illusory bias, talk with your clients periodically about the benefits of medication you may be seeing both in their behavior and in the results (better school performance, better work participation, more responsibility at home, better management of money, etc.). Encourage others who care about them to do the same. This is so the client gets someone else’s perspective and does not base their decision to stay on or go off medication on their own subjective view. Just as with losing weight on a diet, there is nothing like hearing from others how much you have improved to keep someone motivated to stay in treatment. What else you do here to help really depends on just which of the ADHD/executive symptoms are contributing most to the problem of medication adherence.
There can be several other reasons an adult may not comply with taking recommended medications besides ADHD. Those reasons can tell you about how you may be able to help your client stick with a medication treatment plan.
“I really don’t have ADHD, so why am I taking these medications?”
This problem goes back to the one of not accepting the diagnosis, which was discussed earlier and which often comes up with young adults. So, you may need to go back and reread the suggestions about how to help deal with denial.
“I don’t like the idea of taking ‘drugs.’”
Unfortunately, the popular media has contributed to a perception that ADHD medications are the same as taking abusable “drugs” like an addict. Consequently, there is an unnecessary stigma and misperception attached to these medications that may not be the case with medications used for other medical conditions, such as high cholesterol. Yes, as was mentioned above, the stimulant medications do have some small abuse potential, but they are not being prescribed to make someone a drug addict, and they are not addictive when taken as prescribed. They are also not increasing any future risk of being dependent on or abusing these or any other drugs.
Let’s also realize that a large segment of our society wishes to be on presumably healthier and more natural or “organic” diets or to adopt vegetarian or vegan approaches to nutrition. Taking medications is often seen as contradictory to these and other “healthy” approaches to nutrition specifically and to lifestyle more generally. To counteract such views in your client, you can talk about the fact that all food involves chemistry that affects the body. Some natural chemicals are deadly, especially if taken in large quantities. Thus, the distinction between natural chemicals as being healthier for you than artificial chemicals doesn’t really hold up on close examination. If your client drinks coffee or uses alcohol, these are all chemicals that are natural but can be harmful when used to excess. They are often used for the changes they create in our mental functioning and not just our physical functioning. You can also discuss the fact that if your client had diabetes or epilepsy, they would not likely be against using medications to treat those life-debilitating or even life-threatening conditions. ADHD is no different. It is both debilitating and potentially life threatening (possibly causing accidents, injuries, poor health, cardiovascular disease, etc.) if not treated consistently and persistently.
Also, try to show a little understanding and empathy toward your clients around taking medicine. Tell them that you realize that no one really likes to take medications for a chronic problem, especially for managing behavior rather than physical functioning. Just as we don’t like taking medication routinely to reduce high cholesterol or for high blood pressure, your client may not like the idea of using medicines chronically. Moreover, this example can be used to educate your client that many, many people are taking various medications over the long term for chronic medical as well as psychiatric problems (think of arthritis, pain, headache, etc., not to mention vitamins and nutritional supplements such as fish oils, ginkgo biloba, garlic, etc.). Therefore, your client is not alone in needing to do so.
“I am doing well now, so I don’t need the medicine any longer.”
This is a rather paradoxical problem that occurs with psychiatric medications, including those used for other disorders such as bipolar disorder. When the drugs are effective, they can so reduce the patient’s symptoms and so improve daily functioning that the person comes to see themself as relatively normal. When this effect goes on for a while, the person may even come to see that much of the improvement is a result of other efforts to manage the condition or just to trying harder, rather than to the benefits of the medication. Or teens comes to think that since they are better, they never had a serious case of ADHD. Because the medication has reduced the very need to take it (serious symptoms), those symptoms no longer exist to give the client the motivation to have them treated. Such circular thinking can lead the person to believe they don’t need the medication any longer to function well and so they stop. This is clearly a misunderstanding.
Fortunately for the ADHD medications, such as the stimulants in particular, the drugs do not need to be taken for long periods before an initial effect is evident (minutes), or before a downstream effect on daily functioning shows up (days), from using the medications. Most of the medicines for ADHD can also be stopped abruptly without causing harm, the exception being the antihypertensive agents. That is because most, like the stimulants, are washing out of the body within 24 hours anyway, so the adult is having a drug washout period almost daily.
All this means that if your client doubts the benefits of stimulant medication or their continuing need for it, then there is little harm in having them stop the medication for a day or a weekend so they, and you, can see what happens. That is not the case for some of the nonstimulants, however, which need to be gradually discontinued for safety reasons. Be sure that your client discusses this with the prescribing physician before doing so just to be sure it is safe.
Typically, within one to three days after quitting the stimulant medicine, a difference becomes evident and convinces the client to return to taking medication. If it does not do so, then have your client speak with the prescribing doctor about the results of this brief trial. A change in dose may be needed. Just be sure that stopping the medicine occurs at a time that won’t pose undue risk to the client. Remember that being off the
ADHD medicine results in a return of the risks ADHD can pose, including accidental injury, driving problems, diminished child-raising abilities, and poor work performance, among others.
“I don’t think the medicine is doing any good.”
This complaint can be a little different from that above because here the is continuing to have problematic ADHD symptoms, but either the client or the spouse or employer is not impressed that the drug is helping much if at all. That can certainly happen where the medicine is not improving symptoms or not doing so completely. If you agree that no improvements are evident, then the thing to do is to consider changing the dose or the type of medication or have your client talk with the prescribing physician if that is not you. Your client or the support person could be right – this dose isn’t working. But that doesn’t mean that no dose will work or that no ADHD medicine type will help. To decide that one must try the different medicines and try higher doses.
Sometimes the improvements your client is getting from the medicine are about as good as they are going to get on any type of medicine. If the client has tried the others and still finds this to be the case, then trying the psychosocial treatments discussed above may be helpful when added to the medicine. In a minority of cases, combining different medicines may be the solution. These medicines each work differently in the brain, so combining them might provide wider improvements in symptom control than just one.
As stated above, adults with ADHD often have less self-awareness. That means that you, family members, and others may perceive positive benefits from the medication that go unappreciated by your client. To address that, tell your client what you see improving and what others have seen as well. Sometimes the problems that are still evident to your client may be ones that ADHD medicines cannot treat. Symptoms of depression and anxiety or other mood disorders are typically not helped by ADHD medicines. These may require separate treatments to be discussed with the prescribing physician. The problems in functioning in some domains may also not have much to do with ADHD, such as difficulties at work or in relationships with others or in school. The fact that these have not improved from taking medication might suggest they come from some other source, such as a difficult supervisor at work, jealousy in an intimate relationship, or a learning disability or too difficult a subject affecting school performance. These and other problems in functioning can arise from many other sources besides ADHD. Discuss this possibility with your client.
“I am not as [creative, fun, spontaneous, vibrant, etc.] as I used to be off the medicine.”
This can certainly be true, particularly for some adults. Lower levels of inhibition are related to higher levels of creativity--being less inhibited contributes to thinking of more unusual ways to do things or making unusual connections among our ideas. Inhibition allows us to suppress thinking of these more unusual ideas, largely because they may be distracting to the work we may need to do and because they are not relevant. But sometimes, what can seem like an irrelevant idea can be a quite useful or brilliant way of seeing something. Because ADHD medicines increase inhibition, which is largely for the better, they might just be reducing this capacity to make creative linkages across seemingly irrelevant ideas. Theoretically, that might reduce someone’s creativity, although it has not yet been studied in research.
Where such reduced creativity is the case, can the adult not take the medication on those days or hours of the day when focusing on creative work? Fortunately, the stimulants dissipate from the body within 24 hours, so they can be stopped and started like this typically without any significant harm occurring to that person. The same is not true for the nonstimulants.
Promising but Under-Investigated Therapies
Routine Physical Exercise
While
routine physical exercise is recommended for all adults, increasing research
suggests that it may be especially beneficial for people with ADHD. It seems to temporarily reduce the symptoms and/or
help the adult to better cope with their symptoms. It can also help to address
their propensity toward obesity, noted earlier. Some studies with children with
ADHD even suggest that just allowing some movement or fidgeting while working
can help those with ADHD to concentrate better and improve their performance of
mental work. There is no reason to think this would not work as well for adults
with ADHD, but good quality research specifically with adults with ADHD is
lacking. So the adult with ADHD might wish to think about how to incorporate
some repetitive movement into the work they have to do and even develop a
routine aerobic exercise program. This small motor activity while working or
studying can be something as simple as keeping a rubber ball or tennis ball in
the non-dominant hand and squeezing it frequently.
Understand of course that large muscle and aerobic exercise comes with its own risks, particularly for injuries. But done properly, moderately, and carefully, routine physical exercise may well prove to reduce symptoms, improve self-regulation, and help with weight management for adults with ADHD given that it provides such benefits in studies of general-population adults. No one particular form of sport or exercise has shown itself to be superior to others. Therefore, the adult with ADHD should be encouraged to identify a method of exercise that interests them, for which they may have some aptitude, and which they are most likely to incorporate routinely and easily into their daily schedule. They can then consider incorporating small motor activity into work/study periods as needed to help address ADHD symptoms in those settings.
Marital/Couples Counseling
There
is no research yet on the effectiveness of couples counseling for those couples
in which one has ADHD. But it is often a necessary therapy for adults with ADHD
and their cohabiting partners given the findings discussed earlier about the
social impairments often seen with ADHD. Low marital satisfaction, impulsive
emotional reactions, difficulties managing home responsibilities and finances,
driving problems, excess tobacco, alcohol, and drug use, greater health
problems, risky sexual practices and a propensity for casual sex (one-night
stands), and even a propensity for reactive aggression in intimate
relationships are among the many problems couples may face when one member has
adult ADHD. Helping couples address these problems through marital/couples
counseling will be essential for a substantial number of adults with ADHD.
Fortunately,
a few trade books exist to provide some preliminary guidance to such couples
about these problems and possible ways to address them. One excellent book is
by Gina Pera, Is It You, Me, or Adult ADHD. Another is by Melissa Orlov, The couple’s guide to thriving with ADHD. And a newer textbook for
clinicians has been published recently on couples’ difficulties and possible
counseling methods for adults with ADHD (by Ms. Pera and Arthur Robin, Ph.D.;
see Resources). So this remains an area in serious need of greater
empirical research on treatment methods that may be most effective in dealing
with the markedly higher rates of marital dissatisfaction, conflict, and even
intimate partner aggression linked to adult ADHD.
Vocational Assessment and Counseling
When
young adults are first starting to think about a career, those with ADHD would
likely benefit from being advised to seek out a thorough vocational assessment
first. There is almost no research on the issue of optimal occupational specialties
for adults with ADHD. But given what little is known, identifying an area of
vocational specialization for which a young adult has an aptitude would seem to
help with identifying those that will be most intrinsically interesting to that
young adult. Ideally, this evaluation should be done by a professional who is
knowledgeable about adult ADHD, although that is quite uncommon. More likely,
clinicians specializing in adult ADHD will need to combine their expertise on
the disorder with that of a professional in vocational assessment and
counseling in order to incorporate the specific knowledge of the problems
inherent in ADHD with the results of the vocational assessment. From such an
evaluation, one can suggest appropriate ADHD-friendly educational options and
career paths.
Research
suggests that such occupations include frequent movement, changes in the nature
of the work (or novelty), assignments that require multi-tasking, busy and
fast-paced work, hands-on or physically demanding tasks, intrinsically
interesting projects, and more frequent feedback about performance than may
occur in other, more sedentary, repetitive, and isolated work. Even if such a
counselor is not well aware of ADHD in adults, they can collaborate with those
professionals more traditionally trained in the disorder. The latter include
such professionals as clinical psychologists, psychiatrists, and clinical
social workers who can help adapt the results of the vocational assessment to
the particular symptoms and characteristics of the adult with ADHD.
Technology
Although
numerous “apps” have been developed to assist teens and adults with ADHD in
addressing the various problems they have with Executive Functioning in daily
life (time management, self-organization, etc.), no research is currently
available on their effectiveness. Off-loading the cognitive demands of tasks in
which the adult with ADHD may have some deficiency (e.g., scheduling, working
memory) onto either low-tech means (calendars, day-planners, paper lists, etc.)
or high-tech devices (computers, tablets, smartphones) does make some sense as
a method of compensating for these EF deficits. Dr. Kevin Murphy recommends
that adults with ADHD be aware of the tools technology may offer to assist them
in coping with their executive deficits. As he notes:
“A variety of
tools and devices can help greatly in communication, writing, spelling, keeping
track of time, and the like. Word processors and programs with spell-check and
grammar-check options can aid in writing and spelling more quickly, legibly,
and effectively. Smartphones, tablets, and PDAs offer a wide range of
components including an electronic address book, a planner/calendar, “to do”
list, and notepad. Smartphones and text messaging make communication easier,
more spontaneous, and faster. Many software programs are available to
assist with personal finances and taxes. Websites devoted to
organizational skills, time management, and just about any other relevant topic
are immediately available on the Internet. Electronic banking offers online
bill paying, including setting up automatic payments at regular intervals to
protect against delinquent payments and late fees. Books on tape and
voice-activated word-processing programs can assist in learning and writing.
“Smart pens” can greatly assist students in note taking and recording classroom
lectures. These sorts of devices and interventions should be used whenever
appropriate, but will require time, practice, and persistence to master.”
Mindfulness Meditation
One
treatment approach for adult ADHD that is becoming more popular but which does
not yet have a sufficient evidence base in the scientific literature to
definitively determine its effectiveness is mindfulness meditation. It is often
recommended in the mainstream media as a self-help approach to coping with
stress, anxiety, depression, and other emotional difficulties. It has also been
recommended for coping with psychological problems that may be associated with
chronic health problems or even life-threatening disorders such as cancer.
The
next figure summarizes the mindfulness meditation approach developed by Susan
Smalley and colleagues at the UCLA Medical School. It is certainly
representative of similar approaches used by others.
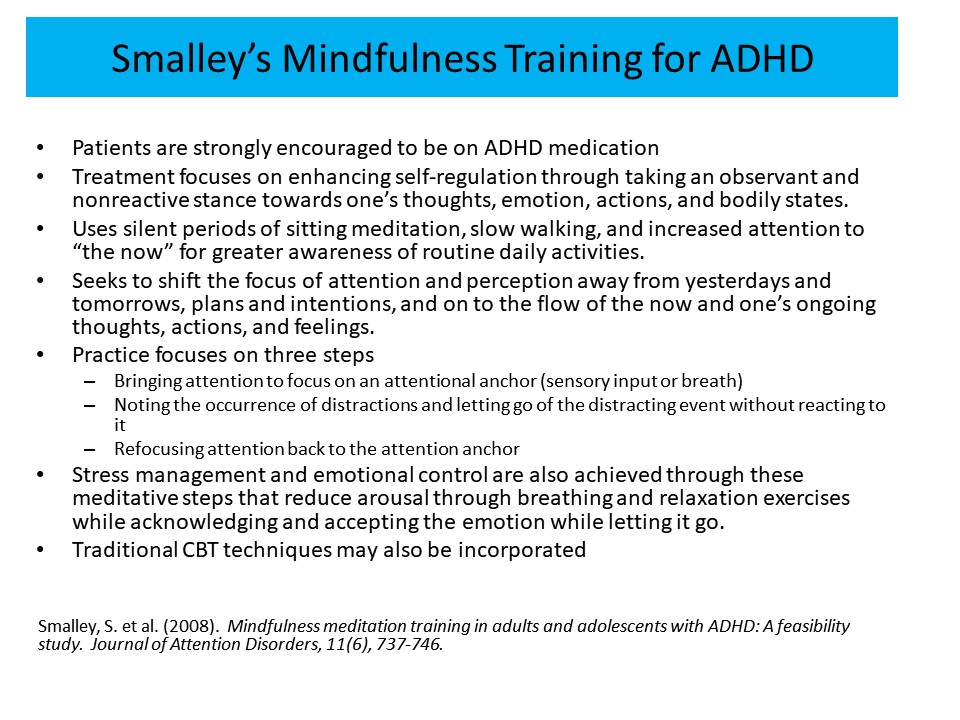
A
somewhat different approach that has received more attention recently is the
mindfulness meditation method developed by Lydia Zylowska and colleagues (see Resources).
In an initial feasibility study, Zylowski and colleagues enrolled 24 adults and
eight teens with ADHD in an eight-week mindfulness meditation program and found
significant pre- to post-treatment improvements in ADHD symptoms, anxiety, and
depression. Satisfaction with the program was good. Yet, this is merely a
quasi-experimental design lacking in the more rigorous methods (placebo or
alternative treatment comparison group, blinded assessments, appropriate same
size, etc.) needed to fully evaluate the effectiveness of this approach.
Another pilot study of this same approach likewise demonstrated effectiveness
for ADHD and related EF deficits, among other outcome measures, and had the
added advantage of at least a wait-list comparison group.
And
so while initial clinical reports suggest some promise for this approach to
treating adult ADHD, those reports and other studies were typically not
rigorously done sufficiently to definitively evaluate the effectiveness of this
therapy for ADHD. That leaves the results to date open to considerable debate
and even doubt. Until that type of research is done, mindfulness meditation is
not recommended as a first-line treatment for adult ADHD as would be ADHD
medications and Cognitive Behavioral Therapy (CBT). Dr. Mary Solanto and her
student Ayman Househam from NYU Medical School, recently reviewed the research
to date on this treatment, concluding that the evidence, while quite promising,
has not yet proven its effectiveness for adult ADHD. But they believe that
there is reason to pursue additional, more rigorous research. More information
on this treatment can be found on the Internet. Additional information on this
approach is contained in the book by Zylowska and Seifel, The Mindfulness
Prescription for Adult ADHD (see Resources).
Despite
the existence of much promise in the available, yet limited, evidence base for
the above non-medication treatments for adult ADHD, such interventions do not
have anywhere near the amount of evidence for their effectiveness as do ADHD
medications, suggesting that much more research is needed before these
treatments can be viewed with the same degree of confidence as can medications.
General Strategies for Managing Adult ADHD
Before
reviewing the specific strategies that can be used in particular domains of
major life activities for adult ADHD, here are some common-sense suggestions
that can help manage the symptoms and impairments from the disorder based on what
is known about it as a disorder of EF and self-regulation.
ADHD is a Disorder of Performance, Not of Knowledge
The
problems those with ADHD experience in major life activities have more to do
with not using what they know than with not knowing what to do. Adult ADHD
is therefore a disorder of performance – a problem of not doing what one knows
to do. Like patients with injuries to the frontal lobes, adults with ADHD
find that what they know does not guide what they do (performance). Thus, the
individual with ADHD may know how to act but may not act that way when placed
in social settings where such action would be beneficial for them in the long
term! The timing and timeliness of behavior is being disrupted in ADHD, not the
basic knowledge or skills.
From
this vantage point, treatments for ADHD will be most helpful when they assist
with helping the adult do what they know is best to do at the point of
performance, where it would be best to do it. That “point” is the place in
the natural environment where they are having problems. Addressing ADHD
requires helping that person to show what they know at those crucial places –
at those points of performance. A related idea to this is that the further away
in space and time a treatment is from this point, the less effective it is
likely to be in assisting with the management of ADHD at that point in the
natural environment. Not only is assistance at the “point of performance” going
to prove critical to treatment success, so is assistance with the time, timing,
and timeliness of behavior in those with ADHD.
This will not be achieved just by training a person with ADHD in what to do. It must come from arranging the particular problem setting in such a way as to assist them to actually do it. Nor will there necessarily be any lasting value or maintenance of treatment benefits from providing that kind of assistance if it is summarily removed within a short period of time. The value of such treatments at the point of performance lies not only in providing assistance by helping the adult with ADHD show what they know; it also rests in maintaining the scaffolding at that point of performance so that the improved behavior can be sustained over time in that natural setting. Yes, there is the possibility that with sufficient repetition and success the individual can even reduce or remove some or all of this “scaffolding” or accommodations due to habit formation. But that takes time and repeated practice within that setting so as to make an effortful behavior more automatic.
Reject Treatments that Don’t Address the “Point of Performance”
Given
the above considerations, adults with ADHD should likely reject most treatment
recommendations that do not involve helping them with these sorts of active
interventions at the points of performance in their daily life where they are
having major problems due to ADHD. These are treatments such as talk- or
insight-oriented therapy, psychoanalysis, weekly group therapy focusing on
complaining or general self-disclosure of feelings, etc. Those treatments are
just not going to do it for the executive deficits that ADHD has created.
Mental Information Does Not Guide Behavior Very Well
Adults
normally regulate much of their behavior by using mental information (held in
their working memory) that guides what they are doing. This working memory
capacity is less effective in those with ADHD.
The
accommodation then is: Don’t rely so heavily on mental information. Instead,
make that information physical in some way in that situation – “externalize” it.
Clinicians and the adult with ADHD can do that by placing the information in
some physical form in front of them to remind them of what needs to be done.
For instance, if the client’s boss or someone else has given a set of
instructions to get something done over the next few days, have them stop trying
to carry this around in their head so they can remember it over that period of
time. That can’t work if they have ADHD. Instead, have them always carry a small
journal and pen and instantly write down the task, any steps given to them to
get it done, and the deadline for when it’s due. Then make sure they keep this
journal in front of them where the work is to be done over the next few days to
help remind them of the project to be done. The journal can serve as an external
type of working memory.
Clinicians
can even help the adult with ADHD translate this written plan into smaller
steps and insert them into a day planner as goals for each hour of that day
and even over the next few days before the work is due. The technique here is
not what is important – the principle behind it is! Make important information,
plans, goals, and deadlines external (in a physical form) around the adult with
ADHD (within their sensory fields) in problem situations if clinicians hope to
improve their chances of getting things done. In tech-speak, off-load the
information that must be held in mind to some other, more physical medium that
exists in that situation or workspace.
ADHD Means Being Blind to Time
This
is one of the most important ideas clinicians and the adult with ADHD can learn
about adult ADHD from viewing it as a disorder of EF. It not only gives
clinicians both a deeper understanding of its nature but a richer understanding
of how to help. Difficulty with organizing behavior across time, known as time
management, is one of the ultimate mental deficiencies created by ADHD. ADHD is
to time what nearsightedness is to vision. The disorder creates nearsightedness
toward the future. The individual’s behavior is being governed by events close
at hand and not by events in the more distant future. Things that are within
“the now” and the immediate situation control them far more than thoughts about
“the later.” The adult with ADHD is not able to think as well about long-term
future events related to that situation. They simply don’t stop to think before
they act. Instead they act on impulse and pay a heavy price for doing so. This
helps us to understand why adults with ADHD make the decisions they do,
shortsighted as those decisions often seem to be. If one is not able to
consider future consequences, then much of that person’s behavior will be aimed
at maximizing the immediate rewards. It will also be aimed at escaping from
immediate hardships without concern for the later negative consequences of
those actions.
How
can clinicians help?
Make
time physical. That is, make time more visible in situations where time matters. The adult
with ADHD can do this with kitchen timers, clocks, computers that give periodic
reminders about deadlines, day-planners or week-at-a-glance desk calendars that
show the days broken down into hourly units, cell-phone timing devices,
smartphones with deadline reminders, etc. The ways to do this are countless,
but it’s the principle that is important here. The more external or physical
one can make the passage of time in front of them and structure that time with
periodic physical reminders, the more likely they are to better manage their time.
Reduce
or eliminate the problematic timing elements of a task when
feasible. For instance, rather than have the adult with ADHD take on a task
that has large time gaps in it such as one that can be done over days or weeks
of time, reduce or eliminate those gaps whenever possible. Instead of them
accepting a project that must be done over the next month as is, encourage them
to break it down into much smaller steps and try to do a step a day toward that
eventual goal. That way, each step does not seem so overwhelming as does the
entire project. Breaking big projects into small steps makes it much easier to
get motivated to do a smaller chunk of work. When those small tasks are done
every day, then when the deadline arrives the work will have been done.
ADHD Reduces Internal or Self-Motivation
Viewing adult ADHD as an EF disorder also implies that it greatly reduces a person’s ability to create internal motivation; what we generally call self-motivation, drive, persistence, or stick-to-it-iveness. The adults with ADHD can’t self-motivate like other adults are able to. They cannot do as well at getting themselves “pumped up” or activated to start projects or to sustain motivation for the activities that need to be done over time toward deadlines and goals as well as others.
How
to help:
- Encourage adults with ADHD to arrange for frequent external types of motivation to help them get through the job. For instance, break a project into smaller pieces so that each piece takes just a short time to do. Then have them allow themselves a small respite from work at the end of completing each piece, such as at the end of each hour or even half-hour of sustained work they can stretch, get a soda or coffee, check their smartphone for new email, text messages, or Facebook posts, etc., but only briefly!
- Have the adult with ADHD arrange small rewards for completing smaller work quotas instead of waiting until the work is all done. Such artificial reward programs function for the adult with ADHD like a prosthesis does for the physically disabled. The rewards are like the wheelchairs, mechanical limbs, or crutches that someone with a physical disability needs to function more normally in a situation. The motivational disability created by ADHD makes using such motivational devices or “prostheses” nearly essential if longer-term projects, assignments, personal plans, or social promises are to be successfully fulfilled.
- Encourage the adult with ADHD to make arrangements to be more accountable to others, such as finding a coworker or supportive supervisor for them to check in with frequently to review the progress they are making in getting an assigned project completed. Doing so can boost a person’s motivation to get work done, compared to situations in which they have no accountability to others and must work independently.
Manage the External Environment to Manage the Symptoms
As
noted earlier, ADHD prevents adults from thinking as well as others both
before and while they are behaving – they are less capable of using mental
information to contemplate what they need to be doing and to guide them along so
they do it. The solution to this problem is not to nag those with ADHD to
simply try harder or to remember what they are supposed to be working on. It is
instead to take charge of that immediate context and fill it with physical cues
to help them remember what to do and to stay on task. The external environment
has a stronger pull or influence over the behavior of someone with adult ADHD,
and that environment is often filled with irrelevant and distracting events.
Encourage
the adult with ADHD to get rid of those distractions in the places where
they typically work. Replace them with cues, reminders, cards, lists,
signs, sticky notes, day planners, or whatever devices will keep their mind
focused on the task and goals at hand.
Rules Alone Don’t Guide Behavior Very Well
Adults
normally possess sets of internal rules for what to do or how to act in
particular situations, such as at work, in school, while driving, or even when
in social gatherings. Adults activate these mental rules at those crucial times
to guide them more effectively through that situation. Adults with ADHD are far
less likely to activate these rules. Even if they do, the rules or instructions
they recall don’t control their behavior very well. Remember, ADHD makes mental
forms of information very weak as a means of controlling one’s own behavior.
What
can clinicians do to help?
- Encourage
or even help the adult with ADHD to make the rules into physical lists,
such as by using 3x5 file cards or “to do” lists. Externalize the important
rules! The rules or instructions for a particular task can be externalized by
posting them on things like small signs, lists, charts, sticky notes, etc. in
the appropriate place at school, at work, or in a social environment. Encourage
them to frequently refer to these lists or other cues while they are in
those situations.
- Recommend
that adults with ADHD talk out loud in a low voice or whisper to themselves
and state these rules aloud before and during these situations as another
way to stay on task. Talking to ourselves out loud is a great way to help keep
our mind and behavior focused on our work.
- Suggest
that they digitally record these reminders on a recorder and then play them
back again in that situation, even listening to them through an earphone so
as not to disturb others while they are working.
View ADHD as the Diabetes of Psychiatry – A Chronic Disorder that Can Be
Effectively Managed
As
noted earlier, the approach taken to the management of ADHD must be the same as
that taken in the management of other chronic medical disorders or for other
chronic developmental disabilities. Diabetes is a good example of just such a
medical disorder to help clinicians and the adult with ADHD grasp this point.
At the time of diagnosis, all involved realize that no cure exists for
diabetes. Still, multiple means of treatment do exist that can provide
symptomatic relief and thus reduce the deleterious effects of the condition.
Such steps may include taking daily doses of medication and changing settings,
tasks, and lifestyles. Immediately following diagnosis, the clinician educates
the patient and family on the nature of the chronic disorder, and then designs
and implements a daily treatment package for the condition. This package must
be maintained over long periods so as to sustain the symptomatic relief that
the treatments initially achieve. Ideally, the treatment package, so
maintained, will reduce or eliminate the secondary consequences of leaving the
condition unmanaged.
However,
each patient is different and so is each instance of the chronic condition
being treated. As a result, symptom breakthroughs and crises are likely to
occur periodically over the course of treatment that may demand re-intervention
or the implementation of modified or entirely new treatment packages. Changes
to the environment that may assist those with the disorder are not viewed as
somehow correcting earlier faulty learning or leading to permanent improvements
that can permit the treatments to be withdrawn. Instead, the more appropriate
view of psychological treatment is one of designing an artificial social
environment that serves to help the adult with ADHD better cope with and
compensate for their disorder.
Throughout
all this, the goal of the adult with ADHD, their family members, and their
treating professionals is to try to achieve an improvement in the quality of
life and success for the individual, though life with ADHD may never be totally
normal.
Specific Strategies for Assisting Adults with ADHD in Major Life Activities
The
following specific strategies are common-sense recommendations given the risks
for adverse outcomes noted earlier in this course and the fact that they have
been found to be useful clinical recommendations in professional settings by
many specialists in adult ADHD. Granted, research on their effectiveness still
needs to be done, but in the meantime, the following strategies may serve to
benefit adults with ADHD in dealing with problems caused by their symptoms and
EF deficits in these specific domains of major life activities.
Work and School Settings
As
discussed in earlier sections above, the vast majority of adults with ADHD
experience problems in their educational history. They are likely to still do
so if they are pursuing adult education classes or workplace educational
programs. If the adult with ADHD is a young adult who is in college or
technical training, then they will likely require certain accommodations to help
them succeed. Adults with ADHD are entitled to reasonable adjustments or
accommodations in their educational activities as well as in the workplace, as
provided under the Americans with Disabilities Act (ADA), depending on the
severity of their disorder, extent of impairment (disability), and the
reasonableness of the requested accommodations. Clinicians may want to become
familiar with the requirements for documenting a diagnosis of ADHD under the
ADA, especially its most recent reauthorization, as this will have to be
provided to the college or employer if the adult with ADHD wishes to take
advantage of these reasonable accommodations. Several books that can explain
the protections afforded against discrimination under this act can be found below
in the Resources section. Those books also explain the documentation
needed to access such protections and accommodations, and the sorts of
reasonable adjustments to the school or workplace setting that may be required
to assist the adult with ADHD.
Besides
taking medication, a variety of strategies exist that may prove useful in the
school or workplace environment to help compensate for ADHD and associated EF
deficits. This assumes, of course, that these strategies are feasible to
implement in those settings.
Find
a “coach” or “mentor” to whom the adult with ADHD can ask to be held accountable several times each
day for the work that needs to get done that day. This can be a teacher,
professor, roommate, classmate, more senior student, or someone in the special
student services office. At work, it can be a co-worker, friend, or supportive
supervisor. The adult with ADHD can also hire a formal ADHD Coach, as discussed
above. If possible, the adult with ADHD should meet with this person for five
minutes two to three times each weekday. Use the first meeting, usually in the
morning, to review their “to do” list or goals for that day. Then they should meet
with that person again at mid-day (lunchtime, perhaps) and again late in the
day to show the mentor what items on that list have been accomplished. One
sure-fire way to help adults with ADHD stay focused and on-task in pursuing
goals and work is to have them be accountable to someone else they have agreed to
involve, and meet with that person frequently.
Identify
the ADHD specialist if the adult with ADHD is in a college setting (usually they are
in a student special or disability services office) or the disability
specialist in human resources in the workplace. This is usually the person to whom the adult with ADHD must declare that they have ADHD and to whom the documentation (prior evaluations) that proves it should be provided. That specialist will then explain the types of curriculum adjustments and other accommodations typically provided to students with ADHD in that college, or workplace adjustments, to see which ones they may need. They will also work with the teachers (or supervisors, if at work) to see that they get those accommodations. And they can often be linked up with psychologists, counselors, and physicians (usually psychiatrists) that work at the student counseling center or that have contracts with the employer for providing employee mental health services should they require therapy or medication.
Encourage
the adult with ADHD to use a daily assignment calendar and a journal. The calendar is for setting goals for that day and tracking appointments. Typically, it shows the entire week at a glance broken down into one-hour segments. This can be very useful not only for tracking appointments, but also for entering in the time one plans to use to handle a project or smaller steps of a more complex, longer-term project. The journal is simply a book with blank pages into which they can write any promises, deadlines, assignments from others, etc. Later, some of these can be transferred into the calendar. These two books are what they will review with the “coach” during the meetings discussed above. They should keep both in a visible spot in the workspace so they can see them often and be reminded to stay focused on goals and appointments for that day. Writing everything down can help compensate for a poor working memory. The adult with ADHD can use a journal for anything of the slightest importance that should be written there to make up for their working memory deficits. Yes, one can use computers, tablets, or smartphones to take such notes – and this may be preferable if they have trouble with handwriting (see the next strategy). But generally, low-tech paper journals and calendars are better, as they are always visible and available for writing. The relevant apps on smartphones or iPads disappear from view when the device is closed, and thus become out of sight, out of mind, and of little help. Clinicians should suggest that the adult with ADHD review this journal several times a day to make sure they are doing the things recorded there.
Use
word processing on a computer rather than handwriting lengthy assignments. People with ADHD often have motor coordination or other handwriting problems that make them slower to write and have less legible handwriting. Whenever possible, adults with ADHD should use a laptop computer or other means to type their work. In college, the adult with ADHD may also use the word processor for easier note-taking. They can also record some of the assignments this way. Computers with cameras can also be used to create an audio CD or media file as an alternative to a written report if they have a history of significant writing problems. The special student services counselor mentioned above may be able to get them this type of curriculum adjustment if they require it. Or, many recent-generation computers, smartphones, and tables have voice recognition software built into them that allows the adult with ADHD to dictate assignment answers or lengthier reports that are then automatically transcribed into print. Those passages can then be further edited before being printed out on paper as their report.
Digitally
record important lectures or meetings, or use a smart pen digital recorder (such as can be found at livescribe.com). Or, if handwriting is not a problem, use continuous note-taking to boost concentration in classes or meetings. As one way to stay awake, alert, and focused is to be doing something active, they should keep the hand moving continuously and take notes even if they don’t really need to write down the information.
Get
any extra-curriculum materials teachers may have available or that have been
reserved at the library especially for these classes. These may be videos that
supplement what is being taught in class, additional notes or articles that
further explain the topics that are being covered in class, etc. In the
workplace, the adult with ADHD should check to see if there is a library or
information center that contains resources for further learning on the job.
Get
the adult with ADHD a notebook organizing system at the local bookstore or office supply store to help them get and stay organized. Having separate colored folders for each school class or project at work can be very helpful. This is where they can keep completed assignments to ensure that assignments can be easily found and so turned in on time. It is not unusual for adults with ADHD in college settings or at work to do assignments and then misplace their work. Then they are not able to find the work on the date that it is due in their classes or to their supervisors. Since many people now store their work on computers in digital files, encourage the adult with ADHD (or assist them directly) to better organize these files for easier access, relocating them when needed, and backing them up to cloud storage facilities for safe keeping such as with DropBox, iCloud, etc.
Suggest
that adults with ADHD schedule harder classes/meetings/work during their “peak
performance” time slot each day. For most people, this may be the
mid-morning or early afternoon, but people vary in the time each day they are
most alert. From prior experience, the adult with ADHD should know when these
peak hours of alertness and concentration are likely to occur each day. Some
research shows that adults with ADHD have an altered circadian rhythm and
possibly an altered sleep cycle, and so find afternoons or even evening hours
to be their best time to focus and concentrate. This is a few hours later than
adults in the general population are likely to report as their peak performance
time. In any case, encourage the adult with ADHD to identify their daily cycle of
arousal and alertness and use that knowledge to better schedule those tasks
that require more concentration and effort into that time slot.
The
adult with ADHD should alternate required or harder courses with elective or
fun classes during the day or across the weekly schedule of classes. Don’t let them stack all the hard classes into a single day or during the first few days of the week, as this can over-tax them. It can also make them too tired to do well in these classes, lose interest or motivation part way through them, and ruin their attitude toward school in general. So suggest that they intermingle the hard stuff with classes or activities they find more interesting or entertaining. That way trhey are never faced with too many classes or projects that are boring or demand lots of effort being too close together. Clinicians can suggest that adults with ADHD do this at work as well by arranging the work each day so that they alternate difficult/demanding tasks with easy/interesting tasks.
Should
the adult with ADHD request extra time on timed tests in college or at work? Many young adults
with ADHD in college settings believe or have heard from others that this may
be a useful accommodation to request. But what little research there is on the
subject is not that clear cut. Everyone, disabled or not, seems to benefit from
some extra time to take timed tests. But that does not mean it will necessarily
help compensate for ADHD or solve other problems with taking these tests, such
as test anxiety.
More recent opinion suggests that the adult with ADHD might be better off using a method called “time off the clock.” This involves using a stopwatch to take these timed tests. The adult will not get any more “face time” with the test using the stopwatch than do other students. But what they will be allowed to do is to stop the watch anytime, as often as they like, to take a short break of a minute or two. Use this time to stand up, stretch, walk about the room or into the hallway, get a drink of water, use the bathroom, then return to the test and restart the stopwatch. When they have used up the test time on the stopwatch, then the test is done.
Yes, this will result in taking more time than others to complete the test, but that is not the point. The strategy that one is using here is the important thing. That strategy is breaking up the test into smaller work quotas and having frequent breaks to briefly refresh their mental focus and concentration. If they are required to periodically take timed examinations as part of their work, they should try to get this type of accommodation on the tests by using the human resources department that is responsible for implementing ADA accommodations in that work setting. Whether or not a “time off the clock” approach is allowed, encourage the adult with ADHD to request test settings that are free of distractions or offer greatly reduced chances of being distracted.
Encourage
the adult with ADHD to exercise before exams, boring classes, extended meetings
at work, or protracted work periods. As discussed above, routine aerobic exercise improves a person’s ability to concentrate for up to 45-60 minutes more than usual should they have ADHD. Adults with ADHD should learn to build in brief exercise breaks throughout the day but use them especially before they have to do something that is difficult to concentrate on or pay attention to during that day. Although adults with ADHD are also encouraged to routinely engage in more extensive workouts regularly throughout a typical week, that is not what is being suggested here. Here we are encouraging much briefer exercise periods – just two to five minutes of exercise may be enough to help the adult with ADHD concentrate better if it is done just before they enter a boring or demanding class or exam. If the class, meeting, or work project is long enough that they are being given beverage or restroom breaks, suggest that they use those breaks to do a quick aerobic exercise. This can be helpful even if it is just faster-than-normal walking outside the building, in the hallway adjacent to the work area, or walking up and down stairs in a nearby stairwell.
While
in settings where staying seated is required, suggest that the adult with ADHD
engage in small motor activities. This was discussed earlier.
Wear
a tactile cueing device to frequently prompt self-awareness and focus on goals
or the work at hand.
For a small amount, one can buy “The MotivAider” on the Internet (check the
website: addwarehouse.com). This is a small plastic box about the size of a
cell phone that contains a vibrator inside and a digital clock. The clock can
be set for any intervals one may wish, or one may choose the random setting.
When the interval expires, the device vibrates (or will do so at unpredictable
intervals if they chose the random option). This tactile cue can serve to
remind the adult with ADHD to stay alert and focused on what they are doing.
If adults with ADHD have lots of reading to do for school or work, encourage them to learn to use the SQ4R method for improving their reading comprehension, if that is a problem for them. The chart below shows how it works.
Improved Reading Comprehension - The SQ4R System |
Survey the material to
be read – just leaf through it quickly to get some idea of how much is to be
read, how it is broken up, etc.
Draft
some Questions that need to be answered from what is to
be read. Often these are at the end of the chapter to be read or have been
provided by the teacher or workplace supervisor.
Now
use the 4Rs: Read just one paragraph, Recite
out loud in a soft voice or whisper what was important in that material, wRite
that material down in your notebook, then Review it.
Do
this for each paragraph. This not only makes the ADHD adult review what was
read four times per paragraph (read, recite, write, review) but it gives
frequent mental breaks at the end of each paragraph. That can happen as she
or he shifts their concentration from reading, to reciting, to writing, to
reviewing across the assignment. As the adult with ADHD gets good at this,
they can read longer passages, such as two paragraphs at a time or even
an entire page before engaging in the recite, write, and review steps. This is
a great strategy for people with working memory problems. |
Try
some peer/co-worker tutoring.
This is where the adult with ADHD and a
fellow student agree to study together and alternate teaching each other the
material. One of them is the instructor, the other the student. Then they
reverse these roles with each tutoring session. Having to teach someone new
material is a sure-fire way to learn and retain such information compared to
just routine independent study. The same method can be applied at work with a
co-worker when new material needs to be absorbed.
Suggest
that the adult with ADHD work as a team with more organized people.
Working around or
with others who do not have ADHD can serve to keep them better focused on the
work that is to be done. It also makes them more publicly accountable for doing
that work than if they go solo and does the work in isolation.
Find
a “fall-back” college classmate or co-worker.
The adult with ADHD will use this
person in any instance where they are outside of school classes or away from work
and finds that they have forgotten an assignment or other important information.
Suggest that they swap contact information with this other person and do the same in return. That way both people can get the lost or missing assignments or
information quickly when either one finds they have this problem.
Attend
after-class (or after-work) help sessions whenever they are given.
Many teachers in
college or instructors in workplace educational settings are willing to set
aside extra time to help people who need more instructor assistance in learning
a topic. If that is available at the college or worksite of the adult with
ADHD, then recommend that they use it to the hilt. Even if they don’t really
need the assistance, the extra review will help with forgetfulness. It will
also show them to be a motivated student or employee and so make a better
impression with instructors.
The
adult with ADHD should schedule faculty or supervisor review meetings often –
every three to six weeks (not at the end of grading periods or only at workplace
performance review meetings).
Remember that the more often the adult with ADHD is held accountable for their work, the better they will do. So, in addition to using the “coaching” suggestion above each day, suggest that they schedule more frequent and informal reviews with the people actually responsible for grading or evaluating their work at school or on their job. This lets them get more frequent feedback more quickly on just how well they are doing.
Gently
prompt the adult with ADHD to watch, limit, or eliminate the caffeine,
nicotine, alcohol, or marijuana use.
Adults with ADHD are more prone than
others to use these substances and become dependent on them. And they sometimes
try to self-medicate their own disorder using readily available
caffeine-containing beverages or tobacco products. Yes, caffeine and nicotine
are stimulants and they can help people be more alert, though nowhere nearly as
well as the ADHD medications do. But caffeine especially works on the wrong
brain neurochemicals for people with ADHD and it can, in moderate or high
doses, be counterproductive. That is because it makes the adult with ADHD less
focused, more jumpy and jittery, more nervous, and more likely to frequently
need to urinate. They are better off using a prescription ADHD drug than trying
to use substances containing caffeine or over-the-counter pills that contain
caffeine. And, while nicotine may benefit ADHD symptoms to some degree, it is a
highly addictive drug with which to self-medicate. Doing so is only going to
increase the risk of addiction to this chemical, not to mention increase the risk
for pulmonary and heart disease and cancer. Again, using a prescription ADHD
drug instead does not carry such risks and is far more effective.
Help the adult with ADHD manage their
internet use.
The
Internet can become a big source of wasted time and an incredible distraction
from work or home tasks, even for typical people. But for adults with ADHD who
already have significant problems with self-control, having Internet access
readily available at home or work can pose far worse problems. Research shows
that teens and adults with ADHD spend far more time on the Internet, whether
surfing various websites or gaming, than do typical people of the same age.
They are also far more likely to have problems disengaging from the Internet or
gaming when the situation demands that they shift to other more important
things which need to get done. And 15%-20% of young adults with ADHD can be
said to be Internet-addicted, showing all the typical signs of dependence or
addiction often used to diagnose more common alcohol and drug addictions. There
are a few things that clinicians can advise the adult with ADHD to do at work
or at home if the Internet is proving to be a serious and prolonged source of
distraction for them and interfering with other more important demands. If the
adult with ADHD is not sure just how much time is being wasted on the Internet,
recommend a software program such as RescueTime be installed on that
computer. It will track each Internet page that was opened, how long was spent
on that website, and even send clinicians or the adult with ADHD a report
broken down by categories including the websites they are browsing the most. What
else can clinicians do to help alleviate this symptom?
At
home, place the computer and Internet access in a space set aside for working,
such as a home office.
Don’t just leave computers, iPads, and other
Internet-enabled devices in bedrooms, family rooms, and kitchens where they
will tend to easily capture the ADHD adult’s attention during times when they
should be busy doing more important tasks or projects. Advise the adult with
ADHD to have a room for computers and only use these rooms when computer work
is to be done, while otherwise keeping the computer out of sight (and so out of
mind) when tasks are being done that don’t require the use of computers or the
Internet. When in the workspace, have them keep the door closed and wear
headphones or use a “white noise” machine if necessary to cut down on
distractions that might divert them from their work.
Better
yet, set up two different computers – one for work only and the other for play.
The adult with ADHD can use a desktop or laptop computer for their work. This computer is only to have programs on it critical to the type of work that they need to do. This device is to have just one browser and also one of the programs below that can be set for limiting Internet access or access to certain play-related websites. Keep the work email program closed until certain times of the day set aside for doing work emails. And keep the instant messaging program closed as well. If they must instant message someone, open the program for just that short query and close it when they have gotten the reply. Don’t leave this program in the active mode while working. Software for gaming, social media, or other such time-wasters is not to be installed on this computer. Instead, they can use a tablet or even another laptop as their “play” machine. On this computer is to be installed all the entertainment and social media software they wish to use, but is to have no work-related programs or work email. By setting up two different systems, it becomes easier when using the work device to not be distracted by the availability of play, gaming, or other social media programs or personal email accounts. Advise them to never play on their “work computer” and never work on their “play computer.”
Install
Internet time-management software on the home and workplace computers.
There are now several software programs that can be
added on to Internet browsers that can be programmed to restrict Internet
access or block access to websites that are for sheer entertainment and to
which the adult with ADHD is likely to go that can interfere with work. These
programs include StayFocused and ChromeNanny for Google Chrome, WasteNoTime for Chrome and Safari, and Leech Block for Firefox. They can be set to
allow fixed times and durations for accessing certain websites, after which the
sites will be blocked. They can be programmed to limit access to certain times
during work or business hours and for specified durations. Some of these add-on
programs can also be set up so that they cannot be disabled and so that any
changes the adult tries to make to alter the settings don’t take effect until
the next day, both of which can serve to block impulsive use of the Internet
for entertainment or distraction when other work needs to be done. Note that
some of these programs only work on a specific browser so they won’t prevent
the adult with ADHD from getting out on the Internet using another browser.
If
the adult with ADHD has a Mac computer, programs including Self-Control and Anti-Social can be set up to manage Internet or website access or
even block it on any browsers on that computer. So can the program Focal
Filter. On a Mac computer, the program Time Out can be installed and
programmed to give gentle reminders to take a break at specified intervals
while an individual is on the Internet. The program Freedom, can be used
on both Mac and PC computers to shut down Internet access on that computer for
specified time periods. Of course, adults with ADHD can also use the Parental
Controls setting to give control of their website access to another caring
adult, such as a partner, coworker, or friend who can serve in the parental
role by blocking or unblocking Internet or website access. If the problem is
Internet access from a cell phone, look at programs such as Tasker and Do
Not Disturb as possible ways to limit or block Internet access to keep the
adult with ADHD from using it to waste time.
Of
course, all of these tactics can be overcome with “work arounds” if an adult
with ADHD tries hard enough to circumvent them. But the goal is to put enough
initial obstacles in the way of access or lengthy Internet use to cause the
adult with ADHD to have second thoughts about this impulsive desire to get on
the Internet, and hence will restrain themself from doing so.
Managing Health Risks
Adults
with ADHD need to pay more attention to the health and lifestyle risks likely
to come with their disorder than do most adults. Those risks were discussed in
an earlier section. Many health habits and lifestyle activities that adults
with ADHD are prone to are likely to put them at greater risk for coronary
heart disease and cancer, among other medical and dental problems (more dental
cavities, possibly more oral infections). Add to this their greater risk for
accidental injuries and one has a recipe for a life filled with preventable
misfortunes. So the adult with ADHD is going to need more assistance from
medical and health professionals who are expert in the management of these
health risks and lifestyle problem areas, such as smoking cessation programs,
dietary management, exercise regimens, etc.
Don’t
let the adult’s ADHD shorten their life expectancy because of its association
with these risk factors. This means not only helping adults with ADHD to get
their ADHD under control as much as possible, but they may also need encouragement
to pay attention to the lifestyle, nutrition, and other choices that may leave
them at greater risk of a shortened life. Here are some reminders to pass along
to the adult with ADHD to help get them started.
Develop
regular weekly exercise patterns (three-plus times per week) for increased
attention, better health, stress management, etc.
As clinicians have already
heard, regular routine physical exercise done three to four times per week, even
for just 20-30 minutes each time, is good for health. But for adults who have
ADHD, it also seems to be of particular benefit to further controlling ADHD
symptoms or compensating for them. It can also help fend off the risk for
obesity that comes with this disorder. So whether it’s running, biking,
weight-training, dance-classes, using one’s favorite gym equipment (treadmills,
elliptical trainers, stair-climbers, etc.) or some mixture of various types of
exercise, the client, more than most people, needs to be doing routine physical
exercise.
Encourage
the adult with ADHD to make an appointment for a routine physical exam with a
doctor if they have not had one in a while or never did get one as an adult.
This is a status check to see what problems or issues are developing and to try to head them off early with better preventive medical care. If they don’t have insurance or the money needed to do so, maybe a parent, sibling, or relative would cover this cost. If that is not possible, check with the local county or city hospital about getting such a physical exam through them at the county or state’s expense under such programs as Medicare or Medicaid if the adult with ADHD falls below the poverty line in income. Call the local department of social services to see if they can direct the adult with ADHD to free care clinics. Other things that clinicians and the adult with ADHD may wish to discuss with the physician:
- If
the adult with ADHD smokes tobacco and/or marijuana, get the doctor to
recommend a smoking cessation program to help them stop.
- If
the adult with ADHD drinks to excess or may be an alcoholic, ask the doctor to
enroll them in a nearby alcohol rehabilitation program, AA group (Alcoholics
Anonymous), or other such ongoing support program for recovering alcoholics.
- If
the adult with ADHD has a drug problem, ask the doctor to enroll them in a drug
detox clinic or other such local program.
Facilitate
a consult with a local dentist for the adult with ADHD to catch any developing
dental problems or diseases they may have.
If left unchecked, these could cause them to lose some or all of their teeth, require a partial or full set of dentures, lead to more extensive dental or gum surgery, or possibly even abscessed teeth. The latter has the potential to be lethal if that infection happens to enter the blood stream and attack the heart.
Strongly
encourage the adult with ADHD, if appropriate, to go on medication to treat
their ADHD.
Often times, the medical and dental risks we have identified in our research on
adults with ADHD stems from their unmanaged ADHD and the disorganizing effects
it has on their lives. Getting the client’s ADHD under control with medication
can allow them to engage in these other medical, dental, and health-related
activities with a greater chance of success. One side effect of those medicines
is that they can often result in weight loss. For an adult who is already
overweight, this is not actually a side effect but a side benefit of taking
these medications for managing ADHD.
Driving
Driving
is a serious and potentially life-threatening area of impairment for adults
with ADHD. If the adult’s ADHD is of a moderate to severe degree, clinicians
are strongly urged to have them use an ADHD medication whenever operating
a motor vehicle or heavy equipment. Other things clinicians can have them do
to improve this domain include the following:
Make
sure the medication covers as much of the waking day as possible. What is important here is greater attention to the timing of when the adult with ADHD takes their medication relative to when they are most likely to be driving. That is because clinicians want to insure that the adult with ADHD has adequate levels of medication in the blood stream at those hours, such as morning and evening commuting, late night driving for work or social occasions, etc. It is possible that earlier doses, even of extended release medicines, may have worn off to the degree that they are no longer adequately treated with medicine at these peak drive times.
If the adult with ADHD is not taking medication or refuses to and has children, suggest that the spouse or partner who does not have ADHD drive the children to their various activities. The same applies when they are out with a partner, spouse, family member, or other adult with ADHD in the same vehicle and the adult with ADHD is not medicated.
Strongly advise adults with ADHD with that absolutely NO alcohol should be consumed when they plan to operate a motor vehicle. Research shows that alcohol has a differentially greater detrimental effect on driving in an adult with ADHD than a typical adult, even at low doses. So advise the adult with ADHD to avoid alcohol use if they plan to be driving.
Substance Abuse
At least one in four adults with ADHD are likely to have a problem with excessive use, dependence, or abuse of one or more substances. As discussed earlier, the most common substances an adult with ADHD may over-use or abuse are nicotine, alcohol, and marijuana; sometimes all three. A lesser percentage of ADHD adults are likely to be using or abusing “hard” drugs, such as cocaine, heroin, methamphetamine, etc., or illegally using prescription drugs. Sometimes the client’s excessive drug use or abuse is admitted by them as part of the initial evaluation. Other times it can be inferred from the other difficulties that they may be experiencing, as well as from the reports of significant others about them. Some signs of drug abuse are typically associated with abrupt changes in patient mood, behavior, or physical appearance for which there is no obvious explanation. For instance:
If the adult with ADHD is showing excessive drowsiness, slurred speech, glassy eyes, slowed reaction time, poor motor coordination and imbalance, or even depression, clinicians might suspect they are abusing alcohol. Another possible category of abusable drugs showing such signs is prescription sedatives, such as Valium, Librium, and Seconal.
In contrast, is the adult with ADHD excessively alert? Do they have narrowed pupils, show more energy than usual, or seem “high” or manic? Or do they seem more restless, nervous, or fidgety than usual? Do they show excessive talking with pressured speech (words rush out like a fountain), have disjointed thinking, or even seem to be paranoid or hallucinating? Then consider that they may be abusing a stimulant. These include cocaine or “crack,” “speed” or methamphetamine, as well as prescription stimulants like the kind used to treat adult ADHD. Those drugs can be abused by crushing the tablets and snorting them nasally, mixing them with water and injecting them, or even by taking prescription medication in doses far larger than prescribed.
Are clinicians seeing signs of mild euphoria in the adult with ADHD, an excessively laid back or unconcerned attitude, or are they overly relaxed? Do they show racing or paranoid thoughts? Do they report odd perceptual distortions (vivid colors, acute hearing of soft sounds, etc.)? Do clinicians see them engaging in unusual smiling as if everything seems mildly ironic or funny? Then they may be abusing marijuana, hash, or THC (the main abusable ingredient in both), or heroin, morphine, or codeine.
Other signs that an adult with ADHD may be abusing drugs is an abrupt change in daily life functioning. This can include unexpected and unexplained changes in their finances, where money family members thought they had is now gone. Or maybe money they had in their wallet is missing. Have they asked to borrow money from family or friends for vague expenses or ones that don’t make much sense? Have those people reported finding bills they thought were paid that really were not, utilities threatened to be turned off, or that they are suddenly over-extended on credit cards (especially if from taking cash advances)? Look as well for changes in their work life, such as being repeatedly late for work when they previously were not (perhaps due to oversleeping), or a sudden loss of motivation to work. Or they complain they are getting calls from employers about being absent or for inappropriate things that have happened at work, or maybe even being fired. A sudden change from their normal driving patterns, increased negative consequences of driving (speeding tickets, etc.), or using their car at inappropriate times such as very late at night to meet “friends” unknown to their family or partner. Sudden declines in educational performance can also be evidence of this. Because adults with ADHD may have trouble in these domains anyway, even without abusing substances, clinicians should look for sudden changes from the usual level of functioning as a potential sign of drug use or abuse.
If adults with ADHD have such problems with excessive drug use or even abuse, they will find it harder than others abusing these drugs to quit using or abusing them. That is because ADHD creates a problem with self-control. It requires substantial self-control to detox from a substance on which someone is dependent or to which one is addicted. So even if the adult with ADHD is interested in discontinuing their abuse of a substance, it can prove quite difficult. That means they are going to need all of the support they can possibly get from others who care about them, such as you. And it also means that they may need to have their ADHD treated to help boost their self-control.
If the adult with ADHD isn’t sure that they have a drug-use problem, an initial step to consider is to help them with monitoring how often they are consuming that substance. Just keeping a calendar in which they can record the frequency of use of the substance each week can help them answer the issue of whether the frequency is too great. This will be apparent if their use of alcohol is occurring far more than is typical for most adults. Also check to see if it is being done in an uncontrolled fashion across various settings and times of day. Are they binge-drinking or binge-consuming that substance? Check to see if their behavior or daily functioning is being adversely affected, or if others have commented to them about their excess substance use. Watch to see if they are dependent on use of the substance to get through stressful situations.
Encourage cohabiting partners to help remove the substance from the home without provoking serious problems with withdrawal. If they are an alcoholic, daily user of tobacco, or of marijuana, or is clearly addicted to harder drugs, then clinicians may not be able to encourage a partner or friend to eliminate the substances from their living space so easily. They may need some medical assistance to help treat their withdrawal symptoms.
Encourage adults with ADHD to get professional assistance with their substance use problem.
If the problem is with nicotine, then clinicians or the client’s primary care physicians may be knowledgeable about area programs for quitting smoking. Those programs can provide nicotine alternatives to help while they step down from using tobacco or goes “cold turkey” from using tobacco. Sometimes other drugs may be needed to treat the symptoms associated with withdrawal from nicotine.
If the adult with ADHD has an alcohol use problem, then clinicians or the client’s primary care doctors may know the regional resources for treating alcoholics, such as Alcoholics Anonymous, or other forms of group and individual therapy. Again, the adult with ADHD may need certain medications to help quit (such as Antabuse) or to help cope with the symptoms of withdrawal. Sometimes the alcoholism is sufficiently severe to warrant a short-term (one- to two-month) stay in a residential treatment center for alcoholism or other drug use disorders. If that is the case, be sure the center understands that the they also have a dual diagnosis of adult ADHD. Also make sure that the staff is knowledgeable about treating that disorder in the context of a drug-use disorder. The presence of both disorders usually complicates the otherwise routine treatment plan for drug abuse to some degree.
If the adult with ADHD has a problem with marijuana use or abuse, then the same sorts of steps above may also help clinicians identify resources for this type of drug problem. While there are not as many resources for dealing with this type of dependency or abuse as there are for alcoholism, should clinicians be unaware of such programs they may find them by following the same advice given above: speak with a primary care doctor, call the state psychological and psychiatric associations, call university medical school psychiatry departments or university clinical psychology programs, check with county mental health centers, and use the Internet to search for resources.
If the adult with ADHD is dependent on or addicted to other, harder drugs than these, then inpatient hospitalization may be needed to help acutely treat their problem. This hospitalization can be followed by a short-term stay in a residential facility that focuses on treating this type of drug use. Most individuals who are using substances excessively, or who are abusing them, often have more than one psychiatric disorder besides the drug-use problem. Many have several, including their adult ADHD. Disorders such as anxiety, depression, bipolar disorder, personality disorders, etc. often coexist with drug-use disorders. Therefore, don’t be surprised if the adult with ADHD winds up being treated for these additional disorders alongside treatment for their drug use, and in addition to treatment for adult ADHD.
Conclusion
This
course was intended to convey basic information on the variety of
evidence-based and promising approaches to the management of adult ADHD. To do
so, it also reviewed basic information about the nature of the disorder and its
risks for impairment of patients’ life-course that are relevant to such
treatment. Besides reviewing the types of medical and non-medical treatments
often used to treat adult ADHD, this course provided some general
recommendations for compensating for the Executive Functioning deficits
associated with adult ADHD. And it provided numerous specific recommendations
to consider for the adult with ADHD on how to deal with problems in various
specific domains of major life activities, such as work, education, and driving.
In
closing, remember that while adult ADHD is a serious disorder, it is also one
that is highly treatable using a variety of science-based interventions that
can reduce its symptoms and greatly improve daily functioning. Adult ADHD does
not have to prevent one from pursuing one’s dreams and becoming a successful,
happy, well-adjusted adult, provided the disorder is properly diagnosed and
treated. And that success also depends in no small degree on the support that
adults with ADHD receive not just from loved ones but from their treating
professionals as well.
Appendix
Table 1: Available FDA-approved Treatments for ADHD |
Generic Name (Brand Name) |
Formulation and Mechanism |
Duration of Activity |
How Supplied |
Usual Absolute and (Weight-based) Dosing Range |
FDA-Approved Maximum Dose for ADHD |
MPH (Ritalin)* |
Tablet of 50:50 racemic mixture d,l-threo-MPH |
3-4 hours |
5, 10, and 20 mg tablets |
(0.3-2 mg/kg/day) |
60 mg/day |
Dex-MPH (Focalin)* |
Tablet of d-threo-MPH |
3-5 hours |
2.5, 5, and 10 mg tablets (2.5 mg Focalin equivalent to 5 mg Ritalin) |
(0.15-1 mg/kg/day) |
20 mg/day |
MPH (Methylin)* |
Tablet of 50:50 racemic mixture d,l-threo-MPH |
3-4 hours |
5, 10, and 20 mg tablets |
(0.3-2 mg/kg/day) |
60 mg/day |
MPH-SR (Ritalin-SR)* |
Wax-based matrix tablet of 50 : 50 racemic mixture d,l-threo-MPH |
3-8 hours Variable |
20 mg tablets (amount absorbed appears to vary) |
(0.3-2 mg/kg/day) |
60 mg/day |
MPH (Metadate ER)* |
Wax-based matrix tablet of 50:50 racemic mixture d,l-threo-MPH |
3-8 hours Variable |
10 and 20 mg tablets (amount absorbed appears to vary) |
(0.3-2 mg/kg/day) |
60 mg/day |
MPH (Methylin ER)* |
Hydroxypropyl methylcellulose base tablet of 50:50 racemic mixture d,l-threo-MPH; no preservatives |
8 hours |
10 and 20 mg tablets |
(0.3-2 mg/kg/day) |
60 mg/day |
2.5, 5, and 10 mg chewable tablets |
5 mg/5 ml and 10 mg/5 ml oral solution |
MPH (Ritalin LA)* |
Two types of beads give bimodal delivery (50% immediate-release and 50% delayed-release) of 50:50 racemic mixture d,l-threo-MPH |
8 hours |
20, 30, and 40 mg capsules; can be sprinkled |
(0.3-2 mg/kg/day) |
60 mg/day |
D-MPH (Focalin XR) ‡ |
Two types of beads give bimodal delivery (50% immediate-release and 50% delayed-release) of d-threo-MPH |
10-12 hours |
5, 10, 15, 20, 25, 30, 35, and 40 mg capsules |
0.15-1 mg/kg/day |
30 mg/day in youth; 40 mg/day in adults |
MPH (Metadate CD)* |
Two types of beads give bimodal delivery (30% immediate-release and 70% delayed-release) of 50:50 racemic mixture d,l-threo-MPH |
8 hours |
20 mg capsule; can be sprinkled |
(0.3-2 mg/kg/day) |
60 mg/day |
MPH (Daytrana)* |
MPH transdermal system |
12 hours (patch worn for 9 hours) |
10, 15, 20, and 30 mg patches |
0.3-2 mg/kg/day |
30 mg/day |
MPH (Concerta)* ‡ |
Osmotic pressure system delivers 50:50 racemic mixture d,l-threo-MPH |
10-12 hours |
18, 27, 36, and 54 mg caplets |
(0.3-2 mg/kg/day) |
72 mg/day |
MPH (Quillivant XR) |
Extended-release liquid |
10-12 hours |
25 mg/5 mL |
(0.3-2 mg/kg/day) |
60 mg/day |
MPH
(Jornay PM) |
12 hr. Delayed release tablet (microbeads) |
12+ hours |
20, 40, 60, 80, 100 mg |
60-80 mg |
100 mg/day |
AMPH† (Dexedrine Tablets) |
d-AMPH tablet |
4-5 hours |
5 mg tablets |
(0.15-1 mg/kg/day) |
40 mg/day |
AMPH† (Dextrostat) |
d-AMPH tablet |
4-5 hours |
5 and 10 mg tablets |
(0.15-1 mg/kg/day) |
40 mg/day |
AMPH† (Dexedrine Spansules) |
Two types of beads in a 50:50 mixture short and delayed-absorption of d-AMPH |
8 hours |
5, 10, and 15 mg capsules |
(0.15-1 mg/kg/day) |
40 mg/day |
Mixed salts of AMPH† (Adderall) |
Tablet of d,l-AMPH isomers (75% d-AMPH and 25% l-AMPH) |
4-6 hours |
5, 7.5, 10, 12.5, 15, 20, and 30 mg tablets |
(0.15-1 mg/kg/day) |
40 mg/day |
Mixed salts of AMPH*‡ (Adderall-XR) |
Two types of beads give bimodal delivery (50% immediate-release and 50% delayed-release) of 75:25 racemic mixture d,l-AMPH |
At least 8 hours (but appears to last much longer in certain patients) |
5, 10, 15, 20, 25, and 30 mg capsules; can be sprinkled |
(0.15-1 mg/kg/day) |
30 mg/day in children |
Recommended dose is 20 mg/day in adults |
Lisdexamfetamine (Vyvanase)* ‡ |
Tablets of dextroamphetamine and L-lysine |
12 hours |
30, 50, and 70 mg tablets |
|
70 mg/day |
Atomoxetine*‡ (Strattera) |
Capsule of atomoxetine |
5 hour plasma half-life but CNS effects appear to last much longer |
10, 18, 25, 40, 60, and 80 mg capsules |
1.2 mg/kg/day |
1.4 mg/kg/day or 100 mg |
Guanfacine ER** (Intuniv) |
Extended-release tablet of guanfacine |
Labelled for once-daily dosing |
1,2,3 & 4 mg tablets |
Up to 4 mg per day |
Up to 4 mg per day |
Clonidine ER**(Kapvay) |
Extended-release tablet of clonidine |
Labelled for twice-daily dosing |
0.1 mg tablet |
0.1- 0.2 mg twice daily |
Up to 0.4 mg daily |
*Approved to treat ADHD age 6 years and older.
†Approved to treat ADHD age 3 years and older.
‡Specifically approved for treatment of ADHD in adults.
** Approved to treat ADHD in youth 6-17 years old as monotherapy or as adjunctive treatment with stimulant
Updated from Prince, J. et al. (2015). Psychopharmacology for adult ADHD. In R. A. Barkley (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). New York: Guilford Press. Copyright by Guilford Press 2015. Reprinted with permission.
Table 2: The Eight Stimulant Delivery Systems |
The first five delivery systems may be thought of as the 5 Ps – pills, pumps, pellets, patches, and pro-drug. The various brand names of ADHD medicines you will hear about are either one form or another of MPH or AMP and involve one of these delivery systems:
- Pills: These are the original versions of these medicines that have been available for many decades. The first versions of AMP were discovered in the 1930s while the first version of MPH was discovered in the 1950s. In pill form, these medications are absorbed quickly, usually within 15–20 minutes after being taken by mouth. They can usually reach their peak level in the blood (and so in the brain) in 60–90 minutes, and may last 3–5 hours in controlling the symptoms of ADHD in most people. That was their problem. If you wanted to control the symptoms of ADHD across the waking day of, say, 14–16 hours for most adults, you had to give these medications 2–4 times per day or more often. The inconvenience that posed to people having to take these drugs is obvious, not to mention the fact that many had to remember to take them so often and so they frequently forgot to do so. These and other problems with these immediate-release pills led pharmaceutical companies to explore better ways to get the medicines into the body and keep them active there longer. The brand names you are likely to hear about for these pills are Ritalin® (MPH, a mixture of d-MPH and l-MPH), Focalin® (just d-MPH), Dexedrine® (d-AMP), Benzedrine® (l-AMP), and Adderall® (a mixture of the d- and l-AMP forms or salts).
- The Pump: Then came the invention of an ingenious water-pump system for delivering these drugs into the body and keeping them in the bloodstream longer. The brand name for this system is Concerta®, and it contains MPH. It is a capsule-appearing container with a small laser-drilled hole on one of its long ends. Inside, there are two chambers. One chamber contains a paste-like sludge of MPH, and the other chamber is empty. There is also powdered MPH coating the outside of the capsule. Now here is the neat part: when you swallow the capsule, the powder goes right to work just as it would in the pill form of MPH described above (i.e., Ritalin). That gives just enough time for the capsule to start to absorb water from your stomach (and later your intestines). The water is absorbed through the wall of the pump in a continuous, even flow into the empty chamber. As that chamber fills up, it presses against the other chamber that contains the MPH paste. That pressure then squeezes the MPH paste out of the hole in the capsule. It is designed to do that continuously for 8–12 hours or more. The final result is that many people, especially children, only need to take one capsule a day, and not the usual 2–3 (or more) they would have to take using the regular pills discussed above.
The capsules come in various-sized doses of course, so that physicians can adjust the dose to better suit the individual needs and responses of their ADHD patients. One problem, though, is that some older children and teens, and especially adults, may need a longer course of medication each day than what this provides. To deal with that issue, some physicians use the pills of MPH or AMP toward the end of the day. They do this to get an extra 3–5 hours of treatment with medication after the Concerta® may be losing its beneficial control of ADHD symptoms. Even so, you just have to love the human ingenuity that led to the discovery of this delivery system.
- The Pellets:At around the same time as the water-pump method was being invented, chemical (pharmacological) engineers were modifying a method that uses time-release pellets to create a way to keep medicines in the body and bloodstream longer than the pills. This method had been used for years with some cold medicines, such as the old Contac brand. But the system had to be modified in various ways for use with MPH and AMP. Now we have time-release pellets for both stimulants. Little beads of the drug are coated in such a way that some dissolve immediately after being swallowed, and others dissolve in 1, 2, 3, or more hours later. This means that the drug can be more gradually activated and absorbed into the bloodstream across 8–12 hours for most people. Here is another ingenious delivery system. It has the added advantage that someone who simply cannot or does not want to swallow the capsule that contains these pellets can open the capsule (pull it apart) and sprinkle it on a teaspoon of applesauce, yogurt, or other food and swallow it that way. It typically does not change the way the drug will work in the body.
You may have heard of these delivery systems by the brand names of Ritalin LA® (MPH), Focalin XR® (d-MPH), Medadate CD® (MPH), and Adderall XR® (AMP) here in the U.S. Again, there are different sizes (doses) to these capsules to permit a physician to adjust the dose for an individual to their optimal level. Like the water-pump method above, these time-release pellet systems sometimes are supplemented late in the day with a regular or immediate-release pill version of the same drug. That permits even longer symptom control if necessary. Both delivery systems provide good control of ADHD symptoms across the day but not at the same hours of the day. Some research exists that shows that the pellet system gives a little better control of ADHD symptoms in the morning than in the afternoon hours. In contrast, the pump system provides a bit better control in the afternoon than in morning hours. This can be an issue sometimes in deciding which delivery system may be better for someone, depending on when they need the greatest control of their ADHD symptoms during the day.
- The Patch:The next invention of a delivery system for the stimulants was FDA-approved just a few years after the pump and pellet. It is a patch with an adhesive coating that is applied directly to the skin, such as on the back of the shoulder or on the buttocks. The patch contains MPH. When applied to the skin, the MPH is absorbed through the skin and gets into the bloodstream by that means. So long as the patch is worn, MPH is being delivered into the body for that many hours during the day. Because the stimulants can cause insomnia or trouble falling asleep, the patch needs to be removed several hours before bedtime to permit the drug left in the body to be broken down and removed without adversely affecting the onset of sleep. Another problem is that 15%–20% of people experience a skin rash at the site of the patch and may need to stop using the patch for this reason.
This delivery system used to go by the brand name Daytrana® (MPH). But the patent on the device is up for sale and may be purchased by another company and renamed in the future. As with the drugs above, the patch comes in different doses to better adjust the amount of the drug to the individual.
- The Pro-Drug: In 2008, another delivery system received FDA approval, but only for use with adults with ADHD, and that system goes by the brand name of Vyvanse® (a form of AMP). Here is yet a further example of human inventiveness. One of the problems with the immediate-release pills as well as with the pellet systems is that they have the potential to be abused. That is usually done by crushing and inhaling the powder from the pills or the crushed beads from the pellet systems. That powder can also be mixed with water and injected into a vein. Whether snorted through the nose or injected into a vein, the stimulants get into the blood very quickly and so into the brain very rapidly. It is this rapid invasion of the brain by the drug, and nearly as rapid decrease in certain brain regions, that creates the “rush” or euphoria that people can experience with stimulants delivered in this fashion. This does not occur from the oral ingestion of the drug. This pro-drug was designed so that the drug cannot be activated unless it is in the human stomach or intestines. The drug is designed in such a way that the d-AMP typically lasts 10–14 hours – greatly reducing any abuse potential while providing for the desired longer course of action from a single dose.
- The Delayed Onset System: In 2019, the latest delivery system was approved, called Jornay PM, which comprises a reformulation of the drug MPH. This drug is taken at night, typically between 6:30 and 9:30 p.m., and reliably activates 12 hours later. It is approved for people 6 years of age and older. But it is anticipated that the company will likely come out with a version that uses the drug AMP and seek FDA approval for use of that variant in children and adults with ADHD sometime in the near future. This product was developed because early morning hours can be very difficult for families of children with ADHD even if those children are taking one of the other stimulant delivery systems noted above. That is because it can take up to 60–90 minutes for those medications to reach their therapeutic level – a time period that overlaps with the hours parents and children are getting ready to leave home for school and work. Hence, children with ADHD on those other systems are essentially unmedicated or undermedicated for this crucial and stressful time of the weekday morning. This delivery system solves that problem.
- Liquid Extended Release: There are now liquid versions of the extended-release forms of MPH and AMP that may be helpful when clients profess difficulties swallowing the pills or capsules that are used in these other systems above.
- Dissolvable Gel “Gummy” Systems: Another formulation of MPH uses a gel product like that seen in gummy vitamins and candy. This gel dissolves on contact with saliva in the mouth and is not affected in its pharmacological properties if chewed by the child.
|
Resources
Websites
Dr.
Barkley: russellbarkley.org, adhdlectures.com
Dr.
Barkley’s personal website containing fact sheets on ADHD, his speaking
schedule, and information about his various books and newsletter.
ADHDLectures.com contains 10 hours of lectures for parents and 25 hours for
professionals addressing various topics related to ADHD and its management, all
of which can be viewed for free.
ADD
Warehouse: addwarehouse.com
Lists
a variety of books, videos, and other products related to ADHD for sale.
American
Academy of Child & Adolescent Psychiatry: aacap.org
Official
website which also contains a separate directory of fact sheets on childhood
and adolescent mental disorders.
American
Academy of Pediatrics: aap.org
Official
website on which one can find some factual information about ADHD and other
developmental disorders.
ADDA
Organization (Attention Deficit Disorders Association): add.org
This
organization advocates for those with ADHD and has, over time, come to focus
more on adults with the disorder.
Addresources.org
A
non-profit organization dedicated to providing information on ADHD. The website
claims to host hundreds of service providers and its Information Site has a
carefully curated assortment of articles, guides and helpful tips for ADHD, not
to mention countless hours of recorded broadcasts and seminars.
ADHD
Coaching: adhdcoaches.org, totallyadd.com, nancyratey.com
Three
websites that provide information on the ADHD coaching approach to treatment
several of which contain lists of coaching professionals by region.
ADHDRollerCoaster.org
A
website created by journalist, Gina Pera, who also specializes in providing
information on ADHD for adults, especially for couples in which one partner has
adult ADHD.
CHADD
Organization (Children and Adults with ADHD): chadd.org
The
U.S. national non-profit organization dedicated to advocating for children and
adults with ADHD and their families. Contains fact sheets on ADHD, a directory
of state and local CHADD chapters, and information on its annual conferences.
Everydayhealth.com/adhd/adult-adhd.aspx
Sponsored
by Everyday Health Media, this page of this website has information on the
symptoms and treatments for ADHD. The website does accept advertisements for
products in the ADHD marketplace.
Helpguide.org
Bills
itself as a trusted non-profit guide to information on mental health and
well-being created to the memory of Morgan Segal whose suicide may have been
prevented by having better, factual information on mental health disorders and
their treatment. The website notes that it collaborates with the Harvard
Medical School concerning information posted to the site.
National
Institute of Mental Health: help4adhd.org
Co-created
with the CHADD organization (see above) this website sponsored by the U.S.
federal government offers informative and useful fact sheets about many aspects
of ADHD in children and adults.
TotallyADD.com
This
website was co-created by two Canadians, one a comedian with adult ADHD and the
other a video producer with adult ADHD, who became well-known for their
independently produced program, ADHD and Loving It, that aired on many PBS and
CBC stations several years ago. It provides a positive, light hearted, and
sometimes humorous approach to understanding ADHD in adults.
WebMD.com
This
is a for-profit website providing information on many medical and mental health
disorders including ADHD.
Books
and Videos on Adult ADHD
The
list below is not intended to be comprehensive or exhaustive but provides those
books that Dr. Barkley believes offer useful and evidence-based information on
adult ADHD.
Adler, L. (2006). Scattered Minds: Hope and help for adults with attention deficit hyperactivity disorders. G. Putnam & Sons.
Ang, A. G., Nirjar, U., Elkins, A. R., Sizemore, Y. J., Monticello, K. N., Peterson, M. K., Miller, S. A., Barone, J., Eisenlohr-Moul, T. A., & Martel, M. M. (2024). Attention-deficit/hyperactivity disorder and the menstrual cycle: Theory and evidence. Hormones and Behavior, 158, doi.org/10.1016/j.yhbeh.2023.105466
Babinski, D. E. (2024). Sex differences in ADHD: Review and priorities for future research. Current Psychiatry Reports, 26, 151-156.
Babinski, D. E., & Libsack, E. J. (2025). Adult diagnosis of ADHD in women: A mixed methods investigation. Journal of Attention Disorders, 29(3). doi.org/10.1177/1087054724129
Bailey, E. & Haupt, D. (2010). The complete idiot’s guide to adult ADHD. New York: Alpha Books (Penguin Group).
Banaschewski, T., Coghill, D. & Zuddas, A. (2018)_(Eds.), Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 94-102). Oxford University Press.
Barkley, R. A. (2001). ADHD in adults [DVD]. Guilford Press.
Barkley, R. A. (2015). Attention Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment (4th ed.). Guilford Press.
Barkley, R. A. (2016). When an Adult you Love Has ADHD: Professional Advice for Parents, Partners, and Siblings. LifeTools, American Psychological Association.
Barkley, R. A. (2020). Taking Charge of Adult ADHD (3rd ed.). Guilford Press.
Barkley, R. A., Murphy, K. R., and Fischer, M. (2008). ADHD in Adults: What the Science Says. Guilford Press.
Bramer, J. S. (1996). Succeeding in college with attention deficit hyperactivity disorders: Issues and strategies for students, counselors, and educators. Specialty Press, Inc. 300 Northwest 70th Avenue, Suite 102, Plantation, FL.
Brown, T. E. (2013). A new understanding of ADHD in children and adults: Executive function impairments. Routledge.
Brown, T. E. (2014). Smart But Stuck: Emotions in Teens and Adults with ADHD. Jossey-Bass.
CHADD (2001). The CHADD Information and Resource Guide to AD/HD. Landover, MD: CHADD (301-306-7070; chadd.org)
Faraone, S. V., Bellgrove, M. A., Brikell, I., Cortese, S., Hartman, C. A., Hollis, C., Newcorn, J. H., Philipsen, A., Polanczyk, G. V., Rubia, K., Sibley, M. H, & Buitelaar, J. K. (2024). Attention deficit/hyperactivity disorder. Nature Reviews: Disease Primers, 10(Article 11), 1-21. doi.org/10.1038/s41572-024-00495-0.
Gordon, M. & Keiser, S. (2000). Accommodations in higher education under the Americans with Disabilities Act: A no-nonsense guide for clinicians, educators, administrators, and lawyers. Guilford Press.
Gordon, M., Lewandowski, L. J., & Lovett, B. J. (2014). The assessment and management of ADHD in educational and workplace settings in the context of ADA accommodations. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). Guilford Press.
Goldstein, S. & Teeter Ellison, A. (2002). Clinician’s Guide to Adult ADHD. Academic Press.
Gordon, M., & McClure, D. (2008). The down and dirty guide to adult ADHD (2nd ed.). GSI Publications.
Hallowell, E. M., & Ratey, J. J. (1994). Driven to distraction. Pantheon.
Hallowell, E. M. & Ratey, J. J. (2005). Delivered from distraction: Getting the most out of life with attention deficit disorder. Ballentine Books.
Harper, K., & Lewis, T. ADHD symptoms can fluctuate with the menstrual cycle. Scientific American, January 8, 2025.
Jacobs, C., Wendel, I. & Cerulli, T. (2010). The everything health guide to adult ADD/ADHD: Expert advice to find the right diagnosis, evaluation and treatment. Adams Media.
Joffe, V. & Iachan, M. (2006). A day in the life of an adult with ADHD. Vera Joffe, Ph.D.
Kessler, Z. & Quinn, P. O. (2013). ADHD according to Zoe: The real deal on relationships, finding your focus, and finding your keys. New Harbinger Press.
Kohlberg, J. & Nadeau, K. (2002). ADHD-friendly ways to organize your life. Routledge.
Levrini, A. & Prevatt, F. (2012). Succeeding with adult ADHD: Daily strategies to help clinicians achieve your goals and manage your life. American Psychological Association.
Lovett, B. J., & Lewandowski, L. J. (2014). Testing accommodations for students with disabilities: Research-based practice. American Psychological Association
Matlin, T. & Solden, S. (2014). The queen of distraction: How women with ADHD can conquer chaos, find focus, and get more done. New Harbinger Publications.
Nadeau, K. (1994). Survival guide for college students with ADD or LD. Magination Press. Call the ADD Warehouse at 800-233-9273 to order.
Nadeau, K. G., & Quinn, P. (2002). Understanding women with AD/HD. Advantage.
O’Nions, E., El Baou, C., John, A., Lewer, D., Mandy, W., McKechnie, D. G. J., Petersen, I., & Stott, J. (2025). Life expectancy and years of life lost for adults diagnosed with ADHD in the UK: matched cohort study. British Journal of Psychiatry. DOI: 10.1192/bjp.2024.199
Orlov, M. (2010). The ADHD effect on marriage: Understand and rebuild your relationship in six steps. Specialty Press.
Orlov, M. & Kohlenberger, N. (2014). The couple’s guide to thriving with ADHD. Specialty Press.
Ostinelli, E. G., Schulze, M., Zangani, C., Farhat, L. C., Tomlinson, A., Del Giovane, C., Chamberlain, S. R., Philipsen, A., Young, S., Cowen, P. J., Bilbow, A., Cipriani, A., & Cortese, S. (2025). Comparative efficacy and acceptability of pharmacological, psychological, and neurostimulatory interventions for ADHD in adults: A systematic review and component network meta-analysis. The Lancet: Psychiatry, 12(1), p32-43.
Pera, G. (2008). Is it you, me, or adult ADHD? 1201 Alarm Press.
Pera, G.A. & Robin, A.L. (2015). ADHD-focused couple therapy: A clinical guide. Routledge.
Puryear, D. A. (2012). Your life can be better, using strategies for adult ADD/ADHD. Mill City Press
Ramsay, J. R., & Rothstein, A. L. (2014). Cognitive-behavioral therapy for adult ADHD: An integrative psychosocial and medical approach (2nd ed.). Taylor & Francis.
Ramsay, J. R., & Rothstein, A. L. (2014). The adult ADHD tool kit: Using CBT to facilitate coping inside and out. Routledge.
Ratey, N.A. (2002). Life coaching for adult ADHD. In S. Goldstein & A. Teeter Ellison, (Eds), Clinician's guide to adult ADHD: Assessment and intervention. Academic Press.
Ratey, N. A. (2008). The disorganized mind: Coaching your ADHD brain to take control of your time, tasks, and talents. St. Martin’s Griffin.
Safren, S. A., Otto, M., Sprich, S., Winett, C., Wilens, T., & Biederman, J. (2005). "Cognitive-behavioral therapy for ADHD in medication-treated adults with continued symptoms." Behavior Research and Therapy, 43, 831-842.
Safren, S., Perlman, C., Sprich, S., & Otto, M. W. (2005). Therapist guide to the mastery of your adult ADHD: a cognitive behavioral treatment program. Oxford University Press.
Sarkis, S. M. (2008). Making the grade with ADD: A students guide to succeeding in college with attention deficit disorder. New Harbinger Publications.
Sarkis, S. M. (2011). 10 simple solutions to adult ADD: How to overcome chronic distraction and accomplish your goals. New Harbinger Publications.
Sarkis, S. M. & Klein, K. (2009). ADD and your money: A guide to personal finance for adults with attention deficit disorder. New Harbinger Publications.
Sarkis, S. & Quinn, P. O. (2011). Adult ADD: A guide for the newly diagnosed. New Harbinger Publications.
Solden, S. (2012). Women with attention deficit disorder: Embrace your differences and transform your life (2nd ed). Underwood Books.
Solanto, M. V. (2013). Cognitive behavioral therapy for adult ADHD: Targeting executive dysfunction. Guilford Press.
Surman, C. (2012). ADHD in adults: A practice guide to evaluation and management. Humana Press.
Surman, C., Bilkey, T., & Weintraub, K. (2014). Fast minds: How to thrive if clinicians have ADHD (or think clinicians might). Berkley Trade (Penguin Group).
Thurlow, M. L., Elliott, J. L., & Ysseldyke, J. E. (2003). Testing students with disabilities: Practical strategies for complying with district and state requirements. Corwin Press.
Tuckman, A. (2007). Integrative Treatment for Adult ADHD: A Practical, Easy-to-Use Guide for Clinicians. New Harbinger Publications, Inc.
Tuckman, A. (2009). More attention, less deficit: Success strategies for adults with ADHD. Specialty Press.
Tuckman, A. (2012). Understand your brain, get more done: The ADHD executive functions workbook. Specialty Press.
Tuckman, A. (2020). ADHD after dark: Better sex life, and better relationships. Routledge.
Vater, C. H., DiSalvo, M., Biederman, J., Ehrlich, A., Parker, H., O’Connor, H., & Faraone, S. V. (2024). ADHD in adults: Does age at diagnosis matter? Journal of Attention Disorders, 28(5). doi.org/10.1177/10870547231218
Wasserstein, J., Wolf, L., & Lefever, F. (2001). Adult attention deficit disorder: Brain mechanisms and life outcomes. In the Annals of the New York Academy of Sciences, Volume 931. New York Academy of Sciences.
Weiss, M., Hechtman, L., & Weiss, G. (1999). ADHD in adulthood: A guide to current theory, diagnosis, and treatment. Johns Hopkins Press
Yang, X.. Zhang, L., Yu, J., & Wang, M. (2025). Short-term and long-term effect of nonpharmacotherapy for adults with ADHD: A systematic review and network meta-analysis. Frontiers in Psychiatry, 16. doi:10.3389/fpsyt.2025.1516878
Young, J. (2007). ADHD Grown Up: A guide to adolescent and adult ADHD. W. H. Norton.
Zhang, S. Pan, M., Zhang, L., Li, H., Zhou, M., Dong, M., Si., F., Liu, L., Wang, Y., & Qian, Q. (2025). Efficacy of internet-based cognitive behavioral therapy for medicated adults with attention-deficit/hyperactivity disorder (ADHD): A randomized controlled trial. Psychiatry Research, 344. https://doi.org/10.1016/j.psychres.2025.116352
Zylowska, L. & Siefel, D. (2012). The mindfulness prescription for adult ADHD: An 8-step program for strengthening attention, managing emotions, and achieving your goals. Westville, South Africa: Trumpeter Publishers
References
Adler, L. A., Faraone, S. V., Spencer, T. J., Berglund, P., Alperin, S., & Kessler, R. C. (2017). The structure of adult ADHD. International Journal of Methods in Psychiatric Research, 26, e1555.
American Psychiatric Association (2013). Diagnostic and Statistical Manual for Mental Disorders (5th ed.). American Psychiatric Association.
American Psychiatric Association (2022). Diagnostic and Statistical Manual for Mental Disorders (5th ed., text rev.). American Psychiatric Association.
Asherson, P. & Ramos-Quiroga, J. A. (2018). Treatment in adult ADHD. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 426-436). Oxford University Press.
Barkley, R. A. (2020). Taking Charge of Adult ADHD (3rd ed.). Guilford Press.
Barkley, R. A. (2019). Neuropsychological testing is not useful for the diagnosis of ADHD. Stop It! (or Prove It). The ADHD Report, 27, 1-8.
Barkley, R. A. (2015). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). Guilford Press.
Barkley, R. A. (2015). Etiologies. In R. A. Barkley (Ed. ). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). Guilford Press.
Barkley, R. A. (2015). Executive functioning and self-regulation as an extended phenotype: Implications of the theory for ADHD and its treatment. In Barkley, R. A. (Ed.). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed., pp. 405-434). Guilford Press.
Barkley, R. A. (2015). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). Guilford Press.
Barkley, R. A. (2015). Educational, occupational, social, and financial impairments in adults with ADHD. In Barkley, R. A. (Ed.). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). Guilford Press.
Barkley, R. A. (2015). Health problems and related impairments in children and adults with ADHD. In R. A. Barkley (Ed.). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). Guilford Press.
Barkley, R. A. (2012). Executive functions: What they are, how they work, and why they evolved. Guilford Press.
Barkley, R. A. (2012). Barkley Functional impairment scale. Guilford Press.
Barkley, R. A. (2011). Barkley deficits in executive functioning scale. Guilford Press.
Barkley, R. A. (2011). The Barkley adult ADHD rating scale – IV. Guilford Press.
Barkley, R. A. et al. (2008). ADHD in adults: What the science says. Guilford Press.
Barkley, R. A. & Fischer, M. (2018). Hyperactive child syndrome and estimated life expectancy at young adult follow-up: The role of adult ADHD and other potential predictors. Submitted for review for publication.
Barkley, R. A., Fisher, M., Smallish, L., & Fletcher, K. (2006). Young adult follow-up of hyperactive children: Adaptive functioning in major life activities. Journal of the American Academy of Child and Adolescent Psychiatry, 45, 192-202.
Barkley, R. A. & Murphy, K. R. (2010). Deficient emotional self-regulation in adults with ADHD: The relative contributions of emotional impulsiveness and ADHD symptoms to adaptive impairments in major life activities. Journal of ADHD and Related Disorders, 1(4), 5-28.
Barkley, R. A., Murphy, K. R., & Fischer, M. (2008). ADHD in adults: What the science says. Guilford Press.
Buitelaar, J. N. J., Posthumus, J. A., & Buitelaar, J. K. (2016). ADHD in childhood and/or adulthood as a risk factor for domestic violence or intimate partner violence: A systematic review. Journal of Attention Disorders, 24(9), 1203-1214. https://doi.org/10.1177/1087054715587099
Becker, S. P., Willcutt, E. G., Leopold, D. R., Fredrick, J. W., Smith, Z. R., Jacoson, L. A., Burns, G. L., Mayes, S. D., Waschbusch, D. A., Froehlich, T. E., McBurnett, K., Servera, M., & Barkley, R. A. (2022). Report of a work group on sluggish cognitive tempo: Key research directions and a consensus change in terminology to Cognitive Disengagement Hypoactivity Syndrome (CDHS). Journal of the American Academy of Child and Adolescent Psychiatry. Epub ahead of print.
Canu, W. H., Knouse, L. E., Flory, K. & Hartung, C. M. (2023). Thriving in college with ADHD: A cognitive behavioral skills approach therapist guide. Taylor & Francis Publishers.
Chronis-Tuscano, A., Wang, C. H., Woods, K. E., Strickland J., & Stein M. A. (2016). Parent ADHD and evidence-based treatment for their children: Review and directions for future research. Journal of Abnormal Child Psychology. Epub ahead of print.
Connor, D. F. (2015). Stimulant and nonstimulant medications for childhood ADHD. In R. A. Barkley (Ed.), Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 666-685). Guilford Publications.
De Crescenzo, F., Cortese, S., Adamo, N., & Janiri, L. (2017). Pharmacological and non-pharmacological treatment of adults with ADHD: a meta-review. Evidence Based Mental Health, 20, 4-11. doi: 10.1136/eb-2016-102415.
Dalsgaard, S., Leckman, J. F., Mortensen, P. B., Nielsen, H. S., & Simonson, M. (2015). Effects of drugs on the risk of injuries in children with attention deficit hyperactivity disorder: a prospective cohort study. Lancet, 385, 2190-2196.
Dalsgaard, S., Ostergaard, S. D., Leckman, J. F., Mortensen, P. B., & Pedersen, M. G. (2015). Mortality in children, adolescents and adults with attention deficit hyperactivity disorder: A nationwide cohort study. Lancet, 385, 2190-2196.
De Crescenzo, F., Cortese, S., Adamo, N. & Janiri, L. (2017). Pharmacological and non-pharmacological treatment of adults with ADHD: A meta-review. Evidence Based Mental Health, 20, 4-11. doi: 10.1136/eb-2016-102415.
Dittman, R. W., Hage, A., Pedraza, J. D., & Newcorn, J. H. (2018). Non-stimulants in the treatment of ADHD. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 393-401). Oxford University Press.
Fedewa, A. L., & Erwin, H. E. (2011). Stability balls and students with attention and hyperactivity concerns: Implications for on-task and in-seat behavior. Journal of occupational Therapy, 65, 393-399.
Field, S., Parker, D. R., Sawilowsky, S., & Rowlands, L. (2013). Assessing the impact of ADHD coaching services on university students learning skills, self-regulation, and well-being. Journal of Post-secondary Education, 26, 67-81.
Flory, K., Molina, B. S., Pelham, W. E., Jr., Gnagy, E., & Smith, B. (2006). Childhood ADHD predicts risky sexual behavior in young adulthood. Journal of Clinical Child and Adolescent Psychology, 35, 571-577.
Frodl, F. T. & Skokauskas (2012). Meta-analysis of structural MRI studies in children and adults with attention deficit hyperactivity disorder indicates treatment effects. Acta Psychiatrica Scandinavica, 125, 114-126.
Gonzalez, R. A., Kallis, C., & Coid, J. W. (2013). Adult attention deficit hyperactivity disorder and violence in the population of England: Does comorbidity matter? PlosOne, 8, e75575, 1-10.
Hechtman, L. (2020). Attention deficit hyperactivity disorder: Adult outcome and its predictors. Oxford University Press.
help4adhd.org/ living/ coaching/ WWK18, additudemag.com, nancyratey.com, adhdcoaches.org, and psychologytoday.com/ blog/pills-dont-teach-skills/201101/26-benefits-adult-adhd-coaching.
Househam, A. & Solanto, M. (2016). Mindfulness as an intervention for ADHD. The ADHD Report, 23(2), 1-5.
Hoza, B. & Smith, A. L. (2015). Is aerobic physical activity a viable management strategy for ADHD? The ADHD Report, 23(2), 1-5.
Johnston, C. & Chronis-Tuscano, A. (2015). Families and ADHD. . In R. A. Barkley (Ed.). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). Guilford Press.
Kessler, R. C., Adler, L., Barkley, R. A., Biederman, J., Conners, C. K., Demler, O., Faraone, S. V., Greenhill, L. L., Howes, M. J., Secnik, K., Spencer, T., Ustun, T. B., Walters, E. E., & Zaslavsky, A. M. (2006). The prevalence and correlates of adult ADHD in the United States: Results from the National Comorbidity Survey Replication. American Journal of Psychiatry,163, 716-723.
Knouse, L. E. (2015). Cognitive behavioral therapies for adult ADHD. In R. A. Barkley (Ed.). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). Guilford Press.
Knouse, L. E., Bagwell, C. L., Barkley, R. A., & Murphy, K. R. (2005). Accuracy of self-evaluation in adults with attention-deficit hyperactivity disorder. Journal of Attention Disorders, 8, 221-234.
Knouse, L. E. & Barkley, R. A. (2020). What’s in a (symptom example)? Exploring the Impact of DSM-5’s parenthetical additions on self-reporting of adult ADHD symptoms. Poster presentation at the annual meeting of APSARD, the American Professional Society for ADHD and Related Disorders. Washington, DC.
Knouse, L. E., Canu, W. H., Flory, K. & Hartung, C. M. (2023). Thriving in college with ADHD: A cognitive behavioral skills approach student workbook. Taylor & Francis Publishers.
Knouse, L.E. & Ramsay, J. R. (2018). Managing side effects in CBT for adult ADHD. The ADHD Report, 28(2), 6
Knouse, L. E. & Safren, S. A. (2010). Current status of cognitive behavioral therapy for adult attention-deficit hyperactivity disorder. Psychiatric Clinics of North America, 33, 497-509.
Knouse, L.E., Teller, J., Brooks, M.A. (2017). Meta-analysis of cognitive-behavioral treatments for adult ADHD. Journal of Consulting and Clinical Psychology, 85(7), 737-750.
Kooij, J. S. S. (2013). Adult ADHD: Diagnostic assessment and treatment (3rd. ed.). Springer-Verlag.
Kooij, S., Asherson, P., & Rosler, M. (2018). ADHD in adults: Assessment issues. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 307-312). Oxford University Press.
Kooij, J. J. S., Huss, M., Asherson, P., Akehurst, R., Beusterien, K., French, A., Sasane, R., & Hodgkins, P. (2012). Distinguishing comorbidity and successful management of adult ADHD. Journal of Attention Disorders, 16, 3-19.
Kubik, J. A. (2010). Efficacy of ADHD coaching for adults with ADHD. Journal of Attention Disorders, 13, 442-453.
Lasky, A. K., Weisner, T. S., Jensen, P. S., Hinshaw, S. P., Hechtman, L., Arnold, L. E., Murray, D. W., & Swanson, J. M. (2016). ADHD in context: Young adults’ reports of the impact of occupational environment on the manifestation of ADHD. Social Science & Medicine, 161, 160-168.
Li, L., Sujan, A. C., Butwicka, A., Chang, Z., Cortese, S., Quinn, P., Viktorin, A., Oberg, A. S., D’Onofrio, B. M., & Larsson, H. (2020). Associations of prescribed ADHD medication in pregnancy with pregnancy-related and offspring outcomes: A systematic review. CNS Drugs. Epub ahead of print. doi: 10.1007/s40263-020-00728-2.
London, A. S. & Landes, S. D. (2016). Attention deficit disorder and adult mortality. Preventive Medicine, 90, 8-10.
Marsh, L. E., Norvilitis, J. M., Intersoll, T. S., & Li, B. (2012). ADHD symptomatology, fear of intimacy, and sexual anxiety and behavior among college students in China and the United States. Journal of Attention Disorders. Epub ahead of print.
Mitchell, J. T., Bates, A., & Zylowska, L. (2018). Adverse events in mindfulness-based intervetions for ADHD. The ADHD Report, 28(2), 15-18.
McQuade, J., & Hoza, B. (2015). Peer relationships in children with ADHD. In Barkley, R. A. (Ed.). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). Guilford Press.
Michielsen, M., Comijs, H. C., Aartsen, M. J., Semijn, E. J., Beekman, A. T. F., Deeg, D. J. H., & Kooij, J. J. S. (2013). The relationship between ADHD and social functioning and participation in older adults in a population-based study. Journal of Attention Disorders. Epub ahead of print.
Mitchell, J. T., McIntyre, E. M., English, J. S., Dennis, M. F., Beckham, J. C., & Kollins, S. H. (2013). A pilot trial of mindfulness meditation training for ADHD in adulthood: Impact on core symptoms, executive functioning, and emotion dysregulation. Journal of Attention Disorders, Epub ahead of print.
Mohr-Jensen, C., & Steinhausen, H. C. (2016). A meta-analysis and systematic review of the risks associated with childhood attention-deficit hyperactivity disorder on long-term outcome of arrests, convictions, and incarcerations. Clinical Psychology Review, 48, 32-42.
Mongia, M. & Hechtman, L. (2012). Cognitive behavior therapy for adults with attention-deficit hyperactivity disorder: A review of recent randomized trials. Current Psychiatry Reports, 14, 561-567.
Moreno-Alcazar, A., Ramos-Quiroga, J. A., Radua, J., Salavert, J., Bosch, P. G., Salvador, R., Blanch, J., Casas, M., McKenna, P. J., & Pomarol-Clotet, E. (2016). Brain abnormalities in adults with attention deficit hyperactivity disorder revealed by voxel-based morphometry. Psychiatry Research: Neuro-imaging, 254, 41-47.
Mulraney, M., Sciberras, E., & Lecendreaux, M. (2019). ADHD and sleep. In Banaschewski, T., Coghill, D., & Zuddas, A. (2018). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 280-288). Oxford University Press.
Murphy, K. R. (2015). Psychological counseling of adults with ADHD. In R. A. Barkley (Ed.). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). Guilford Press.
Murphy, K. R., Ratey, N., Maynard, S., Sussman, S., & Wright, S. D. (2009). Coaching for ADHD. Journal of Attention Disorders, 13, 546-552.
Nigg, J. T. (2013). Attention-deficit/hyperactivity disorder and adverse health outcomes. Clinical Psychology Review, 33, 215-228.
Pera, G. A. (2008). Is it you, me, or adult A.D.D.? 1201 Alarm Press.
Pera, G. (2016). Adult ADHD-focused couple therapy. Routledge.
Pera, G.A. & Robin, A.L. (2015). ADHD-focused couple therapy: A clinical guide. Routledge.
Pera, G. (2015). Couples therapy for adult ADHD. In R. A. Barkley (Ed.). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). Guilford Press.
Polanczyk, G. V. (2018). Epidemiology. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 131-135). Oxford University Press.
Prevatt, F., & Yelland, S. (2013). An empirical evaluation of ADHD coaching in college students. Journal of Attention Disorders, 19, 666-677.
Prince, J., B., Wilens, T. E., Spencer, T. J., & Biederman, J. (2015). Psychopharmacololgy for adult ADHD. In R. A. Barkley (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). Guilford Press.
Ramsay, J. R. (2010). Nonmedication treatments for adult ADHD: Evaluating impact on daily functioning and well-being. American Psychological Association.
Ramsay, J. R. (2015). Assessment of Adult ADHD. In Barkley, R. A. (Ed.). Attention Deficit Hyperactivity Disorder: A Handbook for diagnosis and treatment (4th ed.). Guilford Press.
Ramsay, J. R. (2015). Psychological assessment of adults. Attention-Deficit Hyperactivity Disorder: A handbook for diagnosis and treatment (4th ed.) (pp.475-500). Guilford Press.
Ramsay, J. R. (2015). CBT for ADHD-Challenged Couples. In G. Pera & A. Robin (Eds.), ADHD-focused couple therapy: A clinical guide. Routledge.
Ramsay, J. R. (2017). Assessment and monitoring of treatment response in adult ADHD patients: Current perspectives. Neuropsychiatric Disease and Treatment, 13, 221-232.
Ramsay, J. R. (2020). Rethinking adult ADHD: Helping clients turn intentions into actions. American Psychological Association.
Ramsay, J. R. & Rostain, A. L. (2014). Cognitive behavioral therapy for adult ADHD: An integrative psychosocial and medical approach. Routledge.
Ratey, N.A. (2002). Life coaching for adult ADHD. In S. Goldstein & A. Teeter Ellison, (Eds), Clinician's guide to adult ADHD: Assessment and intervention. Academic Press.
Ratey, N. A. (2008). The disorganized mind: Coaching your ADHD brain to take control of your time, tasks, and talents. St. Martin’s Griffin.
Robin, A. L., & Payson, E. (2002). The impact of ADHD on marriage. The ADHD Report, 10(3), 9-11, 14.
Safren, S., Perlman, C., Sprich, S., & Otto, M. W. (2005). Therapist guide to the mastery of your adult ADHD: A cognitive behavioral treatment program. Oxford University Press.
Septier, M., Stordeur, C., Zhang, J., Delorme, R., & Cortese, S. (2019). Association between suicidal spectrum behaviors and attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. Neuroscience & Biobehavioral Reviews, 103, 109-118.
Serine, A., D., Rosenfield, B., Di Tomasso, R., Collins, J. M., Rostain, A. L., & Ramsay, J. R. (2020). The relationship between cognitive distortions and adult Attention-Deficit/Hyperactivity Disorder after accounting for comorbidities and personality traits. Cognitive Therapy and Research, Advance online publication. doi: 10.1007/s10608-020-10115-2
Solanto, M. V. (2015). Executive function deficits in adults with ADHD. In Barkley, R. A. (Ed.) Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.) (pp. 256-266). Guilford Publications.
Sonuga-Barke, E. J. S. & Cortese, S. (2018). Cognitive training approaches for ADHD: Can they be made more effective? In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 358-365.). Oxford University Press.
Spencer, T. J., Brown, A., Seidman, L. J., Valera, E. M., Makris, N., Lomedico, A., Faraone, S. V., & Biederman, J. (2013). Effect of psychostimulants on brain structure and function in ADHD: A qualitative review of magnetic resonance imaging-based neuroimaging studies. Journal of Clinical Psychiatry, 74, 902-917.
Sun, S., Kuja-Halkola, R., Faraone, S. J., D’Onofrio, B. M., Dalsgaard, S., Chang, Z., & Larsson, H. (2019). Association of psychiatric comorbidity with the risk of premature death among children and adults with attention-deficit hyperactivity disorder. JAMA Psychiatry. Epub ahead of print.
Surman, C. (2012). ADHD in adults: A practice guide to evaluation and management. Humana Press.
Tuckman, A. (2020). ADHD after dark: Better sex life, and better relationships. Routledge.
Verret, C., Guay, M., Berthiaume, C.. Gardiner, P., & Beliveau, L. (2012). A physical activity program improves behavior and cognitive functions in children with ADHD: An exploratory study. Journal of Attention Disorders, 16, 71-80.
Wakefield, J. C. (1999). Evolutionary versus prototype analyses of the concept of disorder. Journal of Abnormal Psychology, 108, 374-399.
Wymbs, B., Molina, B., Pelham, W., Cheong, J., Gnagy, E., Belendiuk, K., Walther, C., Babinski, D., & Waschbusch, D. (2012). Risk of intimate partner violence among young adults with childhood ADHD. Journal of Attention Disorders, 16, 373-383.
Young, S., Khondoker, M. Emilson, B. Sigurdsson, J. F., Wiegmann, F. P., Baldursson, G., Olafsdottir, H, & Gudjonsson, G.. (2015). Cognitive-behavioral therapy in medication-treated adults with attention-deficit/hyperactivity disorder and comorbid psychopathology: a randomized controlled trial using multi-level analysis. Psychological Medicine, 45, 2793-2804.
Zuddas, A., Banaschewski, T., Coghill, D., & Stein, M. A. (2018). ADHD treatment - psychostimulants. In Banaschewski, T., Coghill, D., & Zuddas, A. (Eds.). Oxford Textbook of Attention Deficit Hyperactivity Disorder (pp. 379-392). Oxford University Press.
Zylowska, L, Ackerman, D. L., Yang, M. H., Futrell, J. L., Horton, N. L., Hale, T. S., Pataki, C., & Smalley, S. L. (2008). Mindfulness meditation training in adults and adolescents with ADHD: A feasibility study. Journal of Attention Disorders, 1, 737-746.
Zylowska, L. & Mitchell, J. (2020). Mindfulness-Based practices for adult ADHD. Guilford Publications.
Zylowska, L. & Siefel, D. (2012). The mindfulness prescription for adult ADHD: An 8-step program for strengthening attention, managing emotions, and achieving your goals. Trumpeter Publishers.
| ©
Copyright 2004-2025 by ContinuingEdCourses.Net, Inc. All rights reserved. |


 ContinuingEdCourses.Net is approved by the American Psychological Association (APA) to sponsor continuing education for psychologists. ContinuingEdCourses.Net maintains responsibility for this program and its content.
ContinuingEdCourses.Net is approved by the American Psychological Association (APA) to sponsor continuing education for psychologists. ContinuingEdCourses.Net maintains responsibility for this program and its content. ContinuingEdCourses.Net, provider #1107, is approved as an ACE provider to offer social work continuing education by the Association of Social Work Boards (ASWB) Approved Continuing Education (ACE) program. Regulatory boards are the final authority on courses accepted for continuing education credit. ACE provider approval period: 3/9/2005-3/9/2027.
ContinuingEdCourses.Net, provider #1107, is approved as an ACE provider to offer social work continuing education by the Association of Social Work Boards (ASWB) Approved Continuing Education (ACE) program. Regulatory boards are the final authority on courses accepted for continuing education credit. ACE provider approval period: 3/9/2005-3/9/2027. ContinuingEdCourses.Net has been approved by NBCC as an Approved Continuing Education Provider, ACEP No. 6323. Programs that do not qualify for NBCC credit are clearly identified. ContinuingEdCourses.Net is solely responsible for all aspects of the programs.
ContinuingEdCourses.Net has been approved by NBCC as an Approved Continuing Education Provider, ACEP No. 6323. Programs that do not qualify for NBCC credit are clearly identified. ContinuingEdCourses.Net is solely responsible for all aspects of the programs. ContinuingEdCourses.Net is recognized by the New York State Education Department's State Board for Psychology (NYSED-PSY) as an approved provider of continuing education for licensed psychologists #PSY-0048.
ContinuingEdCourses.Net is recognized by the New York State Education Department's State Board for Psychology (NYSED-PSY) as an approved provider of continuing education for licensed psychologists #PSY-0048.